Influence of the morphology metrics of serous PED in AMD on the success of triamcinolone acetonide monotherapy
T.B. Kustryn, MD
Filatov Institute of Eye Diseases and Tissue Therapy, NAMS of Ukraine
Odessa, Ukraine
E-mail: laserfilatov@gmail.com
Background: Serous detachment of retinal pigment epithelium (RPE) is a special form of age-related macular degeneration (AMD) and accounts for approximately 10% of all cases of exudative AMD. In the natural course of retinal pigment epithelial detachment (PED), RPE tear, subretinal neovascularization and RPE atrophy develop and are accompanied by severe and irreversible loss of central vision.
Purpose: To determine the prognostic factors for success of triamcinolone acetonide (TA) for serous PED in AMD.
Materials and Methods: Fifty-two patients (54 eyes) with serous PED associated with AMD who were treated with either intravitreal or subtenon TA were followed up over 36 months. At baseline and follow-up visits, they underwent general eye examination including visual acuity assessment, ophthalmoscopy, color fundus photography, long-wave fundusgraphy, fluorescein angiography and macular optical coherence tomography (OCT).
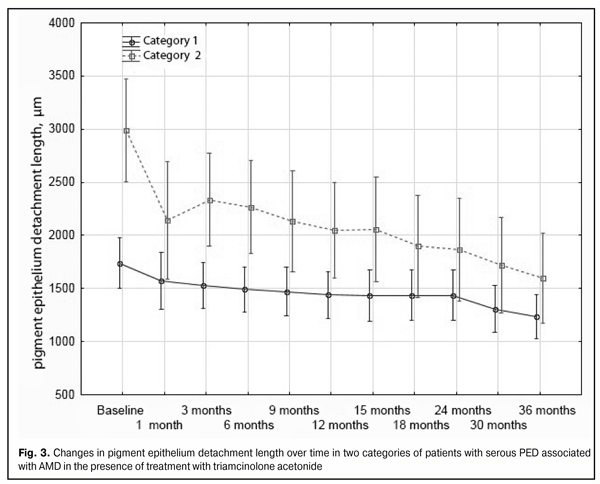
Results: On the basis of a K-means cluster analysis we distinguished two categories of patients with serous PED, which differed in the values of two baseline indices (PED height and length). Over the follow-up period, complete re-attachment was achieved in 60% of cases having higher baseline PED height and more extensive (i.e., longer) baseline PED length versus 23.5% of cases having lower baseline PED height and less extensive baseline PED length (p = 0.01). Triamcinolone acetonide reduced significantly the height and length of PED in both categories of patients over 36 months, with their visual acuity remaining stable compared to the baseline values. Over the 36-month follow-up period, subretinal neovascular membrane developed in 7 (13%) eyes treated with TA.
Conclusion: Higher and more extensive PEDs were found to predict a more favorable response to TA monotherapy. Following administration of TA, complete re-attachment was achieved in 60% of cases having higher baseline PED height and more extensive baseline PED length. Anatomical and morphological features of a serous PED have no effect on the frequency of subretinal neovascular membrane formation.
Key words: serous retinal pigment epithelium detachment, age-related macular degeneration, triamcinolone acetonide
Introduction
Serous detachment of retinal pigment epithelium (RPE) is a special form of age-related macular degeneration (AMD) [1] and accounts for approximately 10% of all cases of exudative AMD. In the natural course of retinal pigment epithelial detachment (PED), RPE tear, subretinal neovascularization and RPE atrophy develop and are accompanied by severe and irreversible loss of central vision.
Although the pathogenesis of PED formation in AMD has not yet been completely elucidated, it is known that the course of PED is influenced by choriocapillaris abnormalities, decreased adhesion between the Bruch’s membrane and the RPE, age-related changes in the structure of Bruch’s membrane, increased lipid content, and poor RPE pump function [2, 3].
