J.ophthalmol.(Ukraine).2016;5:28-34.
|
https://doi.org/10.31288/oftalmolzh201652834 Changes in structural and functional retinal features resulting from the effect of a long-acting steroid in serous PED associated with AMD: a 36-month follow-up study T.B. Kustryn, MD I.O. Nasinnyk, Cand Sc (Med) A.A. Nevskaya, MD O.S. Zadorozhnyy, Cand Sc (Med) A.R. Korol, Dr Sc (Med) Filatov Institute of Eye Diseases and Tissue Therapy Odessa, Ukraine E-mail: laserfilatova@gmail.com
Background: Although a variety of approaches are available for treating retinal pigment epithelial detachment (PED) associated with age-related macular degeneration (AMD), no unified methodology has yet been approved and/or overwhelmingly favored. Purpose: To investigate the effect of a long-acting steroid on the structural and functional RPE features in serous PED associated with AMD in long-term follow-up study, and to improve the efficacy of treatment of this disorder through the use of steroid therapy based on the findings of this investigation. Materials and Methods: Fifty-two patients (54 eyes) with serous PED associated with AMD were followed up for 36 months. They were divided into subtenon and intravitreal groups comprising 30 patients (32 eyes) and 22 patients (22 eyes), respectively, and treated with 0.5 ml (40 mg) subtenon triamcinolone acetonide (TA) suspension and 0.1 ml (4 mg) intravitreal TA crystals, respectively, as needed. Results: We found significant reductions in the height and length of PED in the intravitreal group (from 486 (SD 187) µm to 256 (SD 139) µm, P = 0.005; and from 1859 (SD 911) µm to 1112 (SD 451) µm, P = 0.04, respectively) and in the subtenon group (from 446 (SD 199) µm to 231 (SD 107) µm, P = 0.0001; and from 2055 (SD 587) µm to 1423 (SD 465) µm, P = 0.02, respectively). In study eyes, the visual acuity remained stable throughout the 36-month follow-up period, irrespective of the route of administration of TA. Conclusion: The use of subtenon and intravitreal TA in serous PED associated with AMD is efficacious for maintaining the anatomical structure of the retina. Key words: serous retinal pigment epithelial detachment, age-related macular degeneration, subtenon and intravitreal injections, triamcinolone acetonide
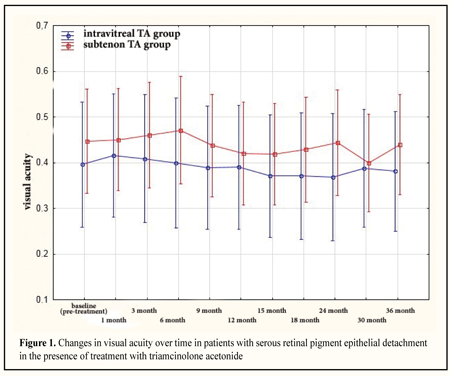
Introduction Although a variety of approaches are available for treating retinal pigment epithelial detachment (PED) associated with age-related macular degeneration (AMD), no unified methodology has yet been approved and/or overwhelmingly favored. The use of retinal laser photocoagulation (RLP) for this purpose began in the 1980s and 1990s. It has been demonstrated in multiple studies that RLP results in developing an RPE tear, subretinal neovascular membranes (SNMs), retinal atrophy and abrupt decrease in central vision [1, 2]. Subsequently, inadequate efficacy of photodynamic therapy for this disorder was reported [3, 4]. Although in recent years, increasing attention has been focused on vascular endothelial growth factors (VEGF), the use of VEGF inhibitors in serous PED often results in developing an RPE tear and loss of central vision [5-7]. More recently, publications have appeared on the use of combination therapy in exudative AMD. A number of studies have demonstrated improved outcomes for patients with this disorder treated with combination of laser therapy, anti-VEGF agents and triamcinolone acetonide (TA) [8-10]. Triamcinolone acetonide is a long-acting synthetic steroid with anti-inflammatory and anti-edematous effects. The efficacy of intravitreal and subtenon TA for diabetic macular edema, retinal vein occlusion-related macular edema, and rhegmatogenous retinal detachment has been already well studied [11-14]. Given the avascular nature of PED, the presence of elements of inflammation in the pathogenesis of, and the improved efficacy of treating PED with a combination including TA, we have hypothesized previously that this disorder, when associated with AMD may be treated with a TA monotherapy [15]. The purpose of the study was to investigate the effect of a long-acting steroid on