J.ophthalmol.(Ukraine).2022;2:10-14.
|
http://doi.org/10.31288/oftalmolzh202221014 Received: 17 November 2021; Published on-line: 30 April 2022 Management of Accommodative Insufficiency among school-age children attending tertiary care Eye Institute Dr. T. Suparna D. O. 1, FIPOS, Dr. Swaroopa Gudimetla M. S. 2, FIPOS Sankar Foundation Eye Institute; Naiduthota, Visakhapatnam, Andhra Pradesh (India) TO CITE THIS ARTICLE:Suparna T, Swaroopa Gudimetla. Management of Accommodative Insufficiency among school-age children attending tertiary care Eye Institute. J.ophthalmol.(Ukraine).2022;2:10-4. http://doi.org/10.31288/oftalmolzh202221014 Introduction. Accommodative insufficiency (AI) is a non-strabismic binocular vision anomaly characterized by an inability to focus for near vision, with symptoms of blurred near vision, headache, visual fatigue, and asthenopic symptoms. Purpose. To evaluate the efficacy of Plus Lens treatment, and Flipper glasses in the improvement of Accommodative Amplitude (AA) and Near Point of Accommodation (NPA) in Accommodative insufficiency (AI). Methods. A prospective study of 50 children aged 8-15years with distance heterophoria (< 2 pd), near heterophoria(< 6 pd), Near Point of Convergence (NPC) (10 cm/better on Royal Air Force (RAF) rule), and NPA (worse than 10 cm, 15d – 2.5* age) were recruited during July 2018 to June 2019 and followed up for 3months. Measurements including NPC, NPA, and AA were measured in each eye of the Plus Lens Reading Addition(PLRA) and Flipper group. Results. Accommodative Insufficiency is higher in female children 67% in PLRA and 60% in the Flipper group with a mean age of 12.73 years in the PLRA group and 12.93 years in the Flipper group. NPA improved from 15.07 cm to 14.4 cm at 4 weeks, 11.87 cm at 8 weeks, and 9.33 cm at 12 weeks of treatment with PLRA. The NPA improved from 15.73 cm to 12.4 cm at 4 weeks, 10.93 cm at 8 weeks, and 8.27 cm at 12 weeks of treatment with Flipper glasses. AA improved from 6.73 D to 7.03 D at 4 weeks, 8.5 D at 8 weeks, and 10.73 D at 12 weeks of treatment with PLRA. The AA improved from 6.33 D to 8.03 D at 4 weeks, 9.13 D at 8 weeks, and 11.73 D at 12 weeks of treatment with Flipper glasses. Children reported good compliance and no longer experienced blur or headache. Conclusion. A higher level of improvement in NPA and AA is observed in the Flipper group. Faster improvement is seen in the Flipper group, and treatment time needed will be shorter in the Flipper group, but it is more difficult to motivate subjects to do orthoptic exercises as compared to wearing reading glasses. Кey words: accommodative dysfunction, flipper test, plus lens reading addition, vision therapy
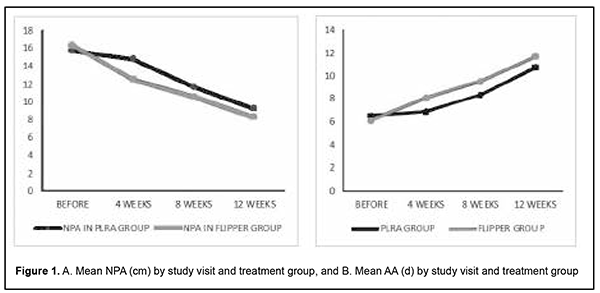
Introduction Accommodative Insufficiency (AI) is a condition in which a patient cannot focus, and/or sustain focus at near. The American Optometric Association(AOA) defines AI as occurring when the amplitude of accommodation is lower than expected for the patient’s age and is not due to sclerosis of the crystalline lens [1]. Accommodative disorders are commonly observed in pediatric eye care practices [2]. Associated signs and symptoms are related to reading and other close work activities and include blurred vision at near, headaches, watering or burning of eyes, tired eyes, loss of concentration, and avoidance of near activities [3-6]. The most commonly prescribed treatments for accommodative insufficiency are plus lens addition at near/vision therapy or orthoptics [2, 8-11]. Although plus lenses worn for near activities may improve symptoms for some patients, orthoptics has the potential to eliminate the accommodative dysfunction rather than solely providing symptomatic relief. Clinical studies reported success rates for the treatment of accommodative insufficiency as high as 96% [9-13]. This study aims to evaluate the efficacy of Plus Lens treatment, and Flipper glasses modalities in the management of Accommodative Insufficiency in children. Material and methods A prospective study was