J.ophthalmol.(Ukraine).2022;4:62-67.
|
http://doi.org/10.31288/oftalmolzh202246267 Received: 28.04.2022; Accepted: 09.06.2022; Published on-line: 24.08.2022 Diagnostic assessment and treatment of cherubism as prevention of ocular complications R. S. Nazaryan 1, N. N. Mikhailenko 1, Yu. Yu. Yaroslavska 1, A. V. Bondarenko 1, V. V. Gargin 1, M. V. Lytvynenko 2, O. V. Artiomov 3, D. A. Oliynyk 2, T. V. Tregub 2 1 Kharkiv National Medical University; Kharkiv (Ukraine) 2 Odesa National Medical University; Odesa (Ukraine) 3 SI "The Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine"; Odesa (Ukraine) TO CITE THIS ARTICLE: Nazaryan RS, Mikhailenko NN, Yaroslavska YuYu, Bondarenko AV, Gargin VV, Lytvynenko MV, Artiomov OV, Oliynyk DA, Tregub TV. Diagnostic assessment and treatment of cherubism as prevention of ocular complications. J.ophthalmol.(Ukraine).2022;4:62-67. http://doi.org/10.31288/oftalmolzh202246267
This is an initiative study. Cherubism as a form of fibrous dysplasia of jaw bones is a congenital hereditary abnormality of osseous tissue maturation. Although the disease requires mostly maxillofacial surgery and orthodontic care, patients also have to be consulted by an ophthalmologist. The purpose of this study was to share our experience in the diagnostic assessment and treatment of cherubism, a rare form of fibrous dysplasia that is commonly misdiagnosed, which results in inadequate treatment and may lead to serious ocular complications. We present our experience of diagnostic assessment and treatment of four patients with cherubism for one to twenty years. The diagnosis of cherubism became evident after histological study of the material excised during surgery, because postoperative histology showed that changes were not cancerous (adamantinoma), but dysplastic. In addition, new foci developed or old foci recurred some time after surgery. Consequently, true jaw tumors must be correctly differentiated from dental cysts and from dysplastic bone lesions. Patients were followed up once every 6 months. Over the period of follow-up, ocular involvement was observed in the woman who had been diagnosed in childhood with congenital mixed astigmatism. Given our observations, one may make a conclusion that cherubism, a rare form of fibrous dysplasia, is a hereditary or familial disorder, and regresses after completion of puberty and puberty-related changes in hormonal milieu. Timely orthodontic care (and, if required, maxillofacial surgery care) will facilitate preventing the progression of the disease and its ophthalmological consequences. Special attention of ophthalmologists should be paid to cherubism patients with maxillary lesions. Keywords: fibrous dysplasia, cherubism, cyst-like jaw lesions, orbit
Fibrous dysplasia of facial bones is a developmental bone abnormality that arises during the embryonal period and continues developing postnatally. The disease may manifest in early childhood and adulthood. The most prominent clinical manifestations of fibrous dysplasia can be seen in symptomatic children and adolescents. This age-related activity of the disease has been attributed to the growth of skeletal bones, permanent teething, sexual maturation and rapid changes in hormonal milieu in the above periods of life [1-3]. The clinical symptoms of the disease may occur at the age of 1.5-3 years; in cherubism, symmetrical mandibular swelling (which starts at the angle region of both sides) along with excessive cheek fullness often gives rise to a typical appearance of cherub-like face [4]. Since most little children have a somewhat chubby face, the parents may not appreciate the abnormality. The disease starts progressing at the age of 8-12 years, with potential spherical swelling beginning to grow at the angle region and along the mandible on the vestibular side. The maxilla may also be affected in a similar manner, with no change in the lingual and palatine plates. Jaw pain may develop, especially at night. Painless enlargement of mobile regional lymph nodes has been noted in this period [5], with no change in the oral cavity mucosa on both sides of the alveolar processes [6]. Although the disease requires mostly maxillofacial surgery and orthodontic care, patients also have to be consulted by an ophthalmologist [7]. It is believed that, in cherubism, the mandible is the first affected, maxilla the second affected, and the orbit the last affected, with the orbital walls undergoing cystic transformation. Cystic formations involve the orbit, causing displacement of the extraocular muscles and globes, exophthalmos and diplopia [8], with bilateral cystic formation in the orbital floor being a common computer tomography (CT) finding. An anterior transcutaneous transseptal orbitotomy has been proposed to remove this defect [11]. Globe