the structural and functional RPE features in serous PED associated with AMD in long-term follow-up study, and to improve the efficacy of treatment of this disorder through the use of steroid therapy based on the findings of this investigation. Materials and Methods This was a prospective, single-centre, comparative study. Fifty-two patients (54 eyes) with serous PED associated with AMD were followed up. They were divided into subtenon and intravitreal groups comprising 30 patients (32 eyes) and 22 patients (22 eyes), respectively, and treated with 0.5 ml (40 mg) subtenon TA suspension and 0.1 ml (4 mg) intravitreal TA crystals, respectively, as needed. A repeat injection was made at 3 months after previous injection, if no decrease in OCT-derived dimensions over this 3-month period was observed. The control data of the Moorfields macular study group based on the controlled trial of argon laser photocoagulation for PEDs in the elderly were used as controls [16, 17]. At baseline, complaints were collected and detailed histories were taken. Thereafter, patients underwent a general eye examination including visual acuity assessment and ophthalmoscopy. In addition, they underwent ocular imaging with color fundus photography, long-wave fundusgraphy, fluorescein angiography and macular optical coherence tomography (OCT). OCT-derived retinal structural parameters, maximum PED height and length at different meridians, were investigated. A general eye examination and ocular imaging studies were performed at baseline and at 1, 3, 6, 9, 12, 15, 18, 24, 30 and 36 months. Primary efficacy endpoints were stabilization of visual acuity and complete re-attachment of the RPE. Major secondary efficacy endpoints included ocular adverse events such as RPE tears, formation of subretinal neovascular membranes and RPE atrophy. Patients of the study were followed up at the Laser Eye Microsurgery Department of the Filatov Institute of Eye Disease. The statistical package StatSoft© Statistica® 10.0 (StatSoft, Tulsa, OK) was used for development of a primary database, data processing and plotting. Repeated measures ANOVA were conducted to examine post-treatment changes in variables over time. The Mann-Whitney rank test was used for data comparison at each of the follow-up time points between groups. The McNemar test was used to assess the treatment efficacy in each arm, and the groups were compared for efficacy using 95% confidence intervals. P < 0.05 was considered statistically significant in all the analyses. Results and Discussion Fifty-two patients (54 eyes; male-to-female percentage, 39.4% to 60.6%; mean age, 66.0 (SD 7.5) years; age range, 47 to 85 years) with serous PED associated with AMD received a complete course of the study. There was no significant difference in the baseline mean visual acuity (SD) between those who received intravitreal TA and those who received subtenon TA (mean (SD), 0.4 (0.3) µm versus 0.45 (0.33); P = 0.6). At 36 months, the mean visual acuity (SD) in the intravitreal group was 0.38 (0.3) (P = 0.7) versus 0.45 (0.33) in the subtenon group (P = 0.8). At the final follow-up time point, no significant difference in visual acuity between the two groups was observed (P = 0.4). In each of the two groups, no significant decrease in visual acuity was observed over the 36-month follow-up period (Fig. 1).
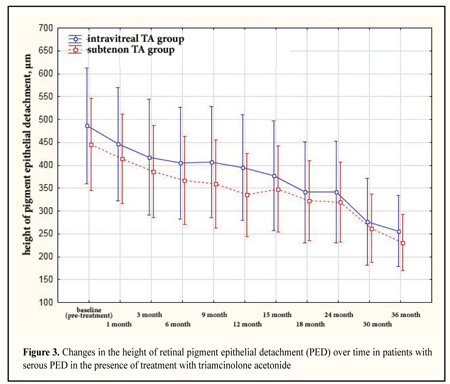
At the next stage of the study, we assessed changes in height and length of serous PED in AMD in the presence of treatment with TA at each of the follow-up time points. There was no significant difference in the baseline height of serous PED between those who received intravitreal TA and those who received subtenon TA (mean (SD), 486 (187) µm versus 446 (199); P = 0.4). At 36 months, the height of serous PED in the intravitreal group was 256 (139) µm versus 231 (107) µm in the subtenon group (Fig. 2), with no significant difference in the height between the two groups (P = 0.7). A significant decrease in the height of RPE detachment was observed in both groups over the 36-month follow-up period (Fig. 3).
