J.ophthalmol.(Ukraine).2022;2:32-36.
|
http://doi.org/10.31288/oftalmolzh202223236 Received: 24 November 2021; Published on-line: 30 April 2022 Clinical features of symptomatic acquired lacrimal outflow obstruction in patients with type 2 diabetes mellitus P. A. Bezditko ¹, N. M. Bezega ² 1 Kharkiv National Medical University; Kharkiv (Ukraine) 2 Poltava State Medical University; Poltava (Ukraine) E-mail: bezeganina@gmail.com TO CITE THIS ARTICLE: Bezditko PA, Bezega NM. Clinical features of symptomatic acquired lacrimal outflow obstruction in patients with type 2 diabetes mellitus. J.ophthalmol.(Ukraine).2022;2:32-6. http://doi.org/10.31288/oftalmolzh202223236 Background: Acquired lacrimal outflow obstruction (ALOO) may be either symptomatic (i.e., manifested by specific symptoms) or asymptomatic. Purpose: To identify the clinical features of symptomatic acquired lacrimal outflow obstruction in patients with type 2 diabetes mellitus (DM2). Material and Methods: Medical records of 284 patients with symptomatic ALOO were retrospectively examined. Of these patients, 56 (19.7%) were found to have DM2, and constituted the study group, and 228 (80.3%) had no diabetes, and constituted the control group. Specific eye examination methods included measurements of punctum size and tear meniscus height, tear production tests (Schirmer, Jones and tear film breakup tests), nasolacrimal test, tear absorbing test, reflux tests, assessment of lacrimal system balance, lacrimal irrigation, and lacrimal canaliculi probing. Results: DM2 was found in 19.7 ± 2.4% of patients with symptomatic ALOO. We identified the clinical features of symptomatic ALOO in patients with type 2 DM. The incidence of bilateral dacryocystitis (46.4 ± 6.7%) was 1.6-fold higher; dacryocystitis (60.7 ± 6.5%) was 1.5-fold higher; punctual occlusion (30.3 ± 6.1%), 1.3-fold higher; bilateral punctual occlusion (7.1 ± 3.4%), 2.7-fold higher; membranous stenosis (9.8 ± 3.3%), twice higher; pinpoint stenosis (9.8 ± 3.3%), 1.9-fold higher; and blepharitis (71.4 ± 6.0%), 1.4-fold higher in the above patients than in patients with symptomatic ALOO in the absence of type 2 DM (р < 0.05). In addition, patients with symptomatic ALOO combined with type 2 DM were at average 8.1 years younger than non-diabetic patients with ALOO (р < 0.05). Conclusion: DM2 was found in 19.7 ± 2.4% of patients with symptomatic ALOO. Clinical features of symptomatic ALOO were noted in patients with DM2. Keywords: acquired lacrimal outflow obstruction, type 2 diabetes mellitus, dacryocystitis
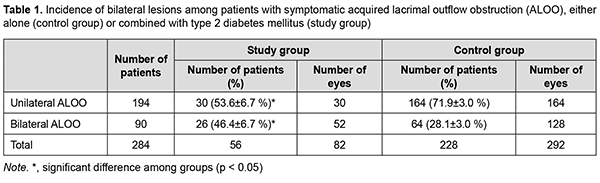
Introduction Disorders of the lacrimal outflow system account for 2% to 25% of all eye diseases and are of medical and social importance [1, 2]. Valieieva [1] reported that 9.2% of the outpatients and 2% of the inpatients with eye disease had disorders of the lacrimal outflow system. Disorders of the lacrimal outflow system cause obstruction of the lacrimal outflow tract and are manifested by tearing [3]. Acquired lacrimal outflow obstruction (ALOO) may be either symptomatic (i.e., manifested by specific symptoms, which makes the patient to seek for medical attention) or asymptomatic (i.e., lacrimal outflow obstruction with no symptoms) [3]. In recent decades, the prevalence of diabetes mellitus (DM) has been dramatically increasing, indicating an impending pandemic of diabetic disease. The reported prevalence of DM among patients with lacrimal outflow obstruction hospitalized for surgery ranges from 11.1 to 24.3% [4, 5]. Woog, an American ophthalmologist [3], found DM in 10.9% of patients with symptomatic ALOO, but did not identify the clinical features of the latter disease in patients with DM. The purpose of this study was to identify the clinical features of symptomatic acquired lacrimal outflow obstruction in patients