Local inflammation leading to the disruption of the anatomical connection between the RPE and the membrane significantly contributes to the pathogenesis of PED in AMD [4, 5]. In addition, it has been hypothesized that that the release of enzymes and cytokines by inflammatory cells (including macrophages) causes changes in the Bruch’s membrane, thus promoting further accumulation of macrophages and stromal white cells in the focus of the pathology as well as enhanced inflammatory response [6, 7]. Thereupon, the development of novel effective treatments for serous PED in AMD has been actively debated in literature.
Purpose: To determine the prognostic factors for success of triamcinolone acetonide (TA) for serous PED in AMD.
Materials and Methods
This was a prospective, single-center comparative study. Fifty-two patients (54 eyes) with serous PED associated with AMD who were treated with either intravitreal or subtenon TA were followed up over 36 months. At baseline and follow-up visits, they underwent general eye examination including visual acuity assessment, ophthalmoscopy, color fundus photography, long-wave fundusgraphy, fluorescein angiography and macular optical coherence tomography (OCT). OCT was used to measure the maximum height and maximum length of PED.
The decision to administer a repeat injection was made at 3 months after previous injection if OCT showed no evidence of decrease in the amount of detachment.
The StatSoft© Statistica® 10.0 (StatSoft, Tulsa, OK) was used for statistical analysis and plotting. Mean (M) and standard deviation (SD) values were obtained for each group. Post-treatment changes in characteristics (visual acuity, height and length of PED) over time in the groups were analyzed by using repeated-measures ANOVA followed by a Newman-Keuls test.
To perform the analysis of treatment efficacy depending on the size of serous PED, patients were automatically classified into one of two categories based on two PED dimensions (PED height and length).
Results and Discussion
Since we have previously demonstrated that the efficacy of treatment of serous PED associated with AMD does not depend on the route of administration of TA [8], we grouped all 52 patients (54 eyes) into a cohort for cluster analysis. As a result, we distinguished two categories of patients with serous PED, which differed in the values of two PED dimensions.
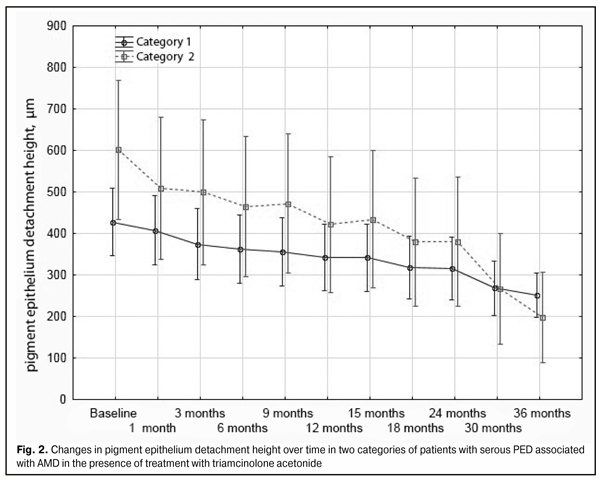
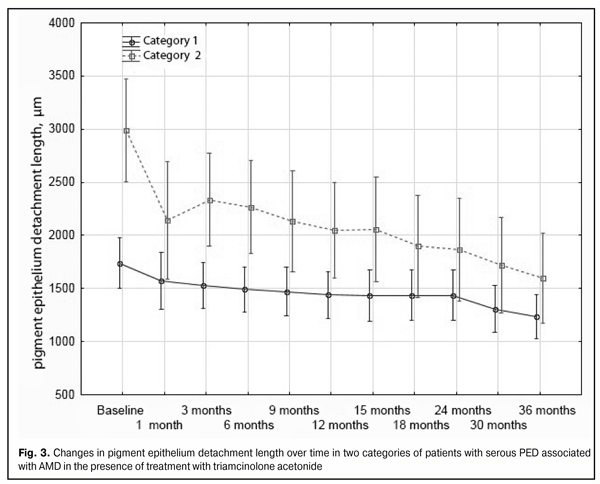
Category 1 patients (32 patients; 34 eyes) had a lower and less extensive (i.e., shorter) detachment compared to that in category 2 patients (20 patients; 20 eyes), with mean height and mean length values of 428 (170) µm versus 602 (231) µm and 1740 (509) µm versus 2987 (596) µm, respectively. Therefore, in category 1 patients, the detachment height was statistically significantly lower, and the detachment length was statistically significantly shorter compared to those in category 2 patients (p = 0.001).