displacement may be accompanied by eyelid retraction and scleral bulging toward the inferior iris [12]. Orbital retrobulbar lesions may result in optic nerve displacement and exophthalmos [13]. The purpose of this study was to share our experience in the diagnostic assessment and treatment of cherubism, a rare form of fibrous dysplasia that is commonly misdiagnosed and not differentially diagnosed, which results in inadequate treatment and may lead to serious ocular complications. Material and Methods Four patients with cherubism (two ten-year boys, a 35-year-old mother of one of the boys, and a 45-year-old man), were involved in the study. The family history of the man was significant for a similar disease (i.e., cherubism) in his cousin. In addition, it was not known whether the woman’s relatives had the disease, but her son had a similar jaw lesion. The mother of the second boy reported no family history of jaw abnormalities. A comprehensive clinical examination, particularly of the eye, was undertaken. Patients were operated and excised samples were examined histomorphologically. Results In the female patient, the first symptoms of the disease were found when she was 9 years old. She was clinically diagnosed with adamantinoma of the left maxilla with maxillary sinus involvement, and underwent the first surgery for excohleation of the tumor focus, removal of two permanent tooth germs, and leveling of the anterior wall of the left maxilla. Over the subsequent years, she underwent six surgeries for scraping clean the cystic cavities and recurrent foci with simultaneous removal of the permanent tooth germs located in the cysts on both sides of the maxilla and the mandibular body and angles. Bone tissue was observed at the focal site. The patient received adequate prostheses. As of today, the patient has a cystic cavity at the right maxillary tuberculum which slowly decreased in size over four years without surgical involvement. The adult male patient for the first time sought medical attention at the age of 26 years. He was diagnosed with adamantinoma of the left mandible and underwent surgery with removal of the tumor and teeth (Nos. 36 and 37). At the 6-month follow-up, his pantomogram demonstrated a large cystic cavity in the region of the right mandibular angle and ramus. He underwent surgery for opening and scraping clean the focus and removing all the molars. At subsequent follow-ups over 15 years (until the patient was 40), a recurrent lesion in the region of the right angle and new maxillary body lesions and those in the sites of both maxillary turbeculi were seen. He underwent six surgical procedures totally, particularly for recurrent cyst festering in the region of the right mandibular angle. The patient received adequate prostheses. A 10-year-old boy was presented by his mother who had a similar disease. She paid attention to deformation in the oval of his face. Another boy was presented by his mother for delayed eruption of right maxillary incisors and abnormal occlusion. Eleven months before, the child underwent surgery for a cyst in the mandible, which was removed together with temporary teeth Nos. 83 and 84, and permanent tooth germs. No evidence of concomitant disease was found in any of the four patients. Physical examination of all these patients was notable for a strange phase shape with wide mandibular angles and somewhat prominent chin, with the facial shape changes being more severe in children (Figure 1).
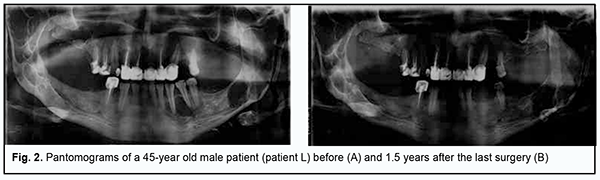
Facial skin was clear and of a normal color. Submandibular, submaxillary, submental and neck lymph nodes were not enlarged. Mandibular motility was within normal limits. The mucosa of the oral vestibule and oral cavity was moderately moist and pale pink. In the adult patients, there was anodontia of the mandible and maxilla. Prostheses were used to restore the integrity of dentitions and normal occlusion. The children had late mixed occlusion. In the adult patients, no malformation was found on palpation of the alveolar processes of the jaws at both sides. In both children, dome-shaped malformations of the vestibular lamina of the maxilla at the areas of lesions were found on palpation. In addition, in one the boys, malformation in the post-operative site on the mandible was found on palpation. Both adults underwent their last surgery 5 to 7 years before, with their pantomograms showing anodontia of the lateral mandible and maxilla. Heterogeneous bone density with poorly delineated post-operative areas of restored bone tissue prevailed. In the man, the X-ray at 1.5 years after surgery showed a well-defined cyst-like mass in the right mandibular ramus, close to the condylar neck, with the mass showing no progression compared to previous X-rays (Figure 2).
