J.ophthalmol.(Ukraine).2022;1:73-76.
|
http://doi.org/10.31288/oftalmolzh202217376 Received: 25 February 2021; Published on-line: 15 March 2022 Trabeculoplasmy, a new surgical technique in the treatment of glaucoma: pilot report Leopoldo Garduño Vieyra, Raúl Rúa Martínez, Verónica Muñoz Cornejo, Héctor Bello López Portillo Clínica Oftalmología Garduño; Irapuato, Guanajuato (México) E-mail: ruamartinez@yahoo.es TO CITE THIS ARTICLE: Leopoldo Garduño Vieyra, Raúl Rúa Martínez, Verónica Muñoz Cornejo, Héctor Bello López Portillo. Trabeculoplasmy new surgical technique in the treatment of glaucoma: pilot report. J.ophthalmol.(Ukraine).2022;1:73-6. http://doi.org/10.31288/oftalmolzh202217376 The effectiveness of trabeculoplasmy in lowering intraocular pressure (IOP) in glaucoma patients was determined. A longitudinal study was carried out in 10 patients with open-angle glaucoma that underwent trabeculoplasmy. The postoperative results Of IOP, visual acuity (VA) and the occurrence of complications were evaluated at 24 hours, one week, 3, 6, 9 and 12 months. 10 surgeries were performed (10 eyes, 10 patients). Preoperative average IOP was 32.5mmHg and preoperative VA was 0.5. At one year the average IOP was 10.10 mmHg and the average VA was 0.7, both values were significant (p<0.001, p=0.019 respectively). Trabeculoplasmy may be effective technique in the treatment of glaucoma, providing a decrease and maintenance of IOP within normal limits after one year of follow-up. Key words: glaucoma, intraocular pressure, surgery, trabeculoplasmy
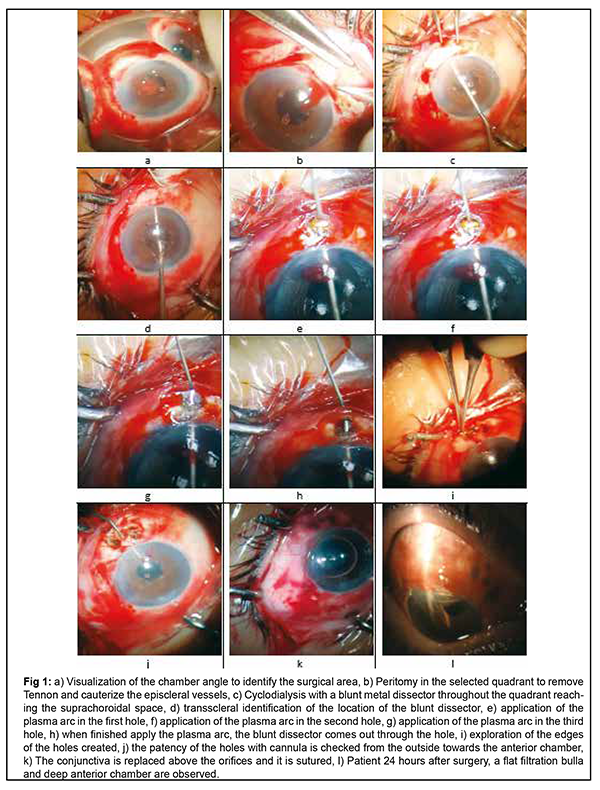
Introduction. Despite the fact that many techniques have been described in the treatment of glaucoma, it continues to be a visual problem worldwide. Even more so in developing countries where access to specialized services continues to be a barrier [1]. With trabeculectomy, the expected results are not always achieved, which is why glaucoma surgery is always evolving towards more effective, less invasive and more accessible techniques [1]. New instruments are also required. This is how the “Fugo Blade” plasma scalpel (MediSURG M100, Indianapolis, USA) arose, which has been very useful in modern glaucoma surgery [1]. The plasma scalpel, like the excimer laser, works by plasma energy ablating the tissue. When using this instrument, the plasma arc that is generated at the same time creates a wall around the incision that produces hemostasis. The temperature generated does not extend beyond the incision site so it does not affect nearby structures [2]. The advantage of plasma technology in glaucoma surgery is that the ablation power that is generated allows the filtration paths to be performed in a wide variety of ways, meeting the needs of the surgeon and the specificities of the patient [2, 3]. The Fugo Plasma Blade console and its disposable tips can be expensive [3]. this is why a more economical device, the Plasma Pen Liss KC6 (Kiyalaser, Guangdong, China) with 23G disposable needles, was used in this study. The equipment used was the Plasma Pen Liss KC6 (Kiyalaser). This equipment has been used with excellent results in skin diseases, allowing to eliminate flat warts, pigmented nevi, syringomas, corns, skin neoplasms, among other conditions. In the eyes it has been used to lift droopy upper eyelids, remove excess skin, correct asymmetry in eyebrows, reduce excess skin on lower eyelids, reduce expression lines such as crow's feet and frown, reduce stretch marks and scars. In this way we achieve greater accessibility to the use of this technology in glaucoma surgery, favoring our patients. Methods A longitudinal study was carried out that included 10 patients. Elderly, pseudophakic patients with a diagnosis of open-angle glaucoma and without a favorable response to combined ocular antihypertensive therapy were recruited. The glaucoma damage was quantified using the HPA classification system. 