By month 36, complete re-attachment was achieved in 60% (12/20 eyes) of category 2 cases versus 23.5% (8/34 eyes) of category 1 cases (p = 0.01). Over a follow-up period, RPE redetachments occurred in 5.9% (2/34 eyes) of category 1 cases versus 10% (2/20 eyes) of category 2 cases, with no significant difference in the frequency of RPE redetachment between the two categories (p = 0.6).
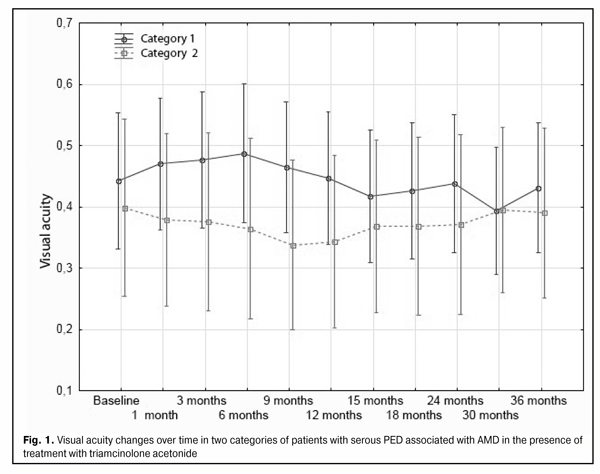
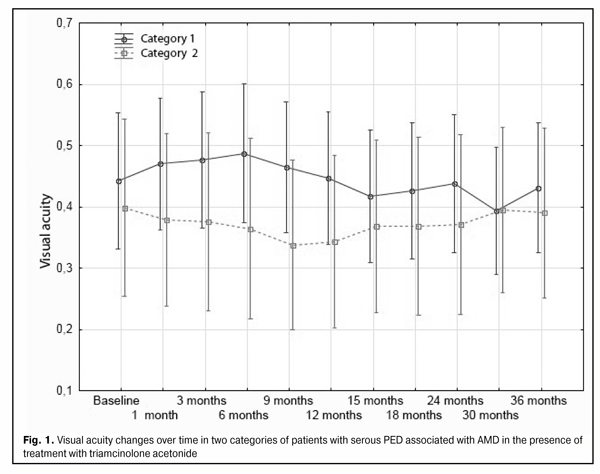
At baseline, the mean visual acuity in category 1 cases and category 2 cases was 0.44 (0.33) and 0.4 (0.3), respectively, with no significant intercategory difference (p = 0.6). At month 36, the mean visual acuity was similar between category 1 cases and category 2 cases (0.43 (0.33) versus 0.39 (0.25), with no significant intercategory difference (p = 0.6)). It should be noted that over the follow-up period, visual acuity in patients of both categories remained stable compared to the baseline values (Fig. 1).
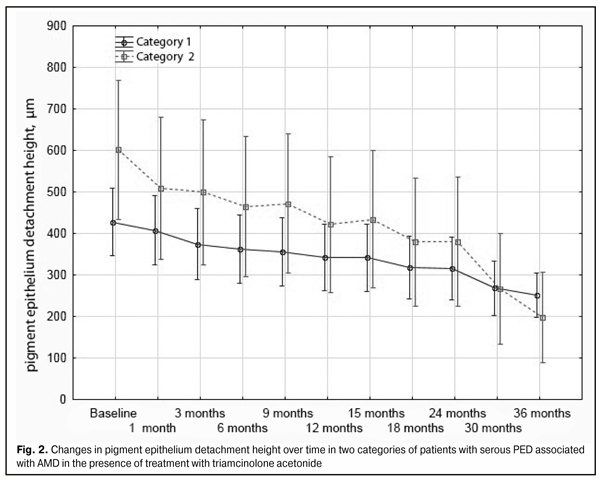
At baseline, the mean detachment height was lower in category 1 cases than in category 2 cases (428 (170) µm vs 602 (231) µm, with a significant intercategory difference (p = 0.001)). No significant intercategory difference in the mean detachment height among category 1 cases and category 2 cases was observed (251 (127) µm vs 198 (59) µm, p = 0.5) at the final follow-up time point.
