J.ophthalmol.(Ukraine).2022;3:54-57.
|
http://doi.org/10.31288/oftalmolzh202235457 Receieved: 17.02.2022; Accepted: 06.06.2022; Published on-line 15.06.2022 Managing proliferative diabetic retinopathy in a patient with vitreous hemorrhage: a case report O. B. Koshchynets, R. L. Vadiuk Ivano-Frankivsk National Medical University; Ivano-Frankivsk (Ukraine) TO CITE THIS ARTICLE:Koshchynets OB, Vadiuk RL. Managing proliferative diabetic retinopathy in a patient with vitreous hemorrhage: a case report. J.ophthalmol.(Ukraine).2022;3:54-7. http://doi.org/10.31288/oftalmolzh202235457 We report a case of successful treatment of a 35-year-old patient diagnosed with severe type 1 diabetes mellitus with moderate glycemic control, bilateral proliferative diabetic retinopathy and total vitreous hemorrhage in the right eye. At baseline, there was optical coherence tomography angiography and fundus photography evidence of significant neovascularization of the optic nerve and peripapillary retina along the vessels. Although Ukrainian guidelines on the use of aflibercept do not mention retinal neovascularization in diabetic retinopathy in the absence of diabetic macular edema as an indication for the use of aflibercept, we relied on the experience of foreign colleagues and the eye without hemorrhage was treated with five monthly loading injections of intreavitreal aflibercept 0.05 ml, and, after the first year, treatment was continued according to a “treat and extend” strategy. The case reported demonstrated that intravitreal aflibercept in combination with panretinal laser photocoagulation is effective for regression of neovascularization and prevention of recurrent vitreous hemorrhage. Keywords: proliferative diabetic retinopathy, neovascularization, intravitreal injection, ant-VEGF agents
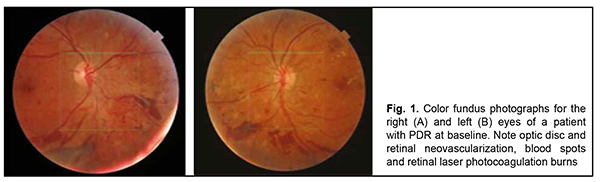
Introduction Diabetes mellitus (DM) causes a huge medical, social and economic burden on the society due to an increasing prevalence of the disease and its vascular complications [1-3, 5, 12]. According to diabetes burden research by the International Diabetes Federation, it was estimated that there were 451 million (age 18-99 years) people with diabetes worldwide in 2017. These figures were expected to increase to 693 million by 2045 [8]. Diabetes mellitus is a systemic disease characterized by microvascular complications. Of these, diabetic retinopathy (DR) is one carrying the most unfavorable prognosis. Proliferative diabetic retinopathy (PDR) is the most severe form of diabetic eye disease [1]. Increased vitreous vascular endothelial growth factor (VEGF) concentration plays a key role in the pathogenesis of both PDR and macular edema [7]. The neovascularization seen on the fundus has been described as new vessels elsewhere (NVE) when located away from the optic disc, and as new vessels on the disc (NVD) when either on the optic disc or within 1 disc diameter of its margin [13]. PDR is less common in type 2 DM than in type 1 DM. PDR prevalence was 60% for patients type 1 DM and disease duration of 20 years, and 20% for patients type 2 DM and disease duration of 20 years. PDR is equally common in men and women, with its incidence peaking at the age of 60 and decreasing thereafter [5]. Diabetic retinopathy is dangerous because it cannot be identified in early stages. Patients with early DR and even those with PDR in the absence of diabetic macular edema (DME) or hemorrhage