J.ophthalmol.(Ukraine).2020;6:3-7.
|
http://doi.org/10.31288/oftalmolzh2020637 Received: 09 July 2020; Published on-line: 21 December 2020 Results of retinotomy for retinal detachment with marked proliferative vitreoretinopathy I. Ia. Novytskyy, R. M. Smal, O. Iu. Plevachuk, Ia. V. Andriiuk Oculus Eye Clinic; Lviv (Ukraine) E-mail: Inovytskyy@gmail.com TO CITE THIS ARTICLE: Novytskyy IIa, Smal RM, Plevachuk OIu, Andriiuk IaV. Results of retinotomy for retinal detachment with marked proliferative vitreoretinopathy. J.ophthalmol.(Ukraine).2020;6:3-7.http://doi.org/10.31288/oftalmolzh2020637 Background: Indications for retinotomy, its procedure and efficacy are still a subject for study and discussions. Purpose: To examine the efficacy of relaxing circumferential and radial retinotomies for retinal detachment associated with marked proliferative vitreoretinopathy (PVR). Material and Methods: Twenty-seven patients (27 eyes) with retinal detachment associated with PVR were involved in the study. Eleven eyes (40%) had retinotomy of less than 90°, eight (30%), of 90° to 180°, four (15%), of 180° to 270°, and four (15%), 360° (circumferential retinotomy). Additional radial retinotomy was performed in 5 eyes (19%), and retinotomy combined with choroidectomy, in 2 eyes. Results: Of the 27 eyes, retinal reattachment was achieved after the first surgery in 20 eyes (74%), after re-surgery in 5 eyes (19%). Anatomical success was achieved after removal of silicone oil in 15 eyes (56%). By the time of analysis, silicone oil was not removed in 12 eyes (44%). Complete retinal re-attachment was achieved in 25 eyes (93%), and partial re-attachment, in 2 eyes (7%). Conclusion: Retinotomy should be performed in eyes with retinal detachment and contraction. Circumferential and radial retinotomies provide a relatively high rate of anatomical success of surgery. Keywords: retinal detachment, proliferative vitreoretinopathy, closed vitrectomy, retinotomy, retinal re-attachment
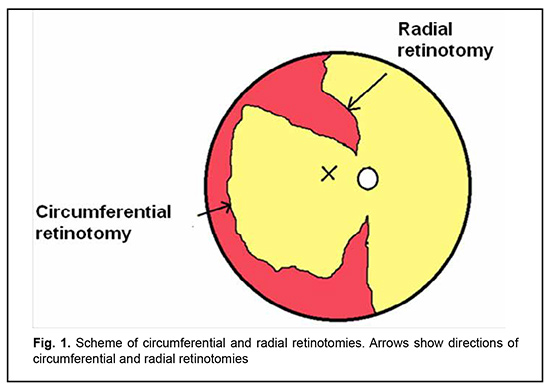
Introduction The most common cause of failure of retinal reattachment surgery is proliferative vitreoretinopathy (PVR) leading to retinal contraction and traction, when the area of the detached retina surface is not large enough for reattachment to the retinal pigment epithelium (RPE). Radial retinal contraction is more common, but it is not uncommon that marked PVR results in circumferential retinal contraction as well. This is caused by PVR, particularly, in inferior retinal detachment, following penetrating injury with retinal incarceration, and following combined rhegmatogenous and traction detachment in diabetic PVR. Membrane removal is not always enough to ensure complete traction removal. In such cases, retinotomy and/or retinoectomy should be performed to achieve retinal reattachment. Machemer described retinotomy in 1979 [1] and defined indications for it. However, indications for retinotomy, its procedure and efficacy are still a subject for study and discussions. The purpose of the study was to examine the efficacy of relaxing circumferential and radial retinotomy for retinal detachment with marked PVR. Material and Methods Twenty-seven patients (27 eyes) with retinal detachment associated with PVR (grade Cp or Ca) were under our observation. PVR was graded according to the updated Retina Society Classification, of 1991 [2]. Of these patients, 13 were men and 14 were women. The mean age was 59.8 ± 12.3 years (range, 32 to 82 years). Retinal detachment was due to ocular contusion (n=1) and penetrating injury with intraocular foreign body (n=1). In addition, one case had lens luxation following ocular contusion. Ocular comorbidities included uveitis (n=1), high myopia (n=2), a Fuchs spot (n=1), macular hole (n=3), and age-related macular degeneration (n=1). Seventeen eyes were phakic, 8 were pseudophakic, one was aphakic, and lens luxation into the vitreous was seen in one eye. Twenty-two patients (81%) had PVR grade Cp and 5 patients (19%) had PVR grade Ca. The macular retina was attached in 7 eyes (26%) and detached in 20 eyes (74%). Of the 17 phakic eyes, 5 (29%) had undergone phacoemulsification during the first vitrectomy, 9 (53%) during re-surgery, and 1 (6%) after vitreoretinal surgeries, and 2 (12%) did not undergo phacoemulsification. Of the 27 study eyes, 9 (33%) had retinotomy during the first surgery for retinal detachment, and 18 (67%), during re-surgery. In addition, of the 27 study eyes, 20 (74%) had one surgery with retinotomy, 6 (22%), two surgeries with retinotomy due to retinal re-detachment, and one (4%), three surgeries with retinotomy. Moreover, eleven eyes (40%) had retinotomy of less than 90°, eight (30%), of 90° to 180°, four (15%), of 180° to 270°, and four (15%), 360° (circumferential retinotomy). Additional radial retinotomy was performed in 5 eyes (19%). Two patients with penetrating ocular injury underwent retinotomy combined with choroidectomy. 25G vitrectomy was performed using the Constellation® vision system (Alcon, Fort Worth, TX) and 25-G Constellation Vitrectomy Pak. Chandelier illumination and bimanual technique were used in 12 eyes (44%). Retinotomy technique Epiretinal membranes were removed as peripheral as possible up to the vitreous base. Electric coagulation was performed to mark the edge of retinotomy centrally from site of membrane adhesion. Retinotomy was created using a vitreous cutter or scissors so to make the edge of retinotomy approaching the ora serrata. The retina peripheral to retinotomy was removed (retinoectomy). Retinotomy was performed until the retina was uniformly reattached to the pigment epithelium. Perfluorodecalin was introduced to make sure that the retina was uniformly attached to the pigment epithelium. Radial retinotomy was performed (Fig. 1) if there was circumferential contraction. Subretinal membranes were removed, if present. The internal limiting membrane was removed. Laser coagulation along the retinotomy edge and around retinal break was applied and silicone oil endotamponade was performed.
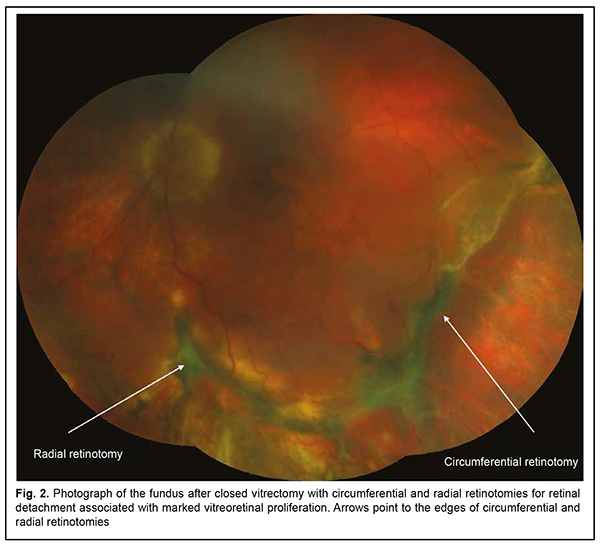
The efficacy of surgery was assessed using the following criteria: anatomical success (if retinal re-attachment was achieved, particularly following removal of silicone oil), number of repeat surgeries to achieve anatomical success, visual acuity before and after surgery, and any intra- and postoperative complications. Results Of the 27 eyes, retinal reattachment was achieved after the first surgery in 20 eyes (74%), after re-surgery in 5 eyes (19%). In addition, anatomical success was achieved after removal of silicone oil in 15 eyes (56%). By the time of analysis, silicone oil was not removed in 12 eyes (44%). Complete retinal re-attachment was achieved in 25 eyes (93%), and partial re-attachment, in 2 eyes (7%). Fig. 2 illustrates the anatomical success of surgery involving circumferential and radial retinotomy.