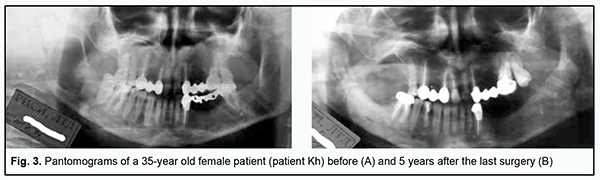
In the woman, the X-ray at 5 years after surgery showed a new bone defect in the right maxillary tuberculum. However, the cyst-like mass decreased in size by almost 50% without surgical treatment compared to the presurgical X-ray (Figure 3).
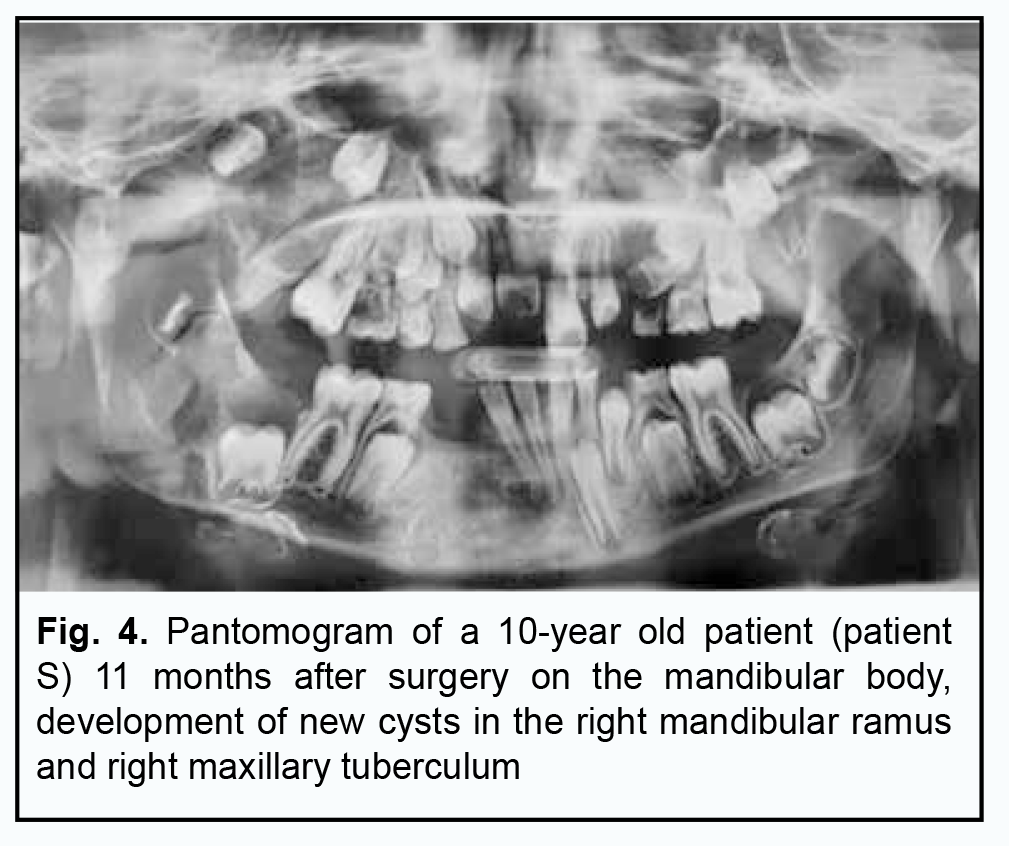
In both boys, X-rays showed cyst-like lesions containing permanent tooth germs in both jaws. One of the boys was diagnosed with adamantinoma of the mandible and underwent surgery with removal of temporary teeth 83 and 84 and tooth germs 43 and 44 enclosed in the cyst (Figure 4) at another clinic.
