J.ophthalmol.(Ukraine).2022;6:35-38.
|
http://doi.org/10.31288/oftalmolzh202263538 Received: 24.10.2022; Accepted: 10.11.2022; Published on-line: 12.12.2022 Efficacy of exenteration of the orbit and sinus in malignant tumors of the ethmoidal labyrinth F. D. Yevchev1, A. F. Yevcheva1, V. V. Gaevsky1, S. I. Poliakova2 1Odesa National Medical University 2SI “The Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine” 1Department of Otorhinolaryngology, Odesa National Medical University 2Filatov Institute of Eye Disease and Tissue Therapy, NAMS of Ukraine, Odesa E-mail: Dr.Yevchev@ukr.net Background: Diagnosing malignant tumors of the ethmoidal labyrinth early, with advanced techniques, is important, because late diagnosis may lead to intracranial spread to the eye or base of the skull. Purpose: To assess the efficacy of exenteration of the orbit and sinus in the presence of the tumor of the ethmoidal labyrinth spreading to the eye. Material and Methods: Sixty-two patients with a malignant tumor of the ethmoidal labyrinth spreading to the eye received surgery during 2017 through 2022. Of these, 42 (75.8%) were females and 20 (32.2%) were males, with patient age ranging from 55 to 75 years. Diagnostic assessment included computed tomography (CT) of the paranasal sinuses and orbit and tumor biopsy from the nasal cavity. Patients underwent a radical surgical procedure, an exenteration of the orbit and sinus. One month after surgery, they received preventive radiotherapy, with a dose of 40-45 Gy applied to the bed of the primary tumor. Results: Intraoperative course was unremarkable, and no postoperative complications were found. All the patients (100%) showed no evidence of tumor recurrence or regrowth and no metastasis over a 6-month and 3-year follow-up. Conclusion: A radical surgical procedure, an exenteration of the orbit and sinus followed by postoperative radiotherapy for a moderately differentiated tumor of the ethmoidal labyrinth spread to the orbit allowed achieving a positive treatment outcome, both in terms of local status (i.e., no tumor recurrence or regrowth) and disease process (no metastasis), over a 3-year follow-up in all the patients (100%). The decision of the extent of surgery should be made by a multispecialty team including an otorhinolaryngologist, eye cancer specialist and neurosurgeon. Keywords: tumor of the ethmoidal labyrinth, exenteration of the orbit and sinus
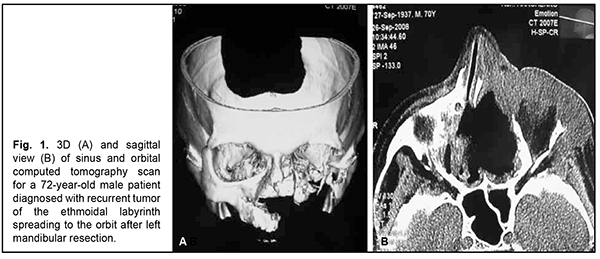
Introduction Cancer incidence is on the rise globally. In Ukraine, 160 thousand people (0.32% of the population) are diagnosed with cancer every year, and there are 100 thousand deaths [1, 2, 3]. By comparison, out of the total US population of 247 million, 50 thousand people (0.02% of the population) are diagnosed with cancer every year [1, 3, 4]. Therefore, cancer is a major medical and social problem both globally and within Ukraine. Diagnosing malignant tumors of the ethmoidal labyrinth early, with advanced techniques, is important, because late diagnosis may lead to intracranial spread to the eye or base of the skull (sinus sphenoidalis), making radical and organ-preserving surgical treatment difficult and, consequently, worsening the patient’s quality of life [1, 4, 5, 6]. When the tumor of the ethmoidal labyrinth expands to the eye, orbital tissues of the inner, superior and orbit and the orbital apex are most commonly affected, with the disease spread to the ocular adnexa (the medial angle of the eye and eyelids). It is not uncommon that the eye globe is involved into the tumor process [1, 4, 5]. The mechanism of spread of the tumor of the ethmoidal labyrinth to the orbit is implemented particularly via easy erosion of the lamina papyracea (a thin bone separating the orbital cavity from the ethmoid sinuses), with lesions affecting the orbital tissues, eye globe and ocular adnexa. In other cases the malignant tumor erodes the orbital floor. Therefore, for these cases, the surgical treatment involves exenteration of the orbit and sinus, an extended mutilating surgical procedure. The success rate of this surgical procedure in the presence of spread of the tumor of the ethmoidal labyrinth to the orbit has been reported to exceed 60% [5, 6]. Late presentation for medical care and patient’s denial of surgical treatment in the presence of an initial or limited cancer lesion are the major causes of the expansion of a malignant process and lack of efficacy of radical treatment. Thus, our previous studies have indicated that more than half of patients with tumors of the ethmoidal labyrinth presented with T3 or T4 tumor stage [1, 4]. The purpose of the study was to assess the efficacy of exenteration of the orbit and sinus in the presence of the tumor of the ethmoidal labyrinth spreading to the eye. Material and Methods