with type 2 DM. Material and Methods Medical records of 284 patients with symptomatic ALOO were retrospectively examined. Of these patients, 56 (19.7%) were found to have type 2 DM, and constituted the study group, and 228 (80.3%) had no DM, and constituted the control group. Patient age was 63.7 ± 12.0 years and 71.8 ± 11.2 years for the former and latter groups, respectively. The study group consisted of 37 women and 19 men, and the control group, of 141 women and 87 men. Diagnostic criteria of symptomatic ALOO included at least one of the following: tearing complaints, a visibly elevated tear meniscus or visible epiphora, reflux upon lacrimal sac compression, punctual stenosis, acute or chronic dacryocystitis, and impaired flow through the tear ducts during lacrimal irrigation. Eye examination methods included chief complaints and history taking, visual acuity, general appearance assessment, biomicroscopy, tonometry, ophthalmoscopy, measurements of punctum size and tear meniscus height, tear production tests (Schirmer, Jones and tear film breakup tests), nasolacrimal test, tear absorbing test, reflux tests, assessment of lacrimal system balance, lacrimal irrigation, and lacrimal canaliculi probing. Punctal stenosis was classified into four types (membranous type, slit type, horseshoe type, and pinpoint type) based on slit-lamp biomicroscopy findings as per the classification of Hur and colleagues [6]. Punctal stenosis was diagnosed based on the symptoms of epiphora and a narrowing of the punctum to less than 0.2 mm in diameter, as determined by slit lamp ex¬amination [6]. If the internal canaliculus was severely narrowed such that the cannula tip could not reach the lacrimal sac and saline irrigation was ineffective, then the patients were diagnosed with a canalicular obstruction and a naso¬lacrimal duct obstruction. Return from the same punctum with some passage of fluid to the nose could imply canalicular stenosis. Common canalicular stenosis typically results in the return of clear fluid from the opposite punctum, with some nasal passage. Complete nasolacrimal duct (NLD) obstruction results in the regurgitation of saline and some mucous through the other punctum. Patients with stenotic NLD show passage of fluid to the nose and minimum reflux from the other canaliculus [7]. The study followed the ethical and bioethical standards stated in the Declaration of Helsinki. Data are presented as mean (M) and standard deviation (SD). Chi squared test was applied for group comparisons. The level of significance p ≤ 0.05 was assumed. Results Our retrospective review of the results of examination of 52 patients with type 2 DM (the study group) and 228 patients without type 2 DM (the control group) demonstrated that either unilateral or bilateral symptomatic ALOO was found in patients of both groups. Table 1 shows the distribution of patients in groups. The percentage incidence of unilateral lesions was for the control group was higher than for the study group (71.9 ± 3.0 versus 53.6 ± 6.7%, р< 0.05; Table 1). The percentage of bilateral lesions was higher for the study group than for the control group (46.4 ± 6.7 versus 28.1 ± 3.0%, р< 0.05). Therefore, incidence of bilateral lesions was 1.6-fold higher in patients with both symptomatic ALOO and type 2 DM than in non-diabetic controls (р< 0.05). These data allows us to hypothesize that DM is a factor resulting in ALOO.
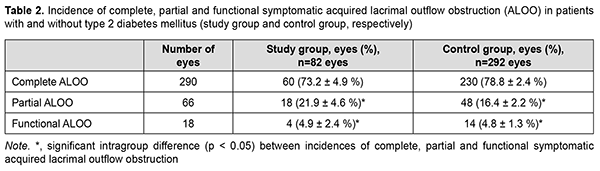
Table 2 shows the distribution of patients in groups with regard to the type of ALOO (complete, partial, or functional). There was no significant difference in the incidence of complete, partial, or functional ALOO between the study group and the control group. The incidence of complete ALOO was higher than that of partial and functional ALOO in either group (р< 0.05).