in the macula will not note decreased vision [5]. Vitreous hemorrhage is one of the two most frequent vision-threatening perioperative and postoperative complications of DR [15]. It is noteworthy that vitreous hemorrhage makes it difficult to perform postoperative monitoring of the fundus and affects reparative processes [4]. Timely laser photocoagulation and/or ant-VEGF treatment for severe PDR, particularly in the presence of DME, can prevent further visual loss [3]. Others confirmed that laser photocoagulation is still effective for visual loss but does not improve DME. Laser photocoagulation is also aimed at retinal ischemic areas, suppression of neovascularization and obliteration of vessels with increased permeability [2, 3]. Only complex surgery may be effective for late DR. Despite recent advances in vitrectomy techniques, there is still a risk of surgical complications related to vitrectomy, including retinal detachment, cataract, neovascular glaucoma, and postoperative infectious disease [3, 16]. However, the advent of anti-VEGF agents has changed the paradigm of treatment for neovascularization, with these agents acting on the major pathophysiologic phase of DR. At present, ranibizumab (Lucentis, Novartis, Basel Switzerland) and aflibercept (Eylea®, Bayer, Leverkusen, Germany) are the most commonly used anti-VEGF agents for DME [5]. The efficacy and safety of local anti-VEGF therapy for DR has been demonstrated by international multicenter clinical trials [8, 11]. Intravitreal anti-VEGF injections enable targeted delivery to specific tissues and minimize adverse systemic effects The purpose of this study was to report a case of aflibercept treatment for diabetic PDR in a patient with vitreous hemorrhage in the fellow eye. Material and Methods A 35-year-old patient treated as an in-patient for severe type 1 diabetes mellitus with moderate glycemic control at Endocrinology department was under our observation. He underwent a scheduled eye examination as per the protocol for type 1 diabetes mellitus, including visual acuity, intraocular pressure (IOP), ophthalmoscopy, biomicroscopy, fundus fundus photography and optical coherence tomography angiography (OCTA). In addition, he underwent general clinical tests and neurological, endocrinological and nephrological assessments as per the protocol for type 1 diabetes mellitus. Fundus photography was performed and OCTA imaging was performed using the Triton (Topcon, Tokyo, Japan) to assess the presence and severity of the retinal and optic nerve neovascularization at 1, 6 and 9 months. Aflibercept is a recombinant fusion protein containing VEGF-binding domain of VEGF receptors 1 and 2, fused to the FC portion of the human IgG1 immunoglobulin. Similar to bevacizumab and ranibizumab, aflibercept binds all isoforms of VEGF-A; however, it also binds VEGF-B and placental growth factors [1, 14]. Results The patient reported that he had been treated by an ophthalmologist and had bilateral retinal laser photocoagulation. At presentation, visual acuity OU was 1.0. Color fundus photographs of the patient with PDR before treatment are presented in Fig. 1.
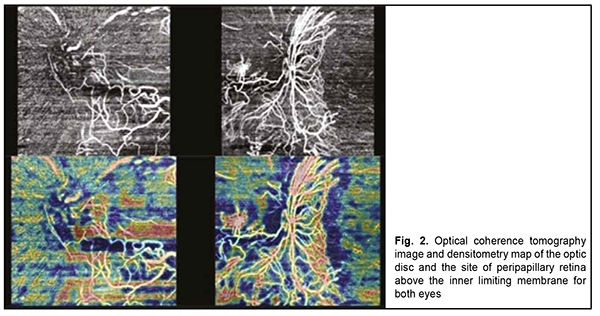
OCT and densitometry map showed more apparent signs of neovasculatization in the left eye than in the right eye (Fig. 2), and, consequently, the patient was planned initially to receive intravitreal aflibercept OS, and than intravitreal aflibercept OD.