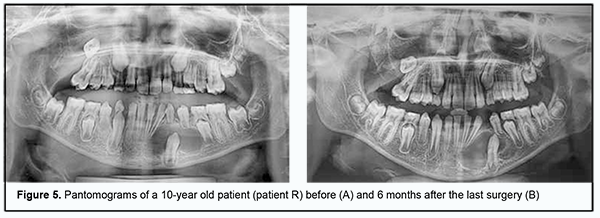
The child that was initially diagnosed at our clinic, had a cyst at tooth germ 33, and underwent cystostomy with preservation of the tooth. The wound site was covered with gauze until epithelialization was complete. The 33 erupted 6 months after surgery. The cystic cavity decreased in size by 50%, and no malformation of the mandible was observed (Figure 5).
Postoperative histopathology of excised tissue did not confirm the initial diagnosis of adamantinoma of the jaw [14]. A histological sample of the front wall of the cyst was obtained from the child that had undergone surgery at out clinic, and monomorphic fibroreticular osteogenic tissues were found and fine-fiber reactive-type tissue bars of a primitive structure without evidence of tumor atypia occurred in the sample. The changes described above are consistent with fibrous dysplasia of jaw bones. In the ophthalmological literature, reports are scarce on the description of cherubism, with the most common ocular sign of the disease being lower eyelid retraction, giving a patient the appearance of eyes looking up to the sky. A wide-spread orbital non-periosteal lesion can be accompanied by exophthalmos, diplopia, globe displacement and visual loss due to optic atrophy. All our four patients underwent a comprehensive preventive eye examination with special attention given to ocular manifestations of cherubism. They are followed up once every 6 months. After the beginning of the follow-up, ocular involvement was seen in the woman; in childhood, she had been prescribed spectacle correction for her mixed astigmatism, started wearing spectacles at the age of eight, but discontinued wearing them at the age of 12. We assessed her medical records and determined that she had had her vision reduced over subsequent five years. We found that this was associated with recurrent fibrous dysplasia of her right maxilla and sphenoidal bone. Of note, there was no apparent exophthalmos in this cherubism patient with decreased vision. A 45-year-old male driver has a preventive eye examination regularly and has no eye disease. He reported that his children also had no problems with their vision, but did not receive a comprehensive eye examination by an ophthalmologist. It is noteworthy that, of our patients with cherubism, only the female patient was found to have an eye disease, with the maxilla being more affected than the mandible. The male patient had six surgeries, and all of them were performed only on the mandible, with no cystic changes found in the maxilla. Discussion The rate of fibrous dysplasia among cases with primary benign jaw tumors has been reported to vary from 7.5% and 22%. Monostotic or polyostotic Braitsev-Lichtenstein disease, leontiasis ossea, Albright syndrome and cherubism are forms of facial bone fibrous dysplasia that differ in clinical manifestations. Cherubism is a hereditary condition, and that is why it is also named familial polycystosis or polycystic disease, familial bilateral giant-cell jaw tumor or familial fibrous dysplasia [4, 7]. Cyst-like jaw lesions varying in shape and size, surrounded by a thin osteosclerotic area, and potentially containing randomly located tooth germs, are common x-ray findings in patients with cherubism. Alteration of tooth germ development is a typical feature of cherubism [15]. Tooth germ malposition and crowding or lack of tooth germs have been observed in the disease. This may cause abnormality of eruption timing, partial anodontia, and incomplete retention of erupted permanent teeth [16, 17]. Some authors believe that the treatment of cherubism should include opening cystic cavities and cleaning them thoroughly [18, 19]. Other researchers believe that because most cases of cherubism regress spontaneously with age, operative treatment may not be necessary [20]. If, however, the focus of the cyst festers, surgical treatment is required - sometimes due to pressure from relatives – to repair the malformation of the jaw [21]. But surgical treatment is