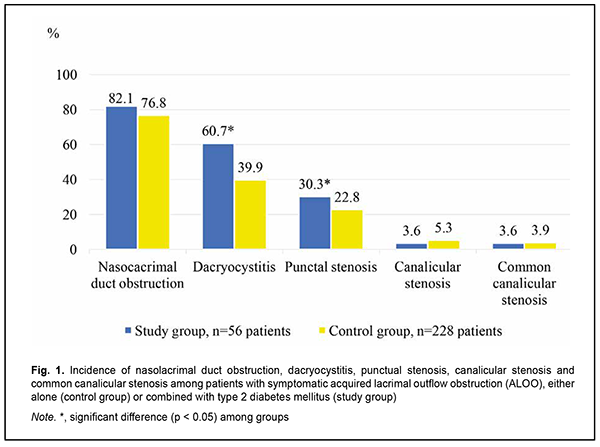
Fig. 1 presents the analysis of the location of lesions among patients with symptomatic ALOO depending on the presence of DM. Nasolacrimal duct obstruction was the most common and found in 82.1 ± 5.1% patients of the study group and 76.8 ± 2.8% patients of the control group (Fig. 1). It is noteworthy that the incidence of dacryocystitis in patients with DM was higher than in controls (60.7 ± 6.5% against 39.9 ± 3.2%, р< 0.05). Unilateral and bilateral dacryocystitis was found in 91.2 ± 4.9% and 8.8 ± 4.9%, respectively, of patients of the study group, and in 89 ± 3.3% and 11 ± 3.3%, respectively, of the controls.
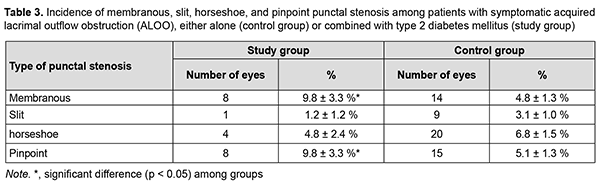
Punctal occlusion was the second most common type of occlusion for both groups, with the incidence of punctal occlusion being higher for the study group than for the control group (30.3 ± 6.1% versus 22.8 ± 2.8%; р< 0.05). Complete and partial punctal occlusion was found in 14.6 ± 3.9% and 11 ± 3.5%, respectively, of patients of the study group, and in 15.4 ± 2.1% and 4.4 ± 1.2%, respectively, of the controls. In addition, in the current study, punctal stenosis in patients of both groups was classified as per the classification of Hur and colleagues [6] (Table 3). Membranous and pinpoint types of punctal stenosis were more common than other types among patients of the study group, and there was no statistically significant difference between the incidences of different types of punctal stenosis among patients of the control group (Table 3). Canalicular obstruction was found in 3.6 ± 2.5% (bilateral canalicular obstruction in 1 patient (1.8 ± 1.8%) and unilateral canalicular obstruction in 1 patient (1.8 ± 1.8%)), and common canalicular obstruction, in 3.6 ± 2.5% (two patients with unilateral lesions) of patients of the study group. In addition, canalicular obstruction was found in 5.3 ± 1.5% (unilateral canalicular obstruction in 12 patients), and common canalicular obstruction, in 3.9 ± 1.3% (nine patients with unilateral lesions) of patients of the control group.