5 Early defects were present in 3 patients, moderate defects in 5 patients and only 2 patients had severe defects. All patients were treated for at least 6 months with the same antihypertensive therapy. It was Dorzolamide-Timolol-Brimonidine (two times a day) and latanoprost (one time a day). An unfavorable response was defined when, after 6 months with maximal combined antihypertensive ocular therapy, optic neuropathy continued to progress and corrected IOP levels below 21 mmHg were not reached. The IOP was measured by an ophthalmology (not related with this study) using a Goldmann tonometer. The patients attended Garduño Ophthalmology Clinic (Irapuato, Guanajuato, Mexico), and complying with the ethical standards of the clinic, gave their written consent for the surgery performed. The plasma technology in glaucoma surgery had been proven before. The new surgical technique was tested first on pig eyes for 3 months. Once skill was achieved, the study was carried out. Surgical technique Description of the surgical technique: - Peribulbar anesthesia is applied with a proportional mixture of lidocaine 2% and bupivacaine 0.5%, after asepsis and antisepsis. - Corneal incision in temporal sector with 15º knife for work port. Visco-elastic instillation in the anterior chamber to open the angle in its greatest proportion. - To use the gonioscope or 3-mirror lens, we apply sodium hyaluronidate on the cornea. By visualizing the angle in the upper nasal quadrant, we identify the area where we will work. - Peritomy in the upper nasal quadrant to remove Tenon's capsule and to cauterize the episcleral vessels. We also apply a 0.2 mg/ml Merocel Mitomycin C sponge for 5 minutes. - We introduce a blunt metal dissector, through the paracentesis performed previously, until reaching the angle in the upper nasal quadrant. Here, a cyclodialysis is performed in the extension of this entire quadrant, dissecting the suprachoroidal space with a depth of 10 to 15 mm. - In this quadrant, with the dissector 6 to 9 mm posterior to the sclerocorneal limbus, the sclera is slightly pushed to identify its transscleral location from the outside. - At this time, the plasma arc (Plasma Pen with 23G disposable needles) is applied to the sclera raised internally by the dissector, until the dissector is visualized externally. Three 2-mm holes are made in this quadrant, and its walls are immediately coagulated. - The permeability of these holes is immediate. They are covered by putting the conjunctiva in place and suturing it with 8-0 vicryl. This results in a long, flat filter bleb. - Finally, a mixed ointment is applied and the eye is occluded for 24 hours. The patients underwent a postoperative follow-up in consultation at 24 hours, 1 week and 3, 6, 9 months until one year. In each consultation, a slit lamp examination was performed to detect complications, taking the intraocular pressure (IOP) and the best-corrected visual acuity (BCVA). To evaluate the results of the surgeries, the statistical technique of t-test was used for means of two paired samples. Complications were quantified and described. Female sex predominated in patients, and age ranged from 41 to 50 years. Results The mean intraocular pressure (MIOP) of the patients before surgery was 32.50 mmHg (range 26-43mmHg). Postoperatively at 24 hours, the MIOP decreased to 3.30mmHg (range 2 to 5mmHg). In subsequent consultations, it remained within acceptable limits and one year after the procedure the PIOP was 10.10 (range 7 to 15mmHg, significance p <0.005) (Table 1).
The mean best corrected visual acuity (MBCVA) of the patients before surgery was 0.5 according to the Snellen chart (range 0.1 to 1.0). Postoperatively at 24 hours, MBCVA decreased only one line in one patient (range 0.2-0.8). At postoperative visits, there was no decrease in MBCVA except in one patient, and some patients improved their vision. At one year the MBCVA was 0.7 (range 0.3 to 1.0, significance p <0.05). One year after surgery (12 months consultation) all patients maintain a long and flat filter bleb. The success of this technique lies in extensive cyclodialysis, non-clogging conduits, and a large, flat filtration tube (fig. 1).