conducted at tertiary care Eye Institute from July 2018 to June 2019 with follow-up cases for 3 months. A total of 50 pediatric patients of age group 8-15 years were enrolled based on the fulfillment of inclusion and exclusion criteria. Inclusion criteria: • Patients of ≤15 years of age group. • Patients with Best corrected visual acuity (BCVA) – 20/20; distance heterophoria <2 pd, near heterophoria < 6pd; near point of convergence - 10 cm/better on RAF rule; NPA – worse than 10 cm/15d – 2.5*age; NFV of atleast 7 pd base in break and 5 pd base in recovery; PFV of 10 pd base out break and 7 pd base out recovery; and normal ocular motility. • Patients with no ocular pathology, no history of ophthalmic treatment, not taking any drugs with known effect on vision, binocular function, and accommodation. Exclusion criteria: • Patients with amblyopia (2/more lines difference in BCVA between 2 eyes), constant strabismus, history of strabismus surgery, and any refractive error (after cycloplegic refraction). • Patients with a history of refractive surgery, presence of manifest/latent nystagmus, accommodative insufficiency secondary to acquired/ traumatic brain injury. • Patients with a history of diabetes mellitus, multiple sclerosis, myasthenia gravis, developmental and intellectual disability. • Patients, who fulfill the inclusion/exclusion were included in the study by the first examiner. Patients were allotted into two groups of management (PLRA and Flippers) according to block randomization (block size 2). All the initial and follow-up measurements of study variables were performed by the second examiner without knowledge of the mode of management patients had received. Distance visual acuities were measured in each eye using Snellen letters and the projector chart. Near visual acuities were measured in each eye with reduced Snellen equivalent letters at 40 cm. A 20/30 to 20/40 Snellen letter was used at distance and a 20/30 reduced Snellen equivalent letter was used at 40cm as a fixation target. Ocular alignment was assessed at a distance and near using cover test and alternate cover testing with prism neutralization. Measurements were assessed at both 6meters and 40 cm. The cover test is used to identify the presence or absence of strabismus. The subjects were instructed to maintain clarity and fixation of the target throughout testing. The magnitude was recorded as the amount of prism just below the amount where 5 reversals were observed. Stereopsis was measured using the Titmus Fly Chart for near and Random chart for distance. NPC, NPA, and AA are measured by specially designed rules such as the RAF rule. It consists of a bar or rule made from metal on which a rider with the test chart can be moved back and forth (fixation target). At one end of the bar is wing-like support that fits over the nose and rests against the lower orbital margins during the measurement. One side is divided into centimeters – used for measurement of NPC, NPA, the second one into inches, the third one into diopters – for AA, and age is indicated in years on the fourth side. NPA, near point of accommodation, is the closest point at which small objects can be seen clearly. To determine NPA, a sliding target with N8 letters is moved towards the eye until the closest point is found at which it still can be seen clearly. NPA is first determined for each eye separately and then for both eyes together. NPA is measured in centimeters.. For the measurement of convergence, a dot is used as a target. It is advanced towards the patient at, or slightly below the eye level until the patient has converged maximally and cannot sustain a single bifoveal fixation as the target is brought closer. At this breakpoint, the subject‘s non-dominant eye will diverge (objective test) and the patient may appreciate diplopia (subjective test). The distance from the canthus to this point is read on the rule and NPC is recorded in mm or cm. The amplitude of accommodation was measured by the push-up method. The patient is instructed to view the