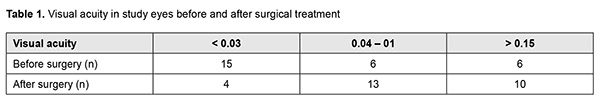
The visual acuity improved in 14 eyes (52%), decreased in 8 eyes (30%), and did not change in 5 eyes (18%). Table 1 shows best-corrected visual acuity (BCVA) in study patients before and after surgical treatment.
Retinal hemorrhage during retinotomy was observed in 22 of the 33 surgeries involving retinotomy and was the most common intraoperative complication (63%). We increased the IOP and performed retinal, and, if required, choroidal coagulation in an attempt to arrest hemorrhages. Subretinal gas, perfluorodecalin, and silicone oil in 5/35 cases (14%), 2/35 cases (6%), and 2/35 cases (6%), respectively, was the second most common intraoperative complication. Subretinal gas was an indication for additional retinotomy within the same procedure. Subretinal perfluorodecalin or silicone oil had to be removed, and patients with this complication frequently required additional retinotomy. In some cases, it was difficult to flatten the retina (retinal slippage). Particularly, this was observed in cases with retinotomy of 180° or more, with the retina tending to shift toward the optic disc and fold up. In these cases, radial retinonomy should be performed. Retinal folds may be additionally flattened under silicone oil. Migration of silicone oil into the anterior chamber (4/35 cases; 11%) was observed in eyes with posterior lens capsule defects or inadequately sealed corneal incisions. Postoperative complications included recurrent retinal detachment with PVR in 7/27 eyes (26%), macular hole in 3/27 eyes (11%), secondary glaucoma in 2/27 eyes (7%), iridocyclitis with hypotony (the IOP less than 12 mmHg) in 3/27 eyes (11%), optic disc atrophy in 1/27 eye (4%), and subretinal silicone in 1/27 eye (4%). Most patients (85%) self-reported metamorphopsia after surgery. Iridocyclitis was successfully treated with topical therapy. Iridocyclitis was frequently seen in conjunction with hypotony. Persistent hypotony in the late postoperative period was a relative contraindication for the removal of silicone oil. In some cases, hypertension was symptomatic and successfully treated hypotensive agents. Secondary glaucoma was associated with silicone oil emulsification, and patients with this complication required a more urgent silicone oil removal. Silicone oil was replaced in 1/27 eye (4%) due to silicone oil emulsification. Discussion Because retinotomy is a traumatic procedure that is difficult to perform, indications for retinotomy should be clear and unambiguous and balanced with potential hazards [3]. Most authors believe that foreshortened and stiffened retina secondary to severe PVR is another indication for retinotomy, in addition to incarceration of the retina with scleral scarring after penetrating ocular injury [4-9]. A decision on the requirement for relaxing retinotomy should be made intraoperatively after removal of the membranes because it is much easier to remove them before retinotomy than after. Failure to do it can result in excessive retinectomy and retained membranes, potentially leading to retinal re-detachment [10]. Achieving tension-free re-attachment of the retina to the choroid is a must. Here the rule of thumb is that little excess is better than little less. It is important to decide whether to perform a circular (360 º) retinotomy or to leave a portion of the peripheral retina in order to prevent its rotation. The retina peripheral to the site of retinotomy should be removed (retinectomy) because it is a source of the vascular endothelial growth factor [10]. We found that, in case of retinal slippage, retinal folds may be additionally flattened under silicone oil. In some cases, laser coagulation may be postponed to achieve better flattening of the retina, and performed not intra-operatively, but postoperatively. The anatomical success rate, functional