J.ophthalmol.(Ukraine).2022;1:20-23.
|
http://doi.org/10.31288/oftalmolzh202212023 Received: 16 November 2021; Published on-line: 15 March 2022 Study of Prevalence of Preoperative Corneal Astigmatism in Patients with Senile Cataract at a Tertiary Care Institute in South India C. Kumar Amruth , P. Ramya Deepthi, K. Sushma Narayana Medical College and Hospitals; Nellore, Andhra Pradesh (India) TO CITE THIS ARTICLE: Kumar Amruth C., Ramya Deepthi P., Sushma K. Study of Prevalence of Preoperative Corneal Astigmatism in Patients with Senile Cataract at a Tertiary Care Institute in South India. J.ophthalmol.(Ukraine).2022;1:20-3. http://doi.org/10.31288/oftalmolzh202212023 Background. The prevalence of corneal astigmatism in patients with cataract has not been well documented in both rural and urban areas of Indian population. Purpose. The aim of this study was to assess prevalence of corneal astigmatism before cataract surgery in adult age group population of rural Andhra Pradesh. Materials and methods. A Prospective, cross-sectional, and observational study was carried out from March 2019 to December 2019 in patients presenting for cataract surgery. Axial length, and intraocular lens power were measured, Keratometric values were measured with an auto refractokeratometer, and astigmatism was calculated. Data was analysed using SPSS software. Results. This study included 1000 eyes of 1000 patients with a mean age of 61.81 ± 8.94 years. The mean astigmatism was 0.80 ± 0.72 D and the mean keratometry was 44.12D ± 1.71 D. A total of less than 1D astigmatism is seen in 67.5% eyes, 23.3% eyes had astigmatism between 1.00 and 1.99 D, 4.6% eyes had 2-2.99D, and ≥3D in 0.8% eyes and no astigmatism in 3.8% eyes. Against the rule astigmatism was seen in 49.8% cases, with the rule astigmatism is found in 31.8% of eyes and oblique astigmatism in 14.9% of eyes. With the increasing age, the WTR percentage decreased while the ATR percentage increased. Conclusion. Our study showed that significant numbers of patients have preoperative corneal astigmatism, affecting the quality of vision after cataract surgery. Majority of patients have corneal astigmatism < 1.00D, which can be corrected by low-cost procedures like steep axis phaco, limbal relaxing incisions, and opposite clear corneal incisions, especially in developing countries like India, and less percentage of candidates require expensive toric IOLs. Кey words: сorneal astigmatism, cataract, keratometry, intraocular lens
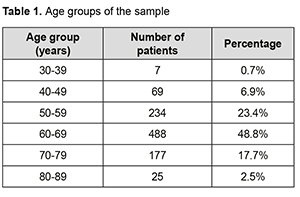
Introduction. Cataract is the most common cause of reversible blindness, and cataract surgery is the most common ocular surgery performed globally with a high rate of success and rapid anatomical and functional visual recovery [1]. With technological advancements and newer intraocular lenses, patients are expecting the best visual outcome even without glasses. To achieve this, both spherical refractive error and astigmatism must be corrected during surgery. With the advanced IOL power calculators, the incidence of spherical refractive errors is significantly reduced [2, 3]. The remaining cause of postoperative blurring of vision is astigmatism, which should be dealt with to achieve the best visual outcome. Astigmatism may be due to cornea or lens. As the lens is removed during cataract surgery, the remaining corneal astigmatism should be addressed. Corneal astigmatism includes pre-existing corneal astigmatism and surgical induced astigmatism, which depends on the incision size and location. With the advent of surgeries with small incisions like phaco and MICS, surgical-induced astigmatism has been overcome successfully [4]. Pre-existing corneal astigmatism is an important limiting factor for optimal results of cataract surgery in a significant number of patients. Pre-existing corneal astigmatism is corrected by limbal relaxing incisions (LRI’s) [5] or opposite clear corneal incisions (astigmatic keratotomy) [6] or excimer laser refractive procedures [7] or femtosecond laser-assisted astigmatic keratotomy [8] or by implanting toric IOLS during surgery [9-13]. For this to be done, a preoperative assessment of