J.ophthalmol.(Ukraine).2021;6:21-24.
|
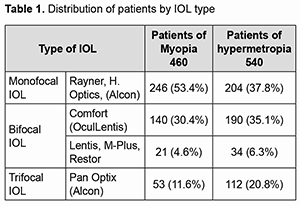
http://doi.org/10.31288/oftalmolzh202162124 Received: 26 May 2021; Published on-line: 21 December 2021 Development of new methods of selection of multifocal intraocular correction in cataract surgery Alnoelaty ALmasri M. A., postgraduate student: V. C. Stebnev, MD, Prof. Federal State Budgetary Educational institution of Higher Education Samara State Medical University of the Ministry of Health of the Russian Federation Samara (Russian Federation) E-mail: noelatyaeham@yahoo.com TO CITE THIS ARTICLE: Alnoelaty ALmasri MA, Stebnev VC. Development of new methods of selection of multifocal intraocular correction in cataract surgery. J.ophthalmol.(Ukraine).2021;6:21-24. http://doi.org/10.31288/oftalmolzh202162124 Рurpose. Upon obtained information from a questionnaire and trial multifocal contact lenses prior operation, our goal is to present a new methodology to select patients for multifocal intraocular correction with an individual definition of the IOL type. Patients and methods. An analysis of 1000 medical case reports (540 hyperopia, 460 myopia) and questionnaire of patients who have undergone operation because of cataract and refractive anomalies in the section of lens surgery and intraocular correction, department of eye diseases in Samara regional clinical hospital named after V. D. Seredavin. Patients are offered monofocal IOLs from leading global manufacturers, such as Rayner, H.Optics and Alcon, bifocal IOLs such as M-plus, Comfort (Oculentis), Restor (Alcon) and the trifocal IOL PanOptix (Alcon) for implantation. To get our goal, questionnaires were developed with questions allowing to determine the psychological type of the patient before the surgery, the nature of his/her visual stress besides requirements and expectations after surgery. Multifocal contact lenses Acuvue Moist with varying ADD power are selected to patients before operation to create similar conditions of multifocal intraocular correction. Visual acuity, contrast sensitivity are evaluated 2 weeks and 2 months postoperatively. At the same time, another survey is conducted to evaluate their satisfaction of visual outcomes. Results. According to analysis, the percentage of implantations of monofocal IOLs was (450 patients) 45%, while percentage of multifocal IOLs was (550 patients ) 55 % among all ultrasound phacoemulsification surgeries. Of these, in (330) 60 % of cases patients have chosen IOLs with a low degree of ADD power (Lentis Comfort), in (165 patients) 30 % — PanOptix and in (55 patients) 10 % — Lentis M-plus or Restor. Degree of satisfaction and visual results in 2 weeks and 2 months was recorded from (5 points) and obtained (506 patients) 92 % and (528 patients) 96 % respectively. Cases with incomplete patient dissatisfaction don’t exceed (18 patients) 3.2 % and is reported mainly in the group with the implantation of bifocal IOLs and are related with typical complaints of light phenomena, mostly at night. Кey words: multifocal, intraocular, contact lenses, questionnaire
Introduction Multifocal IOLs have been implanted since 1986, and over that time they have evolved and improved greatly. Nowadays, the implantation of multifocal intraocular lenses (M-IOLs) is firmly established in the daily surgical practice of most ophthalmic clinics after cataract surgery [1, 2]. The appearance of new models of multifocal IOLs [3-5] forces ophthalmologists and medical staff all around the world to build new discussions and reconsider priorities of patients, [6, 7] who have chosen this method of correction as a measure to get rid of glasses or reduce dramatically their dependence on them [8]. The aim of the work was to analyse performance of the ophthalmology clinic in the field of surgical treatment of both cataract and refractive anomalies in correlation with the degree of satisfaction of patients, whose implanted different types of multifocal IOLs. Depending on the data of the questionnaire and preoperative choice of trial multifocal contact lenses, type of M-IOLs was selected. To achieve this goal, the following tasks were set. 1. Determine the percentage of implanted M-IOL among all ultrasound phacoemulsification operations in our surgical department, which offer various types of intraocular correction. 2. Develop a questionnaire with questions that allows to determine the patient's psychotype, characteristics of his visual strain, and after all, his requirements and expectation of vision before the operation. 3. Create a model of multifocal intraocular correction for patients using experimental multifocal contact lenses with different degrees of addition. 4. Analyse the quantitative of patients who have chosen every type of multifocal correction. 