target at a distance of 40cm and then the target was slowly moved towards the subject along with the RAF rule. Patients were instructed to report when the target first became blurred. At that point, the side of the bar marked in diopters will indicate the amplitude of accommodation in diopters. Fusional vergences were measured by handheld prism bars (base in and base out). The accommodative facility is the speed at which the patient could see 20/30 letters at 40cm clearly through alternating +2.00 D, and -2.00 D lenses, measured in cycles per minute (cpm). The decreased accommodative facility was defined as <6cpm, which is 1 SD below the normative value of 11cpm for school-age children. The treatment received was either +1 D plus lens reading addition (PLRA) or +/- 1.00 D Flipper glasses. For the PLRA treatment, the children were encouraged to use glasses for all types of near visual work as much as possible For the flipper glasses treatment group, the children were instructed to do 2 sessions of fifteen minutes each day. The sessions were to be done at times when the subjects were not feeling tired or experiencing asthenopia. The subjects do as many flips as they can keeping the target at 40cm as clear as possible. The children of both groups were advised to follow up at 4 weeks, 8 weeks, and 12 weeks and visual acuity, NPA, and AA were measured at each visit of follow-up. Statistical analysis was done using SPSS software version 17(SPSS Inc, Chicago, IL). Descriptive statistics were calculated for all the parameters recorded in the study. Hypotheses were formulated and tested for significance using ANOVA. Values are represented in percentage and mean±SD. Column stats and student t-test were used to determine the mean and SD and p-value in respective groups. One-way ANOVA was used to calculate the statistical significance in more than three groups. A p-value of 0.05 or less has been considered statistically significant. Results Demographics In the PLRA group, 13 (52%) belong to 8-12 years of age, 12 (48%) belong to 13- 15 years with a mean age of 12.24 ± 2.08 years. In the FLIPPER group, 9 (36%) belong to 8-12 years of age, 16 (64%) belong to 13-15 years with a mean age of 12.8 ± 1.75 years. In the PLRA group, 9 (36%) were male children and 16 (64%) were female children, whereas, 10 (40%) were male children and 15 (60%) were female children recorded in the FLIPPER group. Improvement of near point of accommodation Near the point of accommodation (NPA)in cm in Plus Lens Reading Addition(PLRA) group before treatment was 15.76 ± 2.66, after 4 weeks of treatment NPA improved to 14.8 ± 2.08, after 8 weeks of treatment NPA improved to 11.64 ± 2.89 and after 12 weeks of treatment NPA was 9.28 ± 1.62, which is almost normal. NPA in Flipper group before treatment was 16.32 ± 2.56, after 4 weeks of treatment NPA improved to 12.48 ± 1.93, after 8 weeks of treatment NPA improved to 10.56±1.47 and after 12 weeks NPA was 8.32 ± 0.74, which is normal (p<0.00001). Improvement of accommodative amplitude Accommodative amplitude (AA) (D) in the PLRA group before treatment was 6.48± 1.11, improved to 6.84±1.08 after 4 weeks of treatment, 8.32±1.27 after 8 weeks of treatment, and 10.76±1.5 after 12 weeks of treatment (p<0.00001). AA in the Flipper group before treatment was 6.12 ± 1.1, improved to 8.06 ± 1.23 after 4 weeks of treatment, 9.48 ± 1.38 after 8 weeks of treatment, and 11.68 ± 0.74 after 12 weeks of treatment (p<0.00001). NPA and AA in both groups before and after treatment NPA in the PLRA group improved from 15.76 cm to 9.28 cm showing an improvement of 6.48 cm which was statistically significant. NPA in the Flipper group improved from 16.32cm to 8.32cm showing an improvement of 8.0 cm which was statistically significant (p<0.00001). AA in the PLRA group improved from 6.48 D to 10.76 D with a difference of 4.28 D which was statistically significant. AA in the Flipper group improved from 6.12 D to 11.68 D with a difference of 5.56 D which was statistically significant (p<0.00001) (Table 1).