corneal astigmatism is essential. Data of prevalence of astigmatism in rural and urban population of Andhra Pradesh are lacking who are presenting for cataract surgery. Hence, this present study was designed to determine the prevalence of corneal astigmatism in populations of adult age groups presented for cataract surgery, which helps the surgeon in planning the surgery and IOL manufacturers to predict patient requirements. Materials and methods It is a prospective, cross-sectional, and observational study performed for 10 months duration from March 2019 to December 2019 in tertiary care centre (Narayana medical college hospital, Nellore) serving rural population in Andhra Pradesh, India. Informed consent was obtained from all patients, and the ethical committee of the hospital approved the study. Inclusion criteria is the patients between the age of 30-90 yrs. posted for cataract surgery. Exclusion criteria was patients with history of contact lens usage, corneal opacities and degenerations, pterygium encroaching the cornea, inflammatory diseases of the eye, history of traumatic cataract, any lid abnormalities or ptosis, and past history of ocular surgeries. In our study, we included 1000 eyes of 1000 patients. All the patients underwent complete ocular examination, which included best-corrected visual acuity assessment, slit lamp examination, tonometry, and fundoscopy. Keratometry readings were taken using the PRK-1000 auto ref-keratometer by a single investigator as a part of the preoperative biometric assessment. The measurements were carried out at least three times for each eye, and average k1 and k2 were taken. Astigmatism was calculated from the dioptric difference of vertical and horizontal readings. Corneal astigmatism was characterized as with the rule (WTR) when meridian of maximum curvature was within 30 degree of vertical 90 degree [90 degree±30 degree] or against the rule (ATR) when meridian of maximum curvature was within 30 degree of horizontal 180 degree [180 degree±30 degree] and oblique if it was neither WRT nor ATR astigmatism. Analysis: Data collected include the age, sex of the patient, type of cataract, keratometry readings in diopters, and astigmatism in diopters. Chi-square test and t test were used for categorical and continuous variables, respectively. Values are expressed as (mean ± standard deviation) and % if appropriate. The data is analysed with SPSS Statistics version 25 (SPSS Inc, Chicago, IL). A P value <0.05 was considered statistically significant. Results Patient demographics: A total of 1000 eyes of 1000 patients were examined, of which 473 were male, and 527 were female with a sex ratio of 1 : 1.11 (473 : 527). The mean age of the subjects was 61.81±8.64 years (range is 30-88 years). Patients were divided into six groups depending upon their age. Majority of patients were in the seventh decade, followed by the sixth and eighth decade (Table 1).
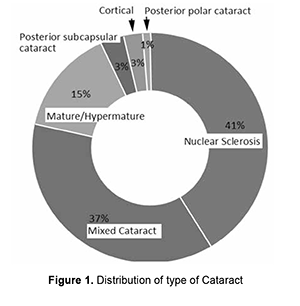
Nuclear sclerosis was present in 41.4% of eyes, mixed cataract in 36.9%, mature/hyper mature cataract in 14.9%, posterior subcapsular cataract in 3.2%, cortical in 2.6%, and posterior polar cataract in 1% of eyes (Figure 1).
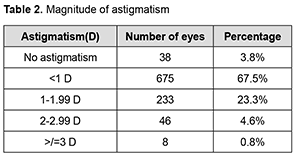
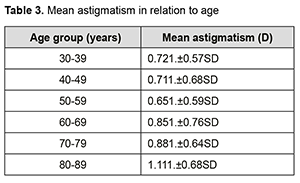
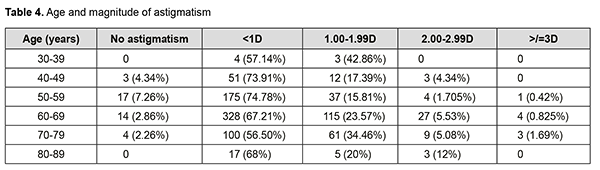
There was no astigmatism in 3.8% of eyes. With the rule, astigmatism was found in 318 (31.8%) eyes against the rule astigmatism was found in 498(49.8%) eyes and oblique astigmatism in 149(14.9%) eyes. With the increasing age, the WTR percentage decreased while the ATR percentage increased. The Mean keratometry was 44.12 ± 1.71D with 38.8 – 52 D range. The mean astigmatism was 0.80D ± 0.72 (mean±SD) ranging from 0 -6.25D. Patients were classified depending upon the magnitude of astigmatism. Mean astigmatism in relation to age was calculated by totalling the amount of astigmatism in each group and dividing the sum by the number of patients in that group. It is revealed that astigmatism less than 1D is the most common astigmatism in all age groups. However, the percentage of higher astigmatism was higher in extreme age groups. (Table 3).