The mean baseline length of serous PED was significantly longer in category 2 cases than in category 1 cases (1740 (509) µm and 2987 (596) µm, respectively, p = 0.001). The mean 36-month length of serous PED was 1233 (440) µm and 1597 (561) µm in category 1 cases and category 2 cases, respectively (p = 0.2) (Fig. 3).
The number of TA injections needed over the treatment period was statistically significantly higher for category 1 cases than for category 2 cases (5.1 (2.1) vs 3.5 (1.7), p = 0.006).
Over the period of treatment with TA, a subretinal neovascular membrane (SNM) developed in 4/34 (12%) of eyes of category 1 cases versus 3/20 (15%) of eyes of category 2 cases, with no significant difference in SNM formation rate between the two categories (p = 0.29). In addition, over a 36-month follow-up, complete re-attachment has been achieved in 20/54 (37%) of eyes treated with TA for serous PED. No significant difference in the percentage of re-attachments between the two routes of administration of TA (p = 0.9) has, however, been observed [8].
In the study reported here, to identify the factors influencing the outcome of treatment with TA for serous PED, patients were classified into two categories, those who had a lower and less extensive (i.e., shorter) serous PED (category 1), and those who had a higher and more extensive (i.e., longer) serous PED (category 2) at baseline, based on a K-means cluster analysis. The analysis of treatment outcomes in patients revealed that complete re-attachment was achieved in 60% of category 2 cases versus 23.5% of category 1 cases (p = 0.01). Therefore, higher and more extensive PEDs are more responsive than lower and less extensive PEDs to TA monotherapy, with a lower number of injections needed over the treatment period.
Other authors have also reported the importance of the baseline PED size as a prognostic factor for outcome of treatment for AMD. Leitritz and colleagues [9] demonstrated that the risk of an RPE tear after bevacizumab treatment for AMD is increased in patients with the PED height of > 600 µm. Chan and colleagues showed that elevated preinjection vPED height > 400 µm was a significant risk for RPE tears after bevacizumab injections for vPED eyes [10]. In addition, in a study of Doguizi and Ozdek [11], a PED height >580 µm was found to be a significant risk factor for RPE tear formation associated with anti-VEGF therapy. Sarraf and co-authors [12] have reported that a baseline PED height >550 microns was identified as a high-risk factor for the subsequent development of an RPE tear in eyes with AMD receiving anti-VEGF therapy.
It should be also noted that administration of TA contributed to statistically significant reductions in the height and length of PED in both categories of patients in our study over 36 months, with visual acuity remaining stable compared to the baseline values.
During the 18-month observation period in the study conducted by the Moorfields macular study group [13], a tear of the RPE developed in 3/24 (12.5%) of untreated patients and in 2/21 (9.5%) of patients treated with photocoagulation for serous PED in AMD. However, in our study, no case of tear of the RPE was revealed in eyes treated with TA for serous PED in AMD.
Barondes and colleagues [14] showed that SNM developed in 10 (45%) untreated eyes with PED, which is 35% higher than the percentage in our study (95% CI = 12.4 to 55.6; p = 0.004). In addition, SNM developed in 8 (40%) eyes treated with photocoagulation for serous PED in AMD [4], which is 25% higher than in the use of TA for this disorder (95% CI = 3.4 to 47.5; p = 0.004).
During the 36-month follow-up period in our study, SNM developed in 7 (13%) eyes treated with TA for serous PED in AMD. Thus, SNM developed in 4/34 (12%) eyes in category 1 patients (having a lower and less extensive PED), versus 3/20 (15%) eyes in category 2 patients (having a higher and more extensive PED), with no significant intercategory difference (p = 0.29).
Therefore, development of a subretinal neovascular membrane does not depend on the route of administration of TA and on the baseline size of serous PED.