NPA has improved significantly in the flipper group after 4 weeks of treatment when compared to the PLRA group. There is no significant difference in outcomes of both treatment groups after 12 weeks of treatment but improvement is fast in the flipper group when compared to the PLRA group. There is a significant improvement in AA in the flipper group after 4 weeks of treatment when compared to the PLRA group. There is no significant difference in outcomes of both treatment groups after 12 weeks of treatment but improvement is fast in the flipper group when compared to the PLRA group (Figure 1).
Discussion This is a hospital-based prospective study conducted on 50 children. Accommodative insufficiency can be improved with vision therapy by purposeful and controlled manipulations of target blur. The commonly used regimes of therapy for AI are fundamentally different, in that PLRA is a more passive type of treatment when compared to flipper treatment. However, in both regimes, the aim was to improve the response of blur-driven sensors, and adaptive mechanisms within the accommodative system, so that they can regain normal capacity. The purpose of this study is to evaluate which mode of therapy either PLRA or spherical flipper, is more effective in the treatment of accommodative insufficiency. Our study included 50 children of age group 8-15 years presenting to the pediatric ophthalmology department with accommodative insufficiency. In our study, 13 (52%) children belong to the age group of 8-12 years, 12 (48%) belong to the age group of 13-15 years and the mean age was 12.24 years in the PLRA group. In the flipper group 9 (36%) children belong to age group 8- 12 years, 16 (64%) children belong to age group 13-15 years, and the mean age was 12.8 years. In our study, 9 (36%) children are male, 16 (64%) are female in the PLRA group, 10 (40%) children are male, 15 (60%) children are female in the flipper group. In our study, NPA improved from 15.76 cm to 9.28 cm with a difference of 6.48 cm after 12 weeks of treatment PLRA group. This result is at par with S. Abdi et al. (2005) [15] which showed improvement of NPA from 10-25 cm to 8-10 cm after treatment with PLRA. S. Abdi et al. [15] showed improvement of NPA at 8 weeks of treatment with PLRA (+1D). In the flipper group, NPA improved from 16.32 cm to 8.32 cm with a difference of 8.0 cm after 12 weeks of treatment. There is no study comparable for improvement of NPA in the flipper group. In our study, AA improved from 6.48D to 10.76D with a difference of 4.28D after 12 weeks of treatment in the PLRA group. This improvement is slightly higher than R. Brautaset et al. [14] where improvement is 1.58 D, due to difference in treatment duration (8 weeks). According to Daum et al.[11], 53% showed total improvement in symptoms within 1 week of treatment with PLRA. In our study AA improved from 6.12 D to 11.68 D with a difference of 5.56 D after 12 weeks of treatment with flipper glasses. This is in variance with Brautaset et al.[14], which showed an improvement of AA from 4.25 D to 7.82 D with a difference of 3.57 D. The higher improvement in our study can be attributed to the increased duration of exercises executed per day when compared to other studies. Sterner et al. [11] showed improvement in accommodative insufficiency with flipper glasses but variables are different. Our study showed faster improvement in both NPA and AA in the flipper group i.e., at 4 weeks of treatment when compared with the PLRA group, but there is no statistically significant difference in the outcome of treatment in both groups after 12 weeks. This finding is in correlation with the results of R. Brautaset et al. [14]. The higher level of improvement in the accommodative amplitude after treatment in the flipper group indicates that treatment time needed will be shorter with this type of treatment as compared with PLRA. On the other hand, it is more difficult to motivate subjects to do orthoptic exercises as compared to wearing reading glasses. Conclusion In Flipper group, NPA improved from 16.32 cm to 8.32 cm, while AA improved from 6.12D to 11.68 D with significant difference. In PLRA group, NPA improved from 15.76 cm to 9.28 cm, while AA improved from 6.48 D to 10.76 D with significant difference. NPA and AA improved in both PLRA and Flipper groups. But a higher level of improvement in NPA and AA is seen in the Flipper group than the PLRA group but the difference is not statistically significant. Faster improvement is seen in the Flipper group than PLRA group, so treatment time needed will be shorter in the Flipper group, but it is more difficult to motivate subjects to do orthoptic exercises as compared to wearing reading glasses. Accommodative insufficiency can be successfully managed by optometric vision therapy in adjunction with an added plus lens. A detailed binocular and accommodative evaluation is a must before prescribing added lens.