Sixty-two patients with a malignant tumor of the ethmoidal labyrinth spreading to the eye received surgery at the Head and Neck Department at Odesa Municipal Clinical Hospital No. 11 during 2017 through 2022. Of these, 42 (75.8%) were females and 20 (32.2%) were males, with patient age ranging from 55 to 75 years. The primary tumor was located in the ethmoidal labyrinth in all these patients. They underwent general clinical tests, rhinoscopy of the nasal cavity, and computed tomography (CT) of the paranasal sinuses and orbit. In addition, an eye cancer specialist from the Filatov institute examined and evaluated the status of the eye to make a common decision on the extent of surgery. A preoperative biopsy was obtained from the nasal cavity tumor after anesthesia with 10% lidocaine and sent for histological examination. Forty five patients received surgery for a primary tumor of the ethmoidal labyrinth spreading to the orbit, and 17 patients, for tumor regrowth after subtotal or partial removal of a primary maxillary sinus tumor that had spread to the maxilla. Patients were proposed to undergo an exenteration of the orbit and sinus, a radical surgical procedure, due to the size of the ethmoidal labyrinth lesion invading the orbital and optic nerve, with the development of optic nerve atrophy leading to a total loss of vision; informed consent for surgery was obtained from all patients. One month after surgery, patients received preventive radiotherapy, with a dose of 40-45 Gy applied to the bed of the primary tumor. Surgery efficacy was assessed by early postoperative results (particularly, the type of postoperative cavity healing and the presence or absence of complications like purulent inflammation) and late postoperative results (particularly, the presence or absence of tumor recurrence or regrowth after subtotal or partial removal, metastatic process development) and patient’s quality of life. All patients were treated postoperatively with topical and systemic anti-inflammatory and anti-bacterial therapy (sea-buckthorn oil dressings). At day 12 after surgery, patients were discharged for outpatient treatment and follow-up. By the time of patient discharge, postoperative nasal and orbital cavities were clear and filled with granulation tissue. Patients were recommended to have furacylin ointment dressings applied to their wounds until complete epithelialization occurred. The minimum follow-up duration was 3 years, but a patient may have a life-long follow-up if requested by the patient. In addition, a patient should be followed up by an oncologist at the place of residence. Results All the 62 patients (100%) complained of difficulty with nasal breathing on the affected side, periodic nasal bleeding, loss of vision and exophthalmos. Thirty two patients (51.6%) exhibited soft tissue edema around the eye, conjunctival chemosis, difficulty with reposition of the eye, and partial or total ophthalmoplegia. Ethmoidal labyrinth and ocular lesions were more common on the left than on the right side. There was CT evidence of tumor of the ethmoidal labyrinth spreading to the orbit in all the patients (100%). Based on histological examination of tumor biopsy and postoperative material, all patients had a moderately differentiated (G2) tumor. The exenteration of the orbit and sinus had no complications (i.e., there was moderate bleeding), and the tumor was removed radically in all patients. In 40 patients (64.5%) with the tumor spread to the temporal cell tissue, the extent of surgery was expanded to include a block of affected tissues from this region. It is noteworthy that a postoperative course was satisfactory and showed no complications like purulent inflammation in all patients. Postoperative wound healing was characterized by gradual granulation tissue formation and re-epithelialization of the bone surface. No recurrence or metastatic process development was observed over a follow-up period of three years. The assessment of quality of life after exenteration of the orbit and sinus, an extended mutilating surgical procedure, showed that patients experienced stress due to a gross cosmetic defect and loss of the eye and, consequently, required psychological consultation and care, which was offered and provided on request to all patients. Figure 1 (a, b) shows CT scans of a patient with a tumor of the ethmoidal labyrinth spreading to the orbit. A 72-year-old male patient underwent a radical left maxillary sinus surgery and left maxillary resection. Nineteen months thereafter, he was diagnosed with a tumor of the ethmoidal labyrinth spreading to the orbit. After the patient underwent a complete examination and was consulted by an eye cancer specialist, he agreed to have his orbit contents removed and all his paranasal sinuses revised (Fig. 2).