Discussion This study was made to determine the prevalence of corneal astigmatism in patients posted for cataract surgery and to study the distribution and type of corneal astigmatism. There was scarcity of studies in India on preoperative corneal astigmatism except few [14, 15, 16], of which some have less sample size, and some are done in other parts of India. The mean age of our study was 60.8+8.64 years, which is similar to studies by Isyaku M. et al. (60.8+12.7) [17], Prasher et al. (59.54+10.96) [14] and Moulick et al. (60.10+10.46) [16]. The mean age is higher in studies by Xiayong Yuan et al. (69.80) [18], Khan et al. (75.54) [19], De Bernado et al. (71.89) [20]. Most of the patients in the study were in the 7th decade (48%), followed by the 6th decade (23%), similar to Venkateshwara Rao et al. Study [15]. It was different from Xiayong Yuan et al. study in which most of the patients were in the 8th decade (36%) followed by the 7th decade (26%) [18]. Our study had more female patients (527) than male patients (473) like in studies by Venkateshwara Rao et al. [15], Chaudary M et al. [21], and Xiayong Yuan et al. [18], whereas studies by Moulick et al. [16] and Isyaku M et al. [17] had more male patients. Regarding the type of astigmatism, ATR (49.5%) is found to be more prevalent than the WTR (31.8%), which is similar to other studies by Venkateshwara Rao et al. [15], Moulick et al. [16], Pascher et al. [14], and Xiayong Yuan et al. [18]. In contrast, WTR was more common in the study by Chaudary et al. [21] In our study, the percentage of ATR increased with age, as found in all other studies [14-21]. Analysis of our study data showed that mean corneal astigmatism was 0.80+0.72D(0-6.25D), which similar to Moulick et al., 0.80+0.61) [16] and Chaudary et al (0.84+0.80) [21] studies. It was higher in studies by Isyaku M et al. (1.16) [17], Xiayong Yuan et al. (1.15) [18], and Khan et al. (1.03) [19]. This may be due to the differences in the ethnicities and races, and these studies had more elderly population. The study by Prasher et al. done in North India also had higher values [14]. It may be due to the racial differences between South India and North India. In this study, mean astigmatism decreased up to the 6th decade and then increased, which concludes that mean astigmatism is higher in extreme age groups. This is similar to the Moulick et al. Study [16]. Mean age is higher is due to late presentation of patients for cataract surgery and Socioeconomic status within the rural population. In our study in most patients (67.5%) astigmatism was <1D, in 23.3% between 1-1.99D, 4.6% had between 2-2.99D, 0.8% had >3D and 3.8% had no astigmatism. It is similar to studies by Moulick et al (<1.25D- 63.5%,>1.25D – 18.8%, 0 – 0.25D – 17.8%) and Chaudary et al (<0.25D -17%, 0.25- 1.5D - 65%,>1.5D - 18%) [16,21]. Whereas, study by Rajesh Subhash and Sonali Arun found that 17.9% eyes had astigmatism from 1.0 - 1.49 D, 3.4% had astigmatism between 2.00 - 2.5 D, and 20 eyes had astigmatism >3 D, overall 32.5%eyes had astigmatism >1.00 D.[22] In Isyaku M study most patients (45.92%) had astigmatism between 1-1.99D [17]. Percentage of patients with astigmatism <1D was less in studies by Xiayong Yuan et al (53.30), Prasher et al (59.37%) and Venkateshwara Rao et al(58.15%) [14,15,18]. Current study limitations include we measured only the anterior corneal astigmatism and leaving posterior corneal astigmatism. This underestimates total astigmatism by 0.25-0.50D. We used an automated ref-keratometer for keratometry readings. Using computerized topography would have been better as it is the gold standard. Conclusion Significant numbers of patients have preoperative corneal astigmatism, affecting the quality of vision after cataract surgery. The percentage of WTR astigmatism decreases with age, and ATR astigmatism increases with age. There is a need to correct corneal astigmatism for best visual results and patient satisfaction after cataract surgery. Majority of patients have corneal astigmatism < 1.00D, which can be corrected by low-cost procedures like steep axis phaco, limbal relaxing incisions, and opposite clear corneal incisions and a lower percentage of candidates require expensive toric IOLs. So in developing countries like India, surgeons can plan for these surgical steps than going for toric IOLs. Hence, study provides information about the characteristics of corneal astigmatism in the Indian population, which will help improve surgical techniques and visual outcomes and design toric IOLS.