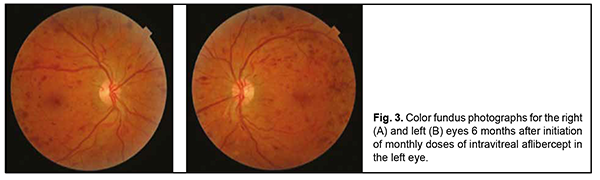
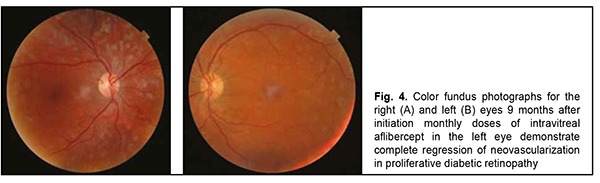
However, several days before the planned procedure, the patient complained of abruptly decreased vision in the right eye. At presentation to the Eye Microsurgery Department on December 12, 2019, visual acuity OD was hand motion. Slit lamp examination OD showed a quiet and non-painful eye, no change in the anterior segment, mild lens opacification, and total vitreous hemorrhage. There was no view to the fundus. Visual acuity OS was 1.0. Slit lamp examination OS showed a quiet and non-painful eye, no change in the anterior segment, and transparent media. Fundus examination OS showed a pale pink optic disc with clear margins, neovascularization, and physiological cupping. In addition, retinal arteries were narrowed and veins dilated, there was a stroke on the retina, and epiretinal and preretinal hemorrhage. On November 11, 2019, blood glucose level was 7.7 mmol/L, and glycated hemoglobin, 8.2%. On the basis of clinical examination, the patient was diagnosed with PDR with optic disc and retinal neovascularization OU, and total vitreous hemorrhage OD. In addition, he was diagnosed with severe type 1 diabetes mellitus and moderate glycemic control. The treatment was initiated with prevention of complications associated with primary total vitreous hemorrhage. In the right eye, a subtotal pars plana vitrectomy with endolaser photocoagulation and gas-air mixture tamponade was performed. Although this operation is more traumatic to the eye than intravitreal injection, it was effective. Two weeks after surgery, uncorrected visual acuity OD was 0.5, and best-corrected visual acuity OD, 0.9. No improvement in neovascularization was observed after the patient received three courses of 232-nm diode laser panretinal photocoagulation OS as per the protocol for managing patients with PDR. This was followed by treatment of the left eye with intravitreal aflibercept which was administered on an off-label basis as per the 2018 Euretina Expert Consensus Recommendations on intravitreal injections and American Diabetes Association recommendations [10, 11] (aflibercept is registered in Ukraine, but Ukrainian guidelines on the use of aflibercept do not mention retinal neovascularization in diabetic retinopathy in the absence of diabetic macular edema as an indication for the use of aflibercept). The patient received five monthly intravitreal aflibercept injections 0.05 ml. The operation and postoperative period were uneventful. Studies [6, 10] have demonstrated that intravitreal aflibercept provides a chance for improvement to most patients with decreased vision, with a reduction in the number of injections needed after month 12 of therapy. Treatment efficacy was assessed at 6 months and 9 months after initiation of treatment (Figs 3 and 4). At these time points, visual acuity OU was 0.9, and there was ophthalmoscopic and OCT evidence of regression of retinal and optic nerve neovascularization.
There was also evidence of regression of retinal and optic nerve neovascularization at 24 months after initiation of treatment. In addition, there was no evidence of vitreous hemorrhage during the postoperative period and at 6-month and 9-month follow-up examinations. After the first year, treatment was continued according to a “treat and extend” strategy, the patient required and received a single injection from month 12 to month 24, and was recommended to have further follow-up on the outpatient basis. Conclusion Each type of fundus changes requires an individualized approach to treatment. A wide variety of surgical techniques is available for treating diabetic retinopathy; however, adequate treatment selection and close cooperation between the ophthalmologist and endocrinologist are prerequisites for positive treatment outcome and prevention of neovascularization. The case reported demonstrated that intravitreal aflibercept in combination with panretinal laser photocoagulation are effective for regression of neovascularization and prevention of recurrent vitreous hemorrhage.
