J.ophthalmol.(Ukraine).2022;6:62-64.
|
http://doi.org/10.31288/oftalmolzh202266264 Received: 07.02.2022; Accepted: 29.03.2022; Published on-line: 21.12.2022 Undiagnosed nevus of Оta, facial hemiparesis and esotropia: a case report Leopoldo Garduño-Vieyra, Raúl Rúa Martínez, Isabel de la Fuente Batta Clínica Oftalmología Garduño Irapuato, Guanajuato (México) TO CITE THIS ARTICLE: Leopoldo Garduño Vieyra, Raúl Rúa Martínez, Isabel de la Fuente Batta. Undiagnosed nevus of Оta, facial hemiparesis and esotropia: a case. J.ophthalmol.(Ukraine).2022;6:62-64. http://doi.org/10.31288/oftalmolzh202266264
Perinatal history is often underrated in ophthalmologic consultation and may provide important information in order to establish an assertive diagnosis. Purpose: To report a case of a patient who was evaluated in two hospitals as a child and misdiagnosed with Goltz syndrome. Material and Methods: it was ruled out a syndrome and the existence of three independent diagnoses was proposed: nevus of Ota, non-accommodative esotropia and left facial hemiparesis due to involvement of the VII cranial nerve. Results: A combined left eye strabismus surgery and neodymium Yag laser treatment were performed under sedation over the entire length of the nevus. Conclusion: The presence of facial palsy, strabismus or a nevus directs the physician to interrogate prenatal and perinatal issues to establish a complete diagnosis. The patient received treatment after several years and now she is satisfied. Key words: nevus, Ota, Goltz, misdiagnosed, oculodermal melanocytosis
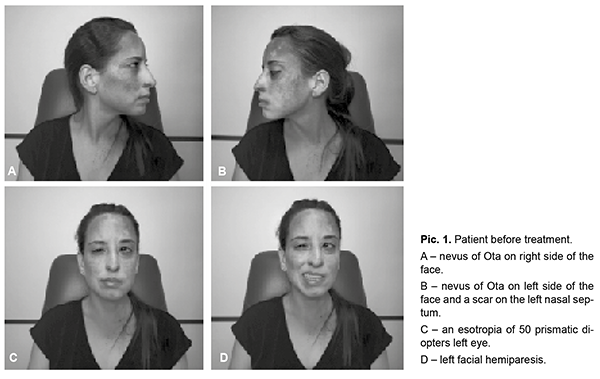
Introduction. Perinatal history is often underrated in ophthalmologic consultation. Nevertheless, an adequate interrogation of prenatal, perinatal, and postnatal issues may provide important information in order to establish an assertive diagnosis. Goltz syndrome or focal dermal hypoplasia is a rare multisystemic disease that involves the ectoderm, mesoderm, and endoderm. It is an X-linked dominant disease caused by the mutation of the PORCN gene. These patients present mainly vermiculate dermal atrophy, outpouchings of fat, telangiectasias, and hypopigmentation. They also present periorificial raspberry-like papilloma, dystrophic nails, sparse hair, abnormal teeth, split hand or foot, and ocular anomalies (microphthalmia). [1]. Three major findings of the skin/nails and one from limbs are necessary to make the clinical diagnosis. The case of a patient who was evaluated in two hospitals as a child and misdiagnosed with Goltz syndrome is described below. Sometimes when multiple findings are found on patient´s physical examination, quickly we think of a syndrome, however, there may be several diseases manifesting at the same time in the patient and not being entirely related to each other. A thorough interrogation provides the required background for medical reasoning, especially when the patient has been misdiagnosed in previous medical visits with other physicians. In this paper we substantiate this statement by describing a case of a 33-year-old woman who was misdiagnosed since childhood with Goltz syndrome, which delayed proper treatment. Case presentation A 33-year-old female patient came to the consultation to assess her refractive state due to decreased vision in the left eye. In the history, the patient refers that as a child she was evaluated in a local hospital and at two hospitals abroad and had been diagnosed with Goltz syndrome. Although the indicated examinations, skull, chest and abdomen tomography, and laboratory, were within normal limits; the doctors told her parents that the girl had a very short prognosis for life, so they did not submit her to any treatment as a child. On facial examination, dark brown nevus was observed in more than 60% of his face, left facial hemiparesis and a scar on the left nasal septum (Pic 1).
The ophthalmological examination shows a visual acuity of 20/20 in the right eye and 20/80 in the left eye. An esotropia of 50 prismatic diopters is detected in the left eye without limitation of abduction. Biomicroscopy confirms oculodermal melanocytosis. The remainder of the anterior and posterior segment examination was within normal limits. She was asked about her perinatal history and she reported that she had fetal distress due to a double round of the umbilical cord and that it was necessary to use forceps during delivery. From this it can be deduced that the poor performance of the forceps technique affected the left face, causing a lesion of the VII cranial nerve and a wound in the nasal septum. Due to all of the above, we ruled out a syndrome and the existence of three independent diagnoses was proposed: nevus of Ota (grade IV according to Tanino and grade IVb according to PUMCH),2 non-accommodative esotropia and left facial hemiparesis due to involvement of the VII cranial nerve. Then it is decided to perform treatment for the nevus of Ota and esotropia. A combined strabismus surgery and neodymium Yag laser treatment were performed under sedation over the entire length of the nevus (Pic 2). The day after surgery, the patient was in orthotropia and with a surgical red eye, the area of the nevus showed a little dryness.
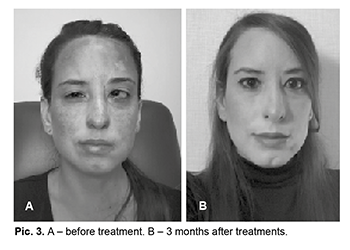
The patient was followed up with four monthly CO2 laser sessions in the nevus area. This allowed effacement of the nevus in 90% of its extension. A satisfactory result was obtained, expressed by the patient herself (Pic. 3).