In 3 eyes of the study group, and in 7 eyes of the control group, canalicular stenosis was combined with partial nasolacrimal duct obstruction. The incidence of dacryocystitis was 1.5-fold higher; punctual occlusion, 1.3-fold higher; bilateral punctual occlusion, 2.7-fold higher; membranous stenosis, twice higher; and pinpoint stenosis, 1.9-fold higher in patients of the main group than in controls. The incidence of blepharitis was high in patients of both groups, and was 1.4-fold higher in patients of the main group than in controls (71.4 ± 6.0% versus 52.6 ± 3.3%, р< 0.05). Discussion The cause of acquired lacrimal drainage obstruction may be primary or secondary. Primary acquired nasolacrimal duct obstruction is more common and results from inflammation of unknown cause that eventually leads to occlusive fibrosis. Secondary acquired lacrimal drainage obstruction may result from a wide variety of infectious, inflammatory, neoplastic, traumatic, or mechanical causes, surgery or sarcoidosis [8]. In the current study, the incidence of type 2 DM in patients with symptomatic ALOO was 19.7 ± 2.4% which is higher than in a study by Woog and collegues (10.9 %) [4]. We identified the clinical features of symptomatic ALOO in patients with type 2 DM. The incidence of bilateral dacryocystitis (46.4 ± 6.7%) was 1.6-fold higher; dacryocystitis (60.7 ± 6.5%) was 1.5-fold higher; punctual occlusion (30.3 ± 6.1%), 1.3-fold higher; bilateral punctual occlusion (7.1 ± 3.4%), 2.7-fold higher; membranous stenosis (9.8 ± 3.3%), twice higher; pinpoint stenosis (9.8 ± 3.3%), 1.9-fold higher; and blepharitis (71.4 ± 6.0%), 1.4-fold higher in the above patients than in patients with symptomatic ALOO in the absence of type 2 DM (р< 0.05). In addition, patients with symptomatic ALOO combined with type 2 DM were at average 8.1 years younger than non-diabetic patients with ALOO (р< 0.05). High incidence of some types of symptomatic ALOO in patients with type 2 DM may be associated with a pathological inflammatory response [9] and epithelial metaplasia [10], which is characteristic for diabetes. Conclusion The incidence of type 2 DM in patients with symptomatic ALOO was 19.7 ± 2.4%. The clinical features of symptomatic ALOO in patients with type 2 DM were as follows: the incidence of bilateral dacryocystitis was 1.6-fold higher; dacryocystitis, 1.5-fold higher; bilateral punctual occlusion, 2.7-fold higher; membranous stenosis, twice higher; pinpoint stenosis, 1.9-fold higher; and blepharitis, 1.4-fold higher in the above patients than in patients with symptomatic ALOO in the absence of type 2 DM (р< 0.05). In addition, patients with symptomatic ALOO combined with type 2 DM were at average 8.1 years younger than non-diabetic patients with ALOO (р< 0.05).
Conflict of Interest. The authors do not have any actual or potential conflicts of interest (financial, personal, professional and other interests) that could affect their opinion regarding the subject or materials described and discussed in this article.
References 1.Valiyeva GN. [Remote results of transcanalicular laser-assisted dacryocystorhinostomy and measures to prevent recurrent nasolacrimal duct obstruction]. [Thesis for the Degree of Cand Sc (Med)]. Ufa: Ufa Eye Research Institute; 2006. Russian. 2.Linberg JV, McCormick SA. Primary acquired nasolacrimal duct obstruction. A clinicopathologic report and biopsy technique. Ophthalmology. 1986 Aug;93(8):1055-63. 3.Woog JJ. The incidence of symptomatic acquired lacrimal outflow obstruction among residents of Olmsted County, Minnesota, 1976-2000 (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2007;105:649-66. 4.Rabina G, Golan S, Neudorfer M, Leibovitch I. External Dacryocystorhinostomy: Characteristics and Surgical Outcomes in Patients with and without Previous Dacryocystitis. J Ophthalmol. 2013;2013:287524. 5.Sung JY, Lee YH, Kim KN, Kang TS, Lee SB. Surgical outcomes of endoscopic dacryocystorhinostomy: analysis of age effect. Sci Rep. 2019 Dec 27;9(1):19861. 6.Hur MC, Jin SW, Roh MS, Jeong WJ, Ryu WY, Kwon YH, Ahn HB. Classification of Lacrimal Punctal Stenosis and Its Related Histopathological Feature in Patients with Epiphora. Korean J Ophthalmol. 2017 Oct;31(5):375-382. 7.Kashkouli MB, Pakdel F, Kiavash V. Assessment and management of proximal and incomplete symptomatic obstruction of the lacrimal drainage system. Middle East Afr J Ophthalmol. 2012 Jan;19(1):60-9. 8.Bartley GB. Acquired lacrimal drainage obstruction: an etiologic classification system, case reports, and a review of the literature. Part 1. Ophthalmic Plast Reconstr Surg. 1992;8(4):237-242. 9.Tsai S, Clemente-Casares X, Revelo XS, Winer S, Winer DA. Are obesity-related insulin resistance and type 2 diabetes autoimmune diseases? Diabetes. 2015 Jun;64(6):1886-97. 10.Kesarwani D, Rizvi SWA, Khan AA, Amitava AK, Vasenwala SM, Siddiqui Z. Tear film and ocular surface dysfunction in diabetes mellitus in an Indian population. Indian J Ophthalmol. 2017 Apr;65(4):301-304.
|