Figure 3 (a, b, c, d) shows photographs of a 57-year-old male patient diagnosed with a tumor of the ethmoidal labyrinth spreading to the eye. He presented late (a year after disease onset) and had an exenteration of the orbit and sinus, an extended radical surgical procedure. A postoperative course was satisfactory in patients that underwent an extended surgical procedure. Although the state of the postoperative cavity was satisfactory, patients experienced stress due to eye removal and a cosmetic defect caused by an absence of opportunity for having prosthesis in the orbital cavity. Consequently, patients were provided psychological consultation and sessions during their rehabilitation period. Discussion Malignant tumors of the ethmoidal labyrinth, especially those spreading to the eye and brain, are very difficult to manage. In these cases, a cooperative, multispecialty approach involving an ENT surgeon, eye cancer specialist and neurosurgeon is required to make a decision on a radical extent of surgery (an exenteration of the orbit and sinus). In most patients (43 patients or 73% of the study sample), a mutilating surgical procedure of such a radical extent (an exenteration of the orbit and sinus) was required because of late presentation, i.e., they failed to present early, when the tumor of the ethmoidal labyrinth has not yet spread to the orbit. Nowadays, surgery is conducted under microscopic visual control and is followed by postoperative radiotherapy (that is, a combination treatment of surgery plus postoperative radiotherapy). Or experience in performing a radical surgical procedure, an exenteration of the orbit and sinus followed by postoperative radiotherapy for a moderately differentiated tumor of the ethmoidal labyrinth spread to the orbit allowed achieving a positive treatment outcome, both in terms of local status (i.e., no tumor recurrence or regrowth) and disease process (no metastasis), over a 3-year follow-up in all the patients (100%). The results obtained will be useful for improving the quality of surgery and patients’ quality of life, and can be considered when selecting a treatment strategy. Conclusion A radical surgical procedure, an exenteration of the orbit and sinus followed by postoperative radiotherapy for a moderately differentiated tumor of the ethmoidal labyrinth spread to the orbit tissues allowed achieving a positive treatment outcome, both in terms of local status (i.e., no tumor recurrence or regrowth) and tumor process (no metastasis), over a 3-year follow-up in all the patients. The decision of the extent of surgery should be made by a multispecialty team including an otorhinolaryngologist, eye cancer specialist and neurosurgeon.
References 1. Yevchev FD, Pukhlik SM, Gajevsky VV, et al. [Surgeon’s strategy in urgent conditions of the head, cavities of the facial skeleton and neck]. Otorynolaryngologiia. 2019;2:22. Ukrainian. 2. Fedorenko ZP, Michailovich YY, Gouldk L, et al. [Cancer in Ukraine 2017-2018. Incidence, mortality, activities of the oncological service]. BULLETIN OF the NATIONAL CANCER REGISTRY OF UKRAINE Vol. 20. National Cancer Institute of Ukraine. Kyiv; 2019. Ukrainian. 3. [Uniform clinical protocol of primary, secondary (specialized) and tertiary (highly specialized) care. Order of the Ministry of Health of Ukraine No. 246 dated 28.03.2016]. Ukrainian. 4. Kovtunenko OV, Tymchuk SM, Bakaiev AA. [Surgical treatment of advanced cancer of the maxillary sinus]. Otorynolaryngologiia. 2019;2:41. Ukrainian. 5. Benazzou S, Arkha Y, Boulaadas M, Essakalli L, KzadriM. Orbital exenteration. Rev Stomatol Chir Maxillofac. 2011 Apr;112(2):69-74. doi: 10.1016/j.stomax.2011.01.003. Epub 2011 Feb 18. PMID:21334035 French. 6. Furdova A, Babal P, Zahorjanova P, Sekac J. Subtotal Exenteration of the Orbit for Benign Orbital Disease. J Craniofac Surg. 2020 Jul-Aug; 31(5): 1367-1369.
Disclosures Received 24.10.2022 Accepted 12.12.2022 Corresponding author: Yevcheva A. F., email: esebuat11@gmail.com Author contribution: All authors participated in the conception of the article and in writing the manuscript. The final version of the manuscript has been approved by all authors, who in turn are solely responsible for submitting the final version for publication. Funding Sources: There are no external sources of funding.
Conflict of Interest Statement: The authors declare that they have no conflict of interest that could influence their opinion on the subject matter or materials described and discussed in this manuscript.
|