not effective in pediatric cases of the disease, as recurrences may develop. Children with the disease should be followed up for progression and require early orthodontic treatment [22]. Orbital involvement may occur after puberty and after stabilization or regression of jaw lesions. Patients with cherubism should have an eye examination by an ophthalmologist regularly [13]. It has been reported [12] that a complete ophthalmological examination revealed bilateral angioid streaks, drusen in both optic disc areas, and a subretinal neovascular membrane in the macula in a patient with cherubism. Ophthalmologic findings in this disease are primarily related to orbital bone involvement. Decreased vision was noted in one patient of this study, a woman with a maxillary lesion in the absence of exophthalmos, which is a component of the typical ocular triad (exophthalmos, strabism, and nasolacrimal duct obstruction) of cherubism. In a case of cherubism reported by Font and colleagues [23], computed tomography showed bilateral inferior lateral masses involving the orbital floors and producing marked superior displacement of the orbital contents. The intrinsic expansile bone lesions involved the inferior and lateral orbital walls with apical compression of the optic nerves. The current study and epidemiological data demonstrate [24] that cherubism symptoms manifest most prominently during the period of mixed occlusion and puberty, and are accompanied by delayed eruption or loss of permanent teeth. In this period, the enlargement of the jawbones on the vestibular side and in some cases, nocturnal jaw pain may develop. Care should be taken at the first examination of a child to pay attention to the shape of face and jaws and collect family history accurately. An adequate X-ray examination (jaw pantomography) for assessing the state of jaw bones and dentitions should be used. In addition, true tumors must be correctly differentiated from odontogenic cysts and from systemic bone lesions. A doctor treating a patient with suspected cherubism should keep in mind that only in rare cases when the cyst festers or jaw malformation is severe, surgical treatment of the disease is required. Surgical treatment should be sparing, without removing even malpositioned germs of permanent teeth and excohleation of cyst cavities to prevent the recurrence of dysplasia. Pediatric cherubism patients require orthodontic care, while adult patients, adequate prostheses, which may contribute to the prevention of ophthalmological complications. Conclusion Given the above literature data and our small-sample but long-term observations, one may make the following conclusions. Cherubism, a rare form of fibrous dysplasia, is a hereditary or familial disorder. After completion of puberty and puberty-related changes in hormonal milieu, the disease regresses, face shape normalizes to some extent, and bone tissue maturation takes place at the sites that were affected by dysplasia. Timely orthodontic (and, if required, maxillofacial surgery care), will facilitate preventing the progression of the disease and the ophthalmological sequelae that we observed in a case with affected maxilla. Consequently, patients with cherubism should be followed up not only by orthodontist and maxillofacial surgeon, but also by an ophthalmologist.
References 1.Morice A, Joly A, Ricquebourg M, et al. Cherubism as a systemic skeletal disease: evidence from an aggressive case. BMC Musculoskelet Disord. 2020;21(1):564. Published 2020 Aug 21. 2.Chrcanovic BR, Guimarães LM, Gomes CC, Gomez RS. Cherubism: a systematic literature review of clinical and molecular aspects. Int J Oral Maxillofac Surg. 2021;50(1):43-53. 3.Machado RA, Pontes H, Pires FR, et al. Clinical and genetic analysis of patients with cherubism. Oral Dis. 2017;23(8):1109-1115. 4.Argyris PP, Gopalakrishnan R, Hu Y, Reichenberger EJ, Koutlas IG. Clinicopathologic and Molecular Characteristics of Familial Cherubism with Associated Odontogenic Tumorous Proliferations. Head Neck Pathol. 2018;12(1):136-144. 