outcomes, and types of intraoperative and postoperative complications for patients of this study were close to those reported by others. In a study by Jiang et al [11], of the 44 eyes that received retinotomy, 31 eyes (70.5%) had at least one prior pars plana vitrectomy. Retinal attachment was achieved in 27 (61.4%) eyes with one surgery, 11 (25%) eyes with two surgeries, and 3 (6.8%) eyes with three surgeries. Thus, overall, 41/44 (93%) were successfully reattached with relaxing retinectomy and vitrectomy. Of these, 21 eyes (47.7%) eyes remained attached under silicone oil. If the IOP remained 10 mmHg or below, the silicone oil was left in place regardless of anatomical reattachment. Others reported a somewhat better atamomical success rate. Tan and al [12] described the functional and anatomic results of retinectomy without scleral buckling for anterior proliferative vitreoretinopathy in eyes that did not undergo previous buckling surgery. The anatomic success rate was 77.2%. Final attachment rate was 95.9%, reached after 1 rhegmatogenous retinal detachment reoperation in 21 cases and after 2 rhegmatogenous retinal detachment reoperations in 4 cases. In a study by Quiram et al [13], retinal re-attachment after the first surgery was achieved in 34 of 56 patients (60%), and complete retinal reattachment was achieved in 52 of 56 patients (93%). Iwahasi-Shima et al [14] evaluated the outcome of 25-gauge vitrectomy for repair of rhegmatogenous retinal detachment (RRD) complicated by PVR. The retina was reattached in 21 eyes (77.8%) after the initial vitrectomy and in 25 eyes (92.6%) at the final examination. Adhi et al [15] assessed anatomical and functional outcomes of retinectomies in retinal detachments complicated by proliferative vitreoretinopathy in 370 eyes. The extent of retinectomies varied from up to 90° in 126 (34.05%) cases and 180° in 105 (28.38%) to 360° in 139 (37.57%) cases. The retina was flat after the first surgery in 311 (84.05%) eyes, and after one or more repeat surgeries in 344 (92.97%) eyes. Phacoemulsification was performed as part of the procedure in all phakic eyes. Seventy-one patients (19.19%) had visual acuity of 0.1 or better preoperatively, and 211 (57.02%) cases achieved visual acuity of 0.1 or better after treatment. Others also noted the complications similar to those seen in our study. In a study by Adhi et al [15], the most common intraoperative complication associated with retinectomy was intraocular hemorrhage (80 eyes; 21.62%). In addition, subretinal PFCL was seen in 14 (3.78%) eyes, SO in the anterior chamber, in 32 (8.65%) eyes, hypotony (< 5 mm Hg), in 24 (6.49%) eyes, optic atrophy, in 16 (4.32%) eyes, and secondary glaucoma, in 57 (15.41%) eyes. In the current study, the postoperative percentage of eyes with hypotony was 11% (3/27 eyes), which is comparable to the results reported by Jiang et al [11] (6.8%) and Scott et al [16] (15%). There has been a transition from 20G and 23G closed vitrectomy to 25G vitrectomy for most vitreoretinal diseases, and there have been fewer studies on the efficacy of 25G vitrectomy than on the efficacy of 20G and 23G vitrectomy for retinotomy and retinectomy. We found a 25G vitrectomy to be rather efficient for retinotomy and retinectomy, which is in agreement with findings of others [11]. Silicone oil tamponade is commonly used in closer vitrectomy with retinotomy for retinal detachment with marked PVR [3]. However, silicone oil tamponade can cause complications like elevated IOP and silicone oil emulsification, which requires repeat surgery. The above complications made use gas endotamponade after retinotomy. Papastavrou et al [17] reported primary and secondary success rates of 75% and 88.3%, respectively, and hypotony in one (8.3%) patient, for gas tamponade for retinectomy in PVR-related retinal detachments. These