5. Determine the degree of patient satisfaction with results of treatment performed in correlation with individual selection of multifocal intraocular lenses. Patients and methods The study is based on data, which was collected from analysis of 1000 clinical cases and questionnaires of patients operated recently in the section of surgery and intraocular correction, department of eye diseases in Samara regional clinical hospital named after V. D. Seredavin. All patients, whose average age was 60± 0.8 years, had anomalies in refraction preoperatively, 540 patients (55%) had hyperopia, while 460 patients had myopia. Visual acuity was assessed in all patients using chart of Snellen S Visual acuity Chart (Appasamy Associate, India) or illiterate E chart and was in the average of 0,3-0,5 in all patients of our study. Every patient was asked about his /her chief complaints, previous history of injury, ocular surgeries, and history of systemic diseases. To involve patients in our research, Criteria for inclusion was established; presence of senile opacity of the lens (cataract) of varying degrees in combination with a varying degree of refractive anomaly of hyperopia or myopia with regular corneal astigmatism not exceeding 0.5 D, absence of gross concomitant pathology of the visual organ, leading to persistent and irreversible vision loss, preservation of the ligamentous apparatus of the lens. In the other hand, patients with irregular astigmatism, corneal disease, abnormal iris, pupil abnormalities, glaucoma, any kind of retinal disease, strabismus, previous ocular trauma or surgery were excluded. All patients had the operation of ultrasound phacoemulsification according to standard methods using the Centurion phacomachine. Patients were presented Monofocal IOLs from Alcon, Rayner, and H. Optics, bifocal IOLs such as M-plus, Comfort (Oculentis), Restor (Alcon), and trifocal Pan-optix IOLs (Alcon) (Table 1). After making a clinical diagnosis and determining indications of surgery, every patient was offered a questionnaire, which was formed by our clinical staff. The patient was asked to check a box against one of possible answers. In cases of difficulties of understanding, questions were read and explained wordily to the patient. - Are you ready to have the operation of cataract surgery, which will restore and improve your vision, and will be performed in our department in the hospital, painless, lasting 10-15 minutes? 1. Not ready yet 2. Yes, I'm ready If the answer to the first question was negative, no further survey was conducted. - What does that mean to you, if you were told, after surgery, that you need glasses for work or for distance vision? 3. I don't want to use glasses at all 4. I don’t mind using glasses for working with small text or objects 5. Glasses do not bother me, I am ready to use them in necessary cases - Is your daily or professional activity related to small objects (jeweller, watchmaker, etc.), or to work with optical instruments (microscope, video camera, etc.), or to drive a car constantly in difficult conditions (night, fog, etc.)? 6. Not related 7. Related - Are you ready for the fact that you may need some time (days, weeks) to get used to the "new" vision after the operation? 8. It doesn't scare me 9. I would not like to face such phenomena - Are you prepared for the fact that when driving a car or truck at night, you may have problems associated with halos around light sources? 10. I don't drive a car 11. I am ready to limit night time movement if necessary 12. I think this is unacceptable - Are you ready for the fact that to get a high-quality vision, you will need a similar operation on the second eye, even with a good vision? 13. I am ready to get operated on both eyes sequentially, if necessary 14. I am not ready to operate the second well-sighted eye Clinical analysis showed that patients who gave positive answers to questions № 3, 8, 11, can be recommended for correction of tri-and bifocal IOLs; patients who noted, in the questionnaire, № 4, 9, 12, was better to correct aphakia with lenses of low degree of addition; those whose responses in questions № 5, 7, 14, was positive, were better recommended to have Monofocal IOLs for correction. Finally, the type of multifocal IOL was selected after a personal conversation with the patient and, when possible, after trying selected multifocal contact lenses with varying degrees of addition. We used the latest developments in the field of multifocal contact correction: Acuvue Moist refractive multifocal contact lenses with the addition of Low (0.75; 1.0; 1.25 dptr), Mid (1.5; 1.75 dptr), High (2.25; 2.50 dptr). Multifocal contact lenses were selected strictly according to methods developed by the manufacturer [9, 10]. Visual acuity and contrast sensitivity are evaluated 2 weeks, 2 months after surgery. To study subjective sentiments of patients and their satisfaction of results of double-sided implantation of multifocal IOLs, we developed a second questionnaire which was offered 2 weeks and 2 months after surgical intervention. The following questions were added to the questionnaire: - Are you satisfied with your eyesight after performing the operation? 1 - Fully satisfied 2 - Satisfied, but not fully satisfied 3 - Not satisfied - Has your life changed after your surgery? 1 - Not changed 2 - Changed for the better 3 - Changed for the worse - Do you use your glasses after the operation? 1 - I don't use it at all 2 - I use it occasionally 3 - I use it constantly - Do you worry about increased os[1]fatigue, light halos, glare after surgery? 1 - Do not disturb 2 - Disturbed occasionally, mostly at night - Do you have difficulty driving a car or a truck? 