5.Chen Wongworawat Y, Jack D, Inman JC, et al. Regional Lymph Node Enlargement in Clinically Severe Cherubism. ClinPathol. 2019;12:2632010X19861107. Published 2019 Jul 4. 6.Popova TM, Kryvenko LS, Tishchenko OV, Nakonechna OA, Podrigalo LV, Nessonova TD, et al. Effect of Electronic Cigarettes on Oral Microbial Flora. J Pharm Nutr Sci. 2021;11(1):54-64.Yoo SH, Pineles SL, Jarrahy R, Velez FG. Ophthalmic manifestations of cherubism. J AAPOS. 2015;19(1):70-72. 7.Carroll AL, Sullivan TJ. Orbital involvement in cherubism. Clin Exp Ophthalmol. 2001;29(1):38-40. 8.Lacorzana J, Prieto-Moreno CG. Cherubism with orbital involvement. Indian J Ophthalmol. 2020;68(11):2534. 9.Nechyporenko AS, Radutny R, Alekseeva VV, Titova G, Gargin V. Complex Automatic Determination of Morphological Parameters for Bone Tissue in Human Paranasal Sinuses. Open Bioinformatics J. 2021;14(1):130-137. 10.Radutniy R, Nechyporenko A, Alekseeva V, Titova G, Bibik D, Gargin VV. Automated measurement of bone thickness on SCT sections and other images. In: Proceedings of the 2020 IEEE 3rd International Conference on Data Stream Mining and Processing, DSMP 2020; 2020. p. 222-6. 11.Ahmadi AJ, Pirinjian GE, Sires BS. Optic neuropathy and macular chorioretinal folds caused by orbital cherubism. Arch Ophthalmol. 2003;121(4):570-573. 12.Mello LGM, Saraiva FP, Monteiro MLR. Angioid streaks and optic disc drusen in cherubism: a case report. Arq Bras Oftalmol. 2020;83(6):535-537. 13.Colombo F, Cursiefen C, Neukam FW, Holbach LM. Orbital involvement in cherubism. Ophthalmology. 2001;108(10):1884-1888. 14.Gargin V, Radutny R, Titova G, Bibik D, Kirichenko A, Bazhenov O. Application of the computer vision system for evaluation of pathomorphological images. 2020 IEEE 40th International Conference on Electronics and Nanotechnology, ELNANO 2020 - Proceedings; 2020. 469-473, 15.Nechyporenko AS, Reshetnik VM, Alekseeva VV, Yurevych NO, Nazaryan RS, Gargin VV. Implementation and analysis of uncertainty of measurement results for lower walls of maxillary and frontal sinuses. In: 2020 IEEE 40th International Conference on Electronics and Nanotechnology, ELNANO 2020 - Proceedings; 20202020. p. 460-3. 16.Nechyporenko A, Reshetnik V, Shyian D, Alekseeva V, Radutny R, Gargin V. Solutions to the 3d model problem of pressure measurement in the area of maxillary sinus anastomosis. In: CEUR Workshop Proceedings [Internet]; 20202020. p. 275-84. 17.Palamar OI, Lukach EV, Maletskyi AP, Poliakova SI, Kravets OV, Serezhko YO, et al. Clinical, morphological, CT and MRI characteristics of anterior skull base and orbital tumors. Oftalmol Zh. 2020(5):62-74. 18.Son JH, Marshall DC, Valiathan M, et al. Innovative Surgical Treatment of Severe Cherubism. Cleft Palate Craniofac J. 2019;56(1):90-93. 19.Bobrova NF, Umanets MM, Dembovetska GM, Bratishko AI. Reconstructive duet in a pole-to-pole surgery for ocular trauma: A pediatric case study. Oftalmol Zh. 2021;90(2):55-60. 20.Mirmohammadsadeghi A, Eshraghi B, Shahsanaei A, Assari R. Cherubism: report of three cases and literature review. Orbit. 2015;34(1):33-37. 21.Lyndin M, Gluschenko N, Sikora V, et al. Morphofunctional features of articular cartilage structure. Folia Med Cracov. 2019;59(3):81-93. 22.Kuzenko Y, Mykhno O, Sikora V, Bida V, Bida O. Dental terminology "discoloration" or "pigment dystrophy" - a review and practical recommendations. Pol Merkur Lekarski. 2022;50(295):65-67. 23.Font RL, Blanco G, Soparkar CN, Patrinely JR, Ostrowski ML. Giant cell reparative granuloma of the orbit associated with cherubism. Ophthalmology. 2003;110(9):1846-1849. 24.Polyvianna Y, Chumachenko D, Chumachenko T. Computer aided system of time series analysis methods for forecasting the epidemics outbreaks. 2019 15th International Conference on the Experience of Designing and Application of CAD Systems, CADSM 2019:1-4.
Disclosures Conflict of Interest: The authors declare that there is no conflict of interest that could influence their opinion regarding the subject or materials of this manuscript. Sources of Support: none.
|