results were somewhat worse than those reported by us and others for silicone tamponade for retinectomy in PVR-related retinal detachments. Another important question is whether it makes sense to remove the opacified crystalline lens or IOL and replace it with a clear IOL. Tseng et al [18] believe that lens removal is not mandatory in all cases with PVR-related retinal detachments. On the contrary, Quiram et al [13] advocated radical anterior vitreous base dissection and lensectomy or removal of IOL in retinectomy with PVR-related retinal detachments. Our results demonstrate that, in marked PVR requiring a rather complex and long surgery with retinotomy, the necessity for cataract phacoemulsification will arise sooner or later. Therefore, it is better to plan closed vitrectomy in combination with cataract phacoemulsification. Another advantage of intraoperative phacoemulsification is an improved performance of the procedure of closed vitrectomy. References 1.Machemer R. [Cutting of the retina: a means of therapy for retinal reattachment]. Klin Monbl Augenheilkd. 1979;175(50):597–601. German. 2.Machemer R, Aaberg TM, Freeman HM, Irvine AR, Lean JS, Michels RM. An updated classification of retinal detachment with proliferative vitreoretinopathy. Am J Ophthalmol. 1991 Aug 15;112(2):159‐165. 3.Khan MA, Brady CJ, Kaiser RS. Clinical management of proliferative vitreoretinopathy: an update. Retina. 2015;35:165–175. 4.Eckardt C, Behrendt S, Zwick A. Results of silicone oil removal from eyes treated with retinectomies. Ger J Ophthalmol. 1992;1(1):2–6. 5.Bovey EH, de Ancos E, Gorivers M. Retinotomies of 180 degrees or more. Retina. 1995;15(5):394–398. 6.Faude F, Lambert A, Wiedemann P. 360 degrees retinectomy in severe anterior PVR and PDR. Int Ophthalmol. 1998;22(2):119–123. 7.Lesnoni G, Billi B, Rossi T, Stirpe M. The use of panoramic viewing system in relaxing retinotomy and retinectomy. Retina. 1997;17(3):186–190. 8.Reinking U, Lucke K, Bopp S, Laqua H. Results after retinotomy and retinectomy in the treatment of complicated retinal detachment. Klin Monbl Augenheilkd. 1990;197(5):382–5. 9.Shalaby KA-G. Relaxing retinotomies and retinectomies in the management of retinal detachment with severe proliferative vitreoretinopathy (PVR). Clin Ophthalmol. September 2010:1107. d 10.Kuhn F. Vitreoretinal Surgery: Strategies and Tactics. Springer International Publishing; 2016. 551 р. 11.Jiang Y, Oh DJ, Messenger W, Lim JI. Outcomes of 25-gauge vitrectomy with relaxing retinectomy for retinal detachment secondary to proliferative vitreoretinopathy. J Vitreoretin Dis. 2019;3(2):69‐75. 12.Tan HS, Mura M, Lesnik Oberstein SY, de Smet MD. Primary Retinectomy in Proliferative Vitreoretinopathy. Am J Ophthalmol. 2010;149(3):447–452. 13.Quiram PA, Gonzales CR, Hu W, et al. Outcomes of Vitrectomy with Inferior Retinectomy in Patients with Recurrent Rhegmatogenous Retinal Detachments and Proliferative Vitreoretinopathy. Ophthalmology. 2006;113(11):2041–2047. 14.Iwahashi-shima C, Sato T, Bando H, Ikeda T, Emi K. Anatomic and functional outcomes of 25-gauge vitrectomy for repair of eyes with rhegmatogenous retinal detachment complicated by proliferative vitreoretinopathy. Clin Ophthalmol. 2013;7:2043–9 15.Adhi MI, Siyal N, Aziz S. Anatomical and functional outcomes of retinectomies in retinal detachments complicated by proliferative vitreoretinopathy. Saudi J Ophthalmol. 2017;31(4):216-223. 16.Scott IU, Flynn HWJ, Murray TG, Feuer WJ. Outcomes of surgery for retinal detachment associated with proliferative vitreoretinopathy using perfluoro-n-octane: a multicenter study. Am J Ophthalmol. 2003;136(3):454–463. 17.Papastavrou VT, Chatziralli I, McHugh D. Gas Tamponade for Retinectomy in PVR-Related Retinal Detachments: A Retrospective Study. Ophthalmol Ther. 2017;6(1):161‐166. The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|