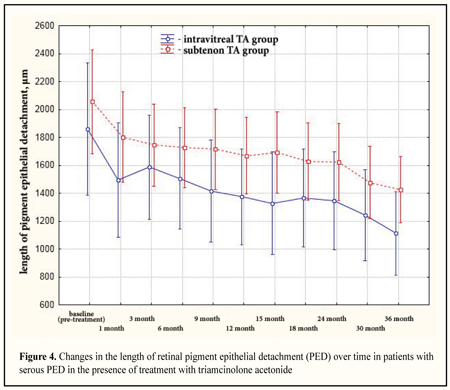
There was no significant difference in the baseline length of serous PED between those who received intravitreal TA and those who received subtenon TA (mean (SD), 1859 (911) µm versus 2055 (587) µm; P = 0.3). At 36 months, the length of serous PED in the intravitreal group and in the subtenon group was 1112 (451) µm and 1423 (465) µm, respectively, with no significant difference in the length of serous PED between the groups (P = 0.17). We found a significant decrease in the length of PED in both groups over the 36-month follow-up period (Fig. 4).
The mean number of injections in the intravitreal group was 3.6 (1.7) versus 5.2 (2.1) in the subtenon group, with a significant difference between the groups (P = 0.005). A primary outcome was complete re-attachment of the RPE. At the final follow-up time point (36 months), complete re-attachment of the RPE was achieved in 20 of 54 eyes (37%) treated with TA, and this rate was 36.4% in the intravitreal group versus 37.5% in the subtenon group, with no significant difference between the two routes of administration of TA (P = 0.9). Over a 36-month follow-up period, RPE re-detachments occurred in 3 eyes (13.6%) of the intravitreal group, with no significant difference in this rate between the two groups (P = 0.15). At 30 months, subretinal neovascular membranes formed in 2 eyes of the intravitreal group versus 3 eyes of the subtenon group. At 36 months, subretinal neovascularization was found in 2 more eyes of the intravitreal group. Over the 36-month follow-up period, SNMs formed in 4/22 (18%) of eyes of the intravitreal group versus 3/32 (9%) of eyes of the subtenon group, with no significant difference in SNM formation rate between the two groups (P = 0.34). Therefore, over a 3-year observation period, subretinal neovascularization developed in 7 eyes (13%) of the study patients. RPE atrophy was found in 1 eye (2%) of the subtenon group at 24 months. No case of RPE tear, infectious complication, retinal detachment or cardiovascular complication was noted over the 36-month follow-up period. Currently, little is known of (a) the changes in visual acuity and structural characteristics of PED over time following introduction of TA into the eye, (b) factors influencing the efficacy of TA in the treatment of this disorder and the risk of developing complications, (c) prognosis for late outcomes of TA treatment in serous PED in a long-term follow-up. In the controlled trial of argon laser photocoagulation in PEDs in the elderly [16, 17], a reduction in VA was noted in 27 patients (27 eyes) of the untreated group at 9 months. Control eyes continued to show gradual but progressive visual loss at the following visits. At 3 years, a visual loss of 0.25 (or 2.42 Snellen lines) was observed in 19 (86%) of untreated eyes, and 14% of control eyes remained stable compared to the baseline values. In addition, in 22 patients (22 eyes) with PED treated with laser photocoagulation, visual loss was noted as early as 3 months. Although that study showed a reduction in PED in most of the treated eyes, their VA continued to decrease, and, at 36 months, a visual loss of 2.93 Snellen lines was found in 15 treated eyes (75%), and 15% of treated eyes remained stable compared to the baseline values [16, 17]. Over the course of our study, visual acuity in both arms of the study remained stable compared to the baseline values. In 2001, Gomez-Ulla and colleagues [2] reported that at 25 months, out of 11 eyes treated with diode laser photocoagulation for RPE detachment, 6 eyes (55%) improved or stabilized VA, and the rest showed no change in VA. De Jong [18] and Ho and colleagues [19] demonstrated that laser photocoagulation did not result in improvement in vision in patients with serous PED associated with AMD. PDT is not used in patients with avascular serous PED associated with AMD. However, PDT for CNV associated with PED in AMD has been shown to result in decreased visual