Conclusion
Higher and more extensive PEDs are more responsive than lower and less extensive PEDs to TA monotherapy. Following administration of TA, complete re-attachment was achieved in 60% of cases having higher baseline PED height and more extensive (i.e., longer) baseline PED length.
Patients were classified into two categories, those who had a lower and less extensive serous PED (category 1), and those who had a higher and more extensive serous PED (category 2) at baseline, based on a K-means cluster analysis. Category 1 patients had a PED with mean baseline height and mean baseline length values of 428 (170) µm and 1740 (509) µm versus 602 (231) and 2987 (596) µm, respectively, in category 2 patients.
Anatomical and morphological features of a serous PED have no effect on the frequency of subretinal neovascular membrane formation.
References
1. Pasyechnikova NV, Korol AR. [Clinical classification and tactics of management of patients with age related macular degeneration]. Oftalmol Zh. 2010;2:38-41 Russian
2. Bird AC. Doyne Lecture. Pathogenesis of retinal pigment epithelial detachment in the elderly; the relevance of Bruch's membrane change. Eye. 1991;5:1–12
Crossref Pubmed
3. Holz FG, Pauleikhoff D, Klein R, et al. Pathogenesis of lesions in late age-related macular disease. Am J Ophthalmol. 2004 Mar;137(3):504-10
Crossref Pubmed
4. Anderson DH, Mullins RF, Hageman GS, et al. A role for local inflammation in the formation of drusen in the aging. Am J Ophthalmol. 2002; 134:411-31
Crossref Pubmed
5. Hageman GS, Luthert PJ, Victor Chong NH, et al. An integrated hypothesis that considers drusen as biomarkers of immune-mediated processes at the RPE-Bruch’s membrane interface in aging and age-related macular degeneration. Prog Retin Eye Res. 2001 Nov;20(6):705-32
Crossref Pubmed
6. Dastgheib K, Green WR. Granulomatous reaction to Bruch’s membrane in age-related macular degeneration. Arch Ophthalmol. 1994; 112:813-8
Crossref Pubmed
7. Seregard S, Algvere P, Berglin L. Immunohistochemical characterization of surgically removed subfoveal fibrovascular membranes. Graefes Arch Clin Exp Ophthalmol. 1994 Jun;232(6):325-9
Crossref Pubmed
8. Kustryn TB, Nasinnyk IO, Nevskaya AA, et al. [Changes in structural and functional retinal features resulting from the effect of a long-acting steroid in serous PED associated with AMD: a 36-month follow-up study]. Oftalmol Zh. 2016;5:28-34 Russian
Crossref
9. Leitritz M, Gelisken F, Inhoffen W, et al. Can the risk of retinal pigment epithelium tears after bevacizumab treatment be predicted? An optical coherence tomography study. Eye. 2008; 22:1504–7
Crossref Pubmed
10. Chan CK, Abraham P, Meyer CH, Kokame GT, et al. Optical coherence tomography-measured pigment epithelial detachment height as a predictor for retinal pigment epithelial tears associated with intravitreal bevacizumab injections. Retina. 2010 Feb;30(2):203–11
Crossref Pubmed
11. Doguizi S, Ozdek S. Pigment epithelial tears associated with anti-VEGF therapy: incidence, long-term visual outcome, and relationship with pigment epithelial detachment in age-related macular degeneration. Retina. 2014 Jun;34(6):1156-62
Crossref Pubmed
12. Sarraf D, Chan C, Rahimy E, Abraham P. Prospective evaluation of the incidence and risk factors for the development of RPE tears after high- and low-dose ranibizumab therapy. Retina. 2013 Sep;33(8):1551-7
Crossref Pubmed
13. Moorfields macular study group. Retinal pigment epithelial detachments in the elderly: a controlled trial of argon laser photocoagulation. Br J Ophthalmology. 1982 Jan; 66(1): 1–16
Crossref Pubmed
14. Barondes MJ, Pagliarinit S, Chisholm IH, et al. Controlled trial of laser photocoagulation of pigment epithelial detachments in the elderly: 4 year review. Br J Ophthalmol. 1992;76(1):5-7
Crossref Pubmed