There were complications in 3 patients. One patient with 2 mm hyphema and two with mild anterior uveitis. These were treated in the postoperative consultations and did not compromise the final result of the surgery. Discussion Trabeculoplasmy is a novel technique that allows conventional glaucoma surgery to be performed using the plasma arc. Although there was a history of the use of the Fugo Plasma Blade [2, 3]; in this case it is not used and is replaced by a Plasma Pen with disposable 23G needle tips. Singh et al. reported the effectiveness of surgery in absolute glaucoma with the use of plasma. A 6-month follow-up demonstrated safety and effectiveness similar to conventional trabeculectomy. There was a reduction in IOP by more than 80% [4, 6]. Trabeculectomy is the "gold standard" procedure in glaucoma surgery. This has been modified and significant progress has been made, all with the aim of minimizing the risk of complications and surgical failure [7]. In conventional trabeculectomy, a sudden decrease in IOP is reported in the first days, which could lead to early hypotonia and various associated complications such as hyphema, atalamia, and uveal effusion [7]. In trabeculoplasmy, the deep anterior chamber and the risk of bleeding in the anterior chamber is greatly reduced by the fact that the plasma arc simultaneously coagulates the tissue where it is applied. One year after trabeculectomy, a decrease in VA compared to preoperative in more than one line of sight in the Snellen chart has been reported in 15-18.8% of patients [7]. In this study only one patient had a decrease in VA of a line on the Snellen chart and was associated with an atrophic maculopathy in both eyes. The training curve for conventional trabeculectomy is well established and easy to learn. Trabeculoplasmy presents a similar curve and can also be developed experimentally in its early stages [8]. In this case, it was started in the eyes of pigs until it was certain that all surgical parameters had been controlled. With the use of the Plasma Pen it was possible to apply plasma technology in glaucoma surgery without excessive costs. In this way, low-income populations can be accessed, allowing them optimal results [4]. In a meta-analysis article published in 2017, the need for more rigorous clinical studies of minimally invasive glaucoma surgery was evidenced. It refers that, although the effectiveness in reducing IOP, the non-need for the use of antiglaucoma drugs and the safety of the procedure are demonstrated, these results come from most descriptive (non-comparative) studies [9]. This longitudinal study constitutes the point of departure for a larger randomized clinical trial with a larger number of patients. Conclusions Trabeculoplasmy could be an effective technique in the treatment of glaucoma, offering a reduction and maintenance of pressure within normal limits after one year of follow-up. References https://vision2020la.wordpress.com/2013/03/26/terapias-alternativas-para... 2.Daljit S. Fugo Blade effective tool for multiple surgical applications. Eurotimes 2008. Disponible en: http://www.escrs.org/Publications/Eurotimes/08June/FugoBladeeffective.pdf 3.Fry Luther L.The Pros and Cons of the Fugo Plasma Blade. Cataract and Refractive Surgery Today. 2007. Disponible en: https://crstoday.com/articles/2007-oct/crst1007_19-php/ 4.Dow CT, de Venecia G. Transciliary filtration with the Fugo plasma blade. Ann Ophthalmol (Skokie) 2008:40(1):8-14. 5.Susanna R Jr, Vessani RM. Staging glaucoma patients: why and how? Open Ophthalmol J 2009;3:59-64. 6.Singh D, Bundela RA, Agarwal A, Bist HK, Satsangi SK. Goniotomy ab interno “a glaucoma filtering surgery” using the Fugo Plasma Blade. Ann Ophthalmol (Skokie) 2006;38(3):213-7. 7.Jankowska-Szmul J, Dobrowolaki D, Wylegala E. CO2 laser-assisted sclerectomy surgery compared with trabeculectomy in primary open-angle glaucoma and exfoliative glaucoma. A 1-year follow-up. Acta Ophthalmol. 2018:96:e582-e591. 8.Roy H, Singh D, Fugo RJ. Ocular applications of the Fugo Blade. 1ra edición. Philadelphia: Lippin Cott Williams and Wilkins; 2011. 9.Lavia C, Dallorto L, Maule M, Ceccarelli M, Fea AM (2017) Minimally-invasive glaucoma surgeries (MIGS) for open angle glaucoma: A systematic review and meta-analysis. PLoS ONE12(8): e0183142.
Authors do not have conflict of interest in this article.
|