function. Thus, Pece and colleagues demonstrated that in eyes with CNV at the edge of PED treated with PDT, the mean preoperative visual acuity changed from 20/80 (0.60 ± 0.33 logMAR) to 20/126 (0.80 ± 0.64 logMAR) at month 18. The authors of that study believe that this was caused by post-PDT complications (subretinal hemorrhage, increase in RPE detachment and RPE tears) [20]. Subsequently, Ladas and colleagues [21] demonstrated a statistically significant visual loss of at least 3 lines following PDT for CNV associated with PED (of at least 1 disc diameter in size) in AMD in 77.3% of eyes at the completion of follow-up (12 to 48 months) [21]. According to Panos et al [6], Kook et al [7], and Lommatzsch and co-authors [22], the use of angiogenesis inhibitors (bevacizumab and ranibizumab) in serous PED results in stabilization of visual acuity over the entire period of treatment; however, the use of anti-VEGF agents for this purpose is associated with high risk of RPE tear which may be followed by a sudden and irreversible loss of vision. In the study presented here, complete re-attachment of the RPE was observed in 20 eyes (37%) treated with TA over the 36-month follow-up period, and the reattachment rate in the intravitreal group was 36.4% (8 eyes out of 22) versus 37.5% (12 eyes out of 32) in the subtenon group. At the final follow-up time point, there was no significant difference in the reattachment rate between the two administration arms (P = 0.9). However, the number of injections needed was statistically significantly higher for subtenon TA treatment than for intravitreal TA treatment of serous PED associated with AMD. Some authors [20, 23, 24] believe that the initial size of PED is an important prognostic factor. Thus, Lasic and Gabric [24] have reported on the outcomes of intravitreal bevacizumab treatment of 102 patients with RPE detachment associated with AMD, with median duration of follow-up of 18 weeks, and finding of direct correlation between the baseline PED height and treatment outcome. In addition, they found that the anti-VEGF agent was of low efficacy in patients with a high pre-injection PED [24]. During the course of our study of PED treatment with TA, we found no cases of RPE tear. This is an evidence for the pathogenetic validity of the use of TA monotherapy for serous PED. The formation of SNM was another type of ocular adverse events evaluated in our study. During the 36-month observation period, SNM developed in 7 eyes out of 54 (13%), including 4/22 (18%) eyes of the intravitreal group and 3/32 (18%) eyes of the subtenon group, with no significant intergroup difference (P = 0.34). It is noteworthy that the first case of SNM formation in our study was observed as late as month 30. During the 3-year observation period in the study conducted by the Moorfields macular study group, SNM developed in 10 (45%) untreated eyes with PED, which is 35% higher than the rate in our study (95% CI = 12.4 to 55.6; P = 0.004). In addition, SNM developed in 8 (40%) eyes treated with laser photocoagulation for PED, which is 25% higher than that in the use of TA for this disorder (95% CI = 3.4 to 47.5; P = 0.04) [17]. It is noteworthy that the first SNM formation event in untreated patients of that study was noted at month 18 [17]. Therefore, in our study, in patients treated with TA, subretinal neovascular membrane developed 2 years later compared to treatment-na?ve patients. To the best of our knowledge, no case of SNM development in serous PED treated with PDT and intravitreal anti-VEGF agents has been reported [25, 26]. Therefore, in our study, SNMs developed in 13% of treated eyes, with the first case of SNM formation observed as late as month 30, which is substantially less frequently and later than in other studies. In the study reported by the Moorfields macular study group [17], by month 36, RPE atrophy was found in 5 (23%) untreated eyes with PED, and in 10 (50%) eyes treated with laser photocoagulation for PED, while in our