References 1.Lindstrom R. Thoughts on cataract surgery: 2015. Rev Ophthalmol. 2015 Mar 9 2.Olsen T. Improved accuracy of intraocular lens power calculation with the Zeiss IOLMaster. Acta Ophthalmologica Scandinavica. 2007 Feb;85(1):84-7. 3.Narváez J, Zimmerman G, Stulting RD, Chang. DH. Accuracy of intraocular lens power prediction using the Hoffer Q, Holladay 1, Holladay 2, and SRK/T formulas. Journal of Cataract & Refractive Surgery. 2006 Dec 1;32(12):2050-3. 4.Harakuni U, Bubanale S, Smitha KS, Tenagi AL, Kshama KK, Meena A, Kathyayini SV, Biala A. Comparison of surgically induced astigmatism with small incision cataract surgery and phacoemulsification. JEMDS. 2015 Sep 3;4(71):12354-60. 5.Monaco G, Scialdone A. Long-term outcomes of limbal relaxing incisions during cataract surgery: aberrometric analysis. Clinical ophthalmology (Auckland, NZ). 2015; 9:15A81. 6.Qammar A, Mullaney P. Paired opposite clear corneal incisions to correct pre-existing astigmatism in cataract patients. Journal of Cataract & Refractive Surgery. 2005 Jun 1;31(6):1167-70. 7.Norouzi H, Rahmati-Kamel M. Laser in situ keratomileusis for correction of induced astigmatism from cataract surgery. Journal of Refractive Surgery. 2003 Jul 1;19(4):416-24. 8.Kim P, Sutton GL, Rootman DS. Applications of the femtosecond laser in corneal refractive surgery. Current opinion in ophthalmology. 2011 Jul 1;22(4):238-44. 9.Mohammad-Rabei H, Mohammad-Rabei E, Espandar G, Javadi MA, Jafarinasab MR, Hashemian SJ, Feizi S. Three methods for correction of astigmatism during phacoemulsification. Journal of ophthalmic & vision research. 2016 Apr;11(2):162. 10.Lee YC. Astigmatism considerations in cataract surgery. Tzu Chi Medical Journal. 2013 Mar 1;25(1):19-22. 11.Khokhar S, Lohiya P, Murugiesan V, Panda A. Corneal astigmatism correction with opposite clear corneal incisions or single clear corneal incisions: comparative analysis. Journal of Cataract & Refractive Surgery. 2006 Sep 1;32(9):1432-7. 12.Mendicute J, Irigoyen C, Ruiz M, Illarramendi I, Ferrer-Blasco T, Montés-Micó R. Toric intraocular lens versus opposite clear corneal incisions to correct astigmatism in eyes having cataract surgery. Journal of Cataract & Refractive Surgery. 2009 Mar 1;35(3):451-8. 13.Bachernegg A, Rückl T, Riha W, Grabner G, Dexl AK. Rotational stability and visual outcome after implantation of a new toric intraocular lens for the correction of corneal astigmatism during cataract surgery. Journal of Cataract & Refractive Surgery. 2013 Sep 1;39(9):1390-8. 14.Prasher P, Sandhu JS. Prevalence of corneal astigmatism before cataract surgery in Indian population. International ophthalmology. 2017 Jun 1;37(3):683-9. 15.Venkateswara R.H., Hanumantha R. G., Sivacharan K. J. N., Anitha Devi Boyapati. "Preoperative Corneal Astigmatism in Patients with Cataract". Journal of Evidence based Medicine and Healthcare; Volume 2, Issue 29, July 20, 2015; Page: 4278-4283 16.Moulick PS, Kalra D, Sati A, Gupta S, Khan MA, Singh A. Prevalence of corneal astigmatism before cataract surgery in Western Indian Population. Medical Journal Armed Forces India. 2018 Jan 1;74(1):18-21. 17.Isyaku M, Ali SA, Hassan S. Preoperative corneal astigmatism among adult patients with cataract in Northern Nigeria. Indian J Ophthalmol. 2014; 62:1094-5 18.Yuan X, Song H, Peng G, Hua X, Tang X. Prevalence of corneal astigmatism in patients before cataract surgery in Northern China. Journal of ophthalmology. 2014;2014. 19.Khan MI, Muhtaseb M. Prevalence of corneal astigmatism in patients having routine cataract surgery at a teaching hospital in the United Kingdom. Journal of Cataract & Refractive Surgery. 2011 Oct 1;37(10):1751-5. 20.De Bernardo M., Zeppa L., Cennamo M., Iaccarino S., Rosa N. Prevalence of corneal astigmatism before cataract surgery in Caucasian patients, European Journal of Ophthalmology, 2013 21.Chaudhary M., Dahal HN, Prevalence and types of corneal astigmatism in patients undergoing cataract surgery. Journal of Institute of Medicine. 2017 Apr 1;39(1). 22.Joshi Rajesh Subhash, Jadhav, Sonali Arun. Frequency of Corneal Astigmatism in Patients Presenting for Senile Cataract Surgery at a Teaching Hospital in Indian Rural Population. Asia-Pacific Journal of Ophthalmology: March-April 2020; 9(2):126-129.
The authors declare no conflict of interest
|