Abbreviations AI: Accommodative insufficiency, AA:Accommodative Amplitude, BCVA:Best corrected visual acuity(BCVA), NPA:Near Point of Accommodation, NPC:Near Point of Convergence, PLRA:Plus Lens Reading Addition, RAF:Royal Air Force, D: diopters, pd: prism dioptres, Cm:centimeters . Declaration of patient consent. The authors certify that they have obtained all appropriate patient consent forms from parents/guardians of the children. Ethics approval was obtained from the institutional ethics committee. Financial support and sponsorship. Nil. Conflicts of interest. There are no conflicts of interest. References 1.Cooper J. Accommodative dysfunction. In Amos JF (Eds.), Diagnosis and management in vision care. Boston: Butterworths (1987): 431-459. 2.Scheiman M, Wick B. Clinical Management of Binocular Vision: Heterophoric, Accommodative and Eye Movement Disorders, 3rd ed. Philadelphia, PA: Lippincott, Williams and Wilkins; 2008. 3.Daum KM. Accommodative dysfunction. Doc Ophthalmol 1983; 55: 177-98. 4.Hennessey D, Iosue RA, Rouse MW. Relation of symptoms to accommodative infacility of school-aged children. Am J Optom Physiol Opt 1984; 61: 177-83. 5.Nunes AF, Monteiro PM, Ferreira FB, Nunes AS. Convergence insufficiency and accommodative insufficiency in children. BMC ophthalmology. 2019; 19 (1):1-8. 6.García-Muñoz Á, Carbonell-Bonete S, Cacho-Martínez P. Symptomatology associated with accommodative and binocular vision anomalies. Journal of Optometry. 2014; 7 (4): 178-92. 7.Wahlberg M, Abdi S, Brautaset R. Treatment of accommodative insufficiency with plus lens reading addition: is+ 1.00 D better than+ 2.00 D?. Strabismus. 2010 Jun 1;18(2):67-71. 8.Hussaindeen JR, Murali A. Accommodative Insufficiency: Prevalence, Impact and Treatment Options. Clinical Optometry. 2020;12:135. 9.Shukla Y. Accommodative anomalies in children. Indian Journal of Ophthalmology. 2020 Aug;68(8):1520. 10.Scheiman M, Cotter S, Kulp MT, Mitchell GL, Cooper J, Gallaway M, Hopkins KB, Bartuccio M, Chung I. Treatment of accommodative dysfunction in children: results from an random clinical trial. Optom Vis Sci 2011;88(11):1343. 11.Sterner B, Abrahamsson M, Sjostrom A. Accommodative facility training with a long term follow up in a sample of school aged children showing accommodative dysfunction. Doc Ophthalmol. 1999; 99: 93-101. 12.Daum KM. Accommodative insufficiency. Am J Optom Physiol Oрt. 1983; 60: 352-9. 13.Hoffman L, Cohen AH, Feuer G. Effectiveness of non – strabismus optometric vision training in a private practice. Am J Optom Arch Am Acad Optom.1973; 50: 813-6. 14.Rune Brautaset, Marika Wahlberg, Saber Abdi, Tony Pansell. Accommodation Insufficiency in children: Are Exercises better than Reading Glasses? Strabismus. 2008; 16: 65-69. 15.Abdi S, Rydberg A. Asthenopia in schoolchildren, orthoptic and ophthalmological findings and treatment. Doc Ophthalmol. 2005; 111(2): 65-72. 16.Scheiman M, Cotter S, Kulp MT, et al. Treatment of accommodative dysfunction in children: results from a randomized clinical trial. Optom Vis Sci. 2011; 88(11): 1343-1352.
Received 17.11.2021
|