study, geographic RPE atrophy was found in 1 (2%) eye treated with TA for PED at month 36. Siqueira and colleagues [27] and Miura and Roiter [28] have demonstrated in their in vivo and in vitro experimental studies that long-acting steroids strengthen intercellular bonds in the RPE, resulting in decreased permeability of cellular membranes. This contributes to protection of RPE cells from oxidative injury followed by cell destruction [27, 28]. We hypothesize that retina protective effect of TA accounts for the low values of the rate of RPE atrophy development in serous PED associated with AMD in our study. Therefore, this confirms the pathogenetic validity of the use of TA monotherapy for serous PED. At the final follow-up time point, no significant difference in visual acuity, and percentages of eyes with re-attachment of the RPE, RPE tears, formations of SNM, or RPE atrophy events between the two administration arms of triamcinolone acetonide was observed. Therefore, the route of administration of TA did not influence the efficacy of TA therapy. Conclusion Intravitreal and subtenon TA injection therapy have similar efficacy in serous retinal pigment epithelial detachment associated with age-related macular degeneration, and contribute to the maintenance of visual acuity throughout 36 months. We found significant reductions in the height and length of pigment epithelial detachment in patients who received intravitreal TA (from 486 (187) µm to 256 (139) µm, P = 0.005; and from 1859 (911) µm to 1112 (451) µm, P = 0.04, respectively) and in those who received subtenon TA (from 446 (199) µm to 231 (107) µm, P = 0.0001; and from 2055 (587) µm to 1423 (465) µm, P = 0.02, respectively). Complete re-attachment of the RPE was achieved in 37% of eyes treated with TA. Irrespective of the route of administration, TA therapy allowed us to prevent RPE tears in patients with serous retinal pigment epithelial detachment associated with age-related macular degeneration throughout the 36-month follow-up period. It was established that, in patients treated with TA, subretinal neovascular membrane develops 2 years later compared to treatment-na?ve patients. References 1.Pasyechnikova NV, Korol AR. [Clinical classification and tactics of management of patients with age related macular degeneration]. Oftalmol Zh. 2010;2:38-41 Russian 2.Gomez-Ulla F, Gonzalez F, Abelenda D, et al. Diode laser photocoagulation of choroidal neovascularization associated with retinal pigment epithelial detachment. Acta Ophthalmol Scand. 2001 Feb;79(1):39-44 3.Axer-Siegel R, Ehrlich R, Rosenblatt I, et al. Photodynamic therapy for occult choroidal neovascularization with pigment epithelial detachment in age-related macular degeneration. Arch Ophthalmol. 2004 Apr;122(4):453-9 4.Gelisken F, Inhoffen W, Partsch M, et al. Retinal pigment epithelial tear after photodynamic therapy for choroidal neovascularization. Am J Ophthalmol. 2001 Apr;131(4):518-20 5.Boguszakova? J, Dubska? Z. Tears of the retinal pigment epithelium. Cesk Slov Oftalmol. 2001;57:367-71 6.Panos GD, Gatzioufas Z, Petropoulos IK, et al. Effect of ranibizumab on serous and vascular pigment epithelial detachments associated with exudative age-related macular degeneration. Drug Des Develd Ther. 2013 Jul 10;7:565-9 7.Kook D, Wolf A, Neubauer AS, et al. [Retinal pigment epithelial tears after intravitreal injection of bevacizumab for AMD. Frequency and progress]. Ophthalmologe. 2008 Feb;105(2):158-64 German 8.Suk SA, Saksonov SG, Kuznetsova TA. [Use of posterior subtenon injection combined with transpupillary thermotherapy for subfoveal choroidal neovascularization associated with age-related macular degeneration]. Oftalmol Zh. 2008;3:19-22 Russian 9.Axer-Siegel R, Ehrlich R, I. Avisar I, et al. Combined photodynamic therapy and intravitreal triamcinolone acetonide injection for neovascular age-related macular degeneration with pigment epithelial detachment. Ophthalmic Surg Lasers Imaging. 