References 1.Abdulaeva EA, Minkhuzina EL, Kuskov AN. [Anti-VEGF therapy for proliferative diabetic retinopathy: translating research evidence into clinical practice]. Russian Journal of Clinical Ophthalmology. 2020;20(2):97–103. 2.Demidova TYu, Trakhtenberg YuA. [Current approaches to the management of diabetic retinopathy]. Diabetes mellitus. 2014;17(3):122-8. Russian. 3.Bikbov MM, Fayzrakhmanov RR, Zaynullin RM, et al. [Macular edema as a manifestation of diabetic retinopathy]. Diabetes mellitus. 2017;20(4):263-9. Russian. 4.Lytvynenko SS. [Vitreous hemorrhage after surgical treatment of diabetic retinopathy in patients with type 2 diabetes]. 2021;9(3):15-21. 5.Seidinova ASh, Ishigov IA, Seidinova ASh, et al. [Incidence of retinopathy in diabetic patients based on the data from the Diabetes Research Center]. Vestnik Kaz NMU. 2017;1:328-30. 6.Alagorie AR, Velaga S, Nittala MG, Yu HJ, Wykoff CC, Sadda SR. Effect of Aflibercept on Diabetic Retinopathy Severity and Visual Function in the RECOVERY Study for Proliferative Diabetic Retinopathy. Ophthalmol Retina. 2021 May;5(5):409-19. 7.Brooks HL Jr, Caballero S Jr, Newell CK, et al. Vitreous levels of vascular endothelial growth factor and stromal-derived factor 1 in patients with diabetic retinopathy and cystoid macular edema before and after intraocular injection of triamcinolone. Arch Ophthalmol. 2004 Dec;122(12):1801-7. 8.Cho NH, Shaw JE, Karuranga S, et al. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018 Apr;138:271-81. 9.Do DV, Schmidt-Erfurth U, Gonzalez VH, et al. The DA VINCI study: phase 2 primary results of VEGF trap-eye in patients with diabetic macular edema. Ophthalmology. 2011 Sep;118(9):1819-26. 10.Microvascular Complications and Foot Care: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018 Jan;41(Suppl 1):S105-S118. doi: 10.2337/dc18-S010. 11.Grzybowski A, Told R, Sacu S, et al. Update on Intravitreal injections: Euretina expert consensus recommendations. Ophthalmologica. 2018;239(4):181-193. 12.Heidemann C, Paprott R, Stühmann LM, et al. Perceived diabetes risk and related determinants in individuals with high actual diabetes risk: results from a nationwide population-based survey. BMJ Open Diabetes Res Care. 2019. 7(1). e000680. 13.Schmidt-Erfurth U, Garcia-Arumi J, Bandello F, et al. Guidelines for the Management of Diabetic Macular Edema by the European Society of Retina Specialists (EURETINA). Ophthalmologica. 2017;237:185-222. 14.Stewart MW. The expanding role of vascular endothelial growth factor inhibitors in ophthalmology. Mayo Clin Proc. 2012 Jan;87(1):77-88. 15.Taskintuna I, Elsayed ME, Taskintuna K, et al. Comparison of outcomes of four different treatment modalities for diabetic vitreous haemorrhage. Sci Rep. 2020 Feb 28;10(1):3674. 16.Yanoff M, Duker JS. Vitrectomy. In: Ophthalmology. 3rd ed. St Louis, MO: Mosby Elsevier;1999. p.533. Disclosures Corresponding Author: Koshchynets Olesia, email: okoshchynets83@gmail.com Author contribution: Vadiuk R.L.: conservative and surgical treatment of the patient, concept and editing; Vadiuk R.L., Koshchynets O.B.: the idea of publishing and editing the article; Koshchynets O.B.: literature analysis and article formation. Conflict of Interest: The authors state that there is no conflict of interest that could affect their opinion on the topic or material presented in the manuscript. Abbreviations: DM – diabetes mellitus; DR– diabetic retinopathy; PDR – proliferative diabetic retinopathy; VEGF – vascular endothelial growth factor; NVE – new vessels elsewhere; NVD – new vessels on the disc; DME – diabetic macular edema; IOP - intraocular pressure, ОСТА – optical coherence tomography angiography.
|