Discussion The nevus of Ota was first described by Ota in 1939. It is characterized by melanocytic pigmentation that extends into the areas of the facial skin innervated by the first and second branches of the trigeminal nerve. [2]. It is a dermal melanocytic hamartoma. [3]. This pigmentation can extend to the conjunctiva, sclera, and tympanic membrane as in oculodermic melanocytosis. Pigmentation will be bluish black with gray areas and brown spots. The intensity of the pigmentation can change according to the feeling of fatigue, menstruation stage, insomnia and weather conditions. Pigmentation at the ocular level can involve the conjunctiva, sclera, cornea, iris, choroid, and less frequently the optic nerve, orbital fat, periosteum, and extraocular muscles. [2]. Nevus of Ota is more frequent in the Asian population with a prevalence of 0.02-0.08%. [3]. The predominant age of onset is at birth or immediately after. Cases of onset in adolescence are also described. It is more common in women than men at a ratio of 1 : 4.8, respectively. It generally occurs unilateraly, bilateral cases are described with a frequency of less than 5% of cases. [3]. Melanocytic lesions are a group of conditions that produce adnexal hyperpigmentation and the eyeball due to an increase in the number of melanocytes. These include the nevus of Ota (oculodermal melanocytosis). In the differential diagnosis, pigmentovascular phakomatosis, acquired bilateral nevus of Ota and nevus of Ito must be ruled out. It can also cause confusion with xeroderma pigmentosum, basal cell carcinoma and / or malignant melanoma [4]. Pigmentovascular phakomatosis is the association of an extended vascular nevus with an extensive pigmentary nevus. It is more common in women. It includes ocular and neurological disorders such as Surge-Webber syndrome and Klippel-Trenaunay syndrome and / or intracranial arteriovenous malformations [2]. Acquired bilateral nevus of Ota is a mottled or confluent brown-blue pigmentation on the patient's face. It can spread to the malar region, nose, eyelids and forehead. Pigmentation occurs bilaterally and is symmetrical. It begins and manifests itself in adulthood [2]. Ito's nevus is a congenital dermal melanosis. The nevus of Ota is similar to the nevus of Ito but located at a different site. It can be considered a variant of the Nevus of Ota, but it involves the acromioclavicular and deltoid region. The clinical, demographic and histological characteristics are similar to the nevus of Ota and even both lesions may be present in the patient at the same time [2]. Complications can occur at birth during labor, the forceps branch can give minimal skin lesions, similar to ecchymosis, but also serious with laceration-blunt wounds that need cosmetic suture, as occurred in this patient [5]. The most serious ocular complication in Nevus of Ota is the appearance of glaucoma or it becomes a malignant melanoma [6]. The treatment of choice for Nevus of Ota is laser. Treatment options were well limited before the advent of laser [2]. Initially, cryosurgery, surgical excision of the lesion, skin grafts, and dermabrasion were performed [3]. The Q-switched Nd: YAG laser is one of the most used in this type of nevus [7, 8]. This laser can also be applied in combination with the fractionated CO2 laser [2, 7, 8]. The success of the treatment is related to the frequency of the sessions received. The more sessions, the better results. This success is not related to the severity or the degree of the nevus according to the classification [3]. Conclusion Meanwhile, in adult patients, the perinatal history has been disposed from the interrogation. It may seem needless, but it can be crucial while establishing complex diagnosis. The presence of facial palsy, strabismus or a nevus directs the physician to interrogate prenatal and perinatal issues to stablish a complete diagnosis. In this case, the patient received treatment after several years, now she is satisfied.
References 1.Sibello Deustua S, Méndez Sénchez T, Naranjo Fernández RM, Estévez Miranda Y, Escobar Rodríguez G. Síndrome de Goltz. Rev Cub Oftalmo. 2016;29(4);735-40. 2.Dewi Nurasrifah IZ. Bilateral Nevus of Ota treated with combination of CO2 fractional laser and 1064 nm Nd:YAG laser. Perodical of Dermatology and Venereology 2017;29(1):81-90. 3.Nam JH, Kim HS, Choi YJ, Ho JJ, Won-Serk K. Treatment and classification of Nevus of Ota: A seven-year review of a single institution´s experience. Ann Dermatol 2017;29(4):446-53. 4.Avendaño Valdez J, Cruzado-Sánchez D. Lesiones melanocíticas en anexos oculares: melanocitosis oculodérmica, xeroderma pigmentoso y melanoma maligno. Vision Pan-America. 2010;9(4):103-6. 5.Cutrone M, Peruzzetto C. Lesiones iatrogénicas en la piel del recién nacido. Dermatol Pediatr Lat. 2006;4(1):9-18. 6.Kouba DJ, Fincher EF, Moy RL. Nevus of Ota successfully treated by fractional photothermolysis using a fractionated 1440 nm Nd:YAG laser. Arch Dermatol 2008;144(2):156-8. 7.Tokuya O, Kayoko N. The role of the CO2 laser and fractional CO2 laser in Dermatology. Laser Therapy 2014;23(1):49.60. 8.Reiko S, Takafumi O, Katsumi S, Toshio O. Usefulness of picosecond pulse alexandrite laser treatment for nevus of Ota. Laser Therapy 2018;27(4):251-5.
Information about authors and disclosure of information Corresponding author: Raúl Rúa Martínez - ruamartinez@yahoo.es Authors’ contributions: All authors contributed equally to this work Conflict of interest. The authors declare that they have no conflict of interest with this article. Ethical statement: The written informed consent was obtained from the patient.
|