2006 Nov-Dec;37(6):455-61 10.el Matri L, Chebil A, Kort F, et al. Intravitreal injection of triamcinolone combined with bevacizumab for choroidal neovascularization associated with large retinal pigment epithelial detachment in age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2010 Jun;248(6):779-84 11.Levitska GV, Putienko AA. Abdulkhadi Mukhammad. [Features of changes in IL-6 and TNF in patients with RRD associated with vitreous detachment after intravitreal injection of triamcinolone acetonide]. [Issues of environmental and medical genetics and clinical ophthalmology]. 2005 5:61-70 Russian 12.Ozdemir H, Karacorlu S, Alacali N, et al. Intravitreal triamcinolone as a primary therapy in diabetic macular oedema. Eye. 2005;19:382–6 13.Ozdek S, Deren YT, Gurelik G, et al. Posterior subtenon triamcinolone, intravitreal triamcinolone and grid laser photocoagulation for the treatment of macular edema in branch retinal vein occlusion. Ophthalmic Res. 2008;40(1):26-3 14.Toda J, Fukushima H, Kato S. Injection of triamcinolone acetonide into the posterior sub-tenon capsule for treatment of diabetic macular edema. Retina. 2007 Jul-Aug;27(6):764-9 15.Pasyechnikova NV, Naumenko VA, Korol AR, et al. Serous Pigment epithelial detachment Associated with Age-Related Macular Degeneration: A Possible Treatment Approach. Med Hypothesis Discov Innov Ophthalmol. 2012 Winter;1(4):72-5 16.Barondes MJ, Pagliarinit S, Chisholm IH, et al. Controlled trial of laser photocoagulation of pigment epithelial detachments in the elderly: 4 year review. Br J Ophthalmol. 1992;76(1):5-7 17.Moorfields macular study group. Retinal pigment epithelial detachments in the elderly: a controlled trial of argon laser photocoagulation. Br J Ophthalmology. 1982 Jan; 66(1): 1–16 18.de Jong PT. Laser treatment of central serous chorioretinopathy, of pigment epithelial detachments and of subretinal neovascularizations in senile disciform macular degeneration. Bull Soc Belge Ophtalmol. 1981;197:55-61 19.Ho PC, Namperumalsamy P, Pruett RC. Photocoagulation of serous detachments of the retinal pigment epithelium in patients with senile macular disease. Ann Ophthalmol. 1984 Mar;16(3):213-8 20.Pece A, Isola V, Vadala M, et al. Photodynamic therapy with verteporfin for choroidal neovascularization associated with retinal pigment epithelial detachment in age-related macular degeneration. Retina. 2007 Mar;27(3):342-8 21.Ladas ID, Kotsolis AI, Rouvas AA, et al. Efficacy of photodynamic therapy in the management of occult choroidal neovascularization associated with serous pigment epithelial detachment. Ophthalmologica. 2007;221(5):313-9 22.Lommatzsch A, Heimes B, Gutfleisch M, et al. Serous pigment epithelial detachment in age-related macular degeneration: comparison of different treatments. Eye (Lond). 2009 Dec;23(12):2163-8 23.Ritter M, Bolz M, Sacu S, et al.Effect of intravitreal ranibizumab in avascular pigment epithelial detachment. Eye (Lond). 2010 Jun;24(6):962-8 24.Lazic R, Gabric N. Intravitreally administered bevacizumab (Avastin) in minimally classic and occult choroidal neovascularization secondary to age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2007 Jan;245(1):68-73 25.Huddad WM, Coscas G, Soubrane G. Eligibility for treatment and angiographic features at the early stage of exudative age related macular degeneration. Br J Ophthalmol. 2002 Jun;86(6):663-9 26.Pauleikhoff D, L?ffert D, Spital G, et al. Pigment epithelial detachment in the elderly. Clinical differentiation, natural course and pathogenetic implications. Graefes Arch Clin Exp Ophthalmol. 2002 Jul;240(7):533-8 27.Siqueira RC, dos Santos WF, Scott IU, et al. Neuroprotective effects of intravitreal triamcinolone acetonide and dexamethasone implant in rabbit retinas after pars plana vitrectomy and silicone oil injection. Retina. 2015 Feb;35(2):364-70 28.Miura Y, Roider J. Triamcinolone acetonide prevents oxidative stress-induced tight junction disruption of retinal pigment epithelial cells. Graefes Arch Clin Exp Ophthalmol. 2009 May;247(5):641-9
|