1 - I don't test it 2 - I experience mostly at night 3 - I experience it constantly - Would you advise your friends or relatives to perform such an operation if necessary? 1 - Yes 2 - No Results According to results of assessments of visual acuity in postoperative period, visual acuity without correction in the group of patients with monofocal IOLs was of 0.82±0.03. Visual acuity in the distance without correction in the group of patients with bifocal IOLs 0.8±0.03 and trifocal IOLs 0.79±0.02. No statistically significant differences in distant visual acuity between all groups (p>0.05). At a distance of 25 cm (near vision), in the group of patients with bifocal IOLs, average value of visual acuity without correction was recorded after surgery of 0.73±0.02. While it was in the groups of patients with trifocal IOLs 0.69 ± 0.02, and for the monofocal group is 0.13 ± 0.01. However, there were no statistically significant differences in the average values of visual acuity at a distance of 25 cm between the group of patients of bifocal and trifocal IOLs (p>0.05). The difference in uncorrected visual acuity between the groups of patients with monofocal IOLs is statistically significant (p<0.05). The average value of visual acuity at a distance of 50 cm (intermediate distance) without correction in the group of patients with trifocal IOLs after surgery was 0.5±0.01. The average value of visual acuity at a distance of 50 cm without correction in the groups of patients of bifocal and monofocal IOLs after surgery was 0.18±0.01 and 0.2±0.001, respectively. At a distance of 50 cm, visual acuity without correction was statistically significantly higher in the group of patients of trifocal IOLs compared to other groups (p<0.05). Clinical studies attested expected decrease in contrast sensitivity at all spatial frequencies in the group of patients with trifocal IOLs. The decrease in spatial contrast sensitivity was not statistically significant in comparison with the group of monofocal IOL patients (p>0.05). Also, the study did not reveal a statistically significant difference between all groups in terms of stereo vision (p>0.05). The analysis of medical points, pre and post-operative questionnaires allowed us to draw the following conclusion: 1. The percentage of multifocal IOL implantation among all ultrasound phacoemulsification operations was (550 patients) 55 %, while the percentage of monofocal IOL was (450 patients) 45%. 2. Among the types of multifocal intraocular lenses selected by the patients, (330 patients) 60 % were IOLs with a low degree of addition (Lentis Comfort), ( 165 patients) 30 % IOLs with trifocal optics (PanOptix) and (55 patients) 10 % — IOLs with bifocal optics (Lentis M-plus, Restor). 3. The degree of patient satisfaction with the operation and related visual outcome two weeks postoperatively was (506 patients) 92 %, and after 2 months (528 patients) 96 %, which, in our opinion, is due to the high quality of modern multifocal lenses and appropriate selection of patients for the operation, based on an individual questionnaire and use of trial contact multifocal lenses. 4. Cases with incomplete patient satisfaction with the operation performed ( 18 patients) 4.6 % were noted mainly in the group with implantation of bifocal intraocular lenses and are associated with typical complaints such appearance of light phenomena, mainly at night. References 1.Pepose JS. Maximizing satisfaction with presbyopia correcting intraocular lenses: The missing links. Am J Ophthalmol 2008;146:641 8. 2.Gibbons A., Ali T.K., Waren D.P., Donaldson K.E. Causes and correction of dissatisfaction a implantation of presbyopia-correcting intraocular lenses. Clin Oph- thalmol. 2016 Oct 11;10:1965–1970. eCollection 2016. 3.Peng C, Zhao J, Ma L, Qu B, Sun Q, Zhang J. Optical performance after bilateral implantation of apodized aspheric diffractive multifocal intraocular lenses with +3.00-D addition power. Acta Ophthalmol. 2012;90(8):e586-93. 4.Pearce JL. Multifocal intraocular lenses. Curr Opin Ophthalmol 1996;7:2 10. 5.Stebnev V.S., Stebnev S.D., Malov I.V., Skladchikova N.I. Our rst experience implantation of trifocal intraocular lenses Acrysof IQ PanOptix. Modern technologies in ophthalmology 2017:6:106–107 (In Russ). 6.Breyer D.R.H., Kaymak H., Ax T., Kretz F.T.A., Au arth G.U., Hagen P.R. Multifocal Intraocular Lenses and Extended Depth of Focus Intraocular Lenses. Asia Pac J Ophthalmol (Phila).2017 Jul-Aug;6(4):339–349. 7.Kohnen T, Titke C, Böhm M. Trifocal Intraocular Lens Implantation to Treat Visual Demands in Various Distances Following Lens Removal. Am J Ophthalmol. 2016 Jan;161:71–77.e1. 8.Alio J.L., Pikkel J. Multifocal Intraocular Lenses: Neuroadaptation. Multifocal Intraocular Lenses. Springer International Publishing, 2014. P. 47–52. 9.Davis R.A. Fitting Tips for Presbyopic Success. Review of Cornea and Contact Lens. 19. 2010. Oct. 10.Hudson C. How to succeed with multifocal contact lenses. Optometry Today. 2011;51(11):3.
Conflict of interest: No conflict of interest. Financial Disclosure: No author has a financial or proprietary interest in any material or method mentioned.
Received 26.05.21
|