J.ophthalmol.(Ukraine).2021;6:8-15.
|
http://doi.org/10.31288/oftalmolzh20216815 Received: 07 July 2021; Published on-line: 21 December 2021
Visual outcome following cataract surgery in children of 2 months to 16 years age: a prospective study in a tertiary eye care center N. Deepthi Slesser, Nasrin Y., P. Krishna Prasad Sankar Foundation Eye Institute, Visakhapatnam, Andhra Pradesh (India) E-mail: drnasrin95@gmail.com TO CITE THIS ARTICLE: Deepthi Slesser N, Nasrin Y, Krishna Prasad P. Visual outcome following cataract surgery in children of 2 months to 16 years age: a prospective study in a tertiary eye care center. J.ophthalmol.(Ukraine). 2021;6:8-15. http://doi.org/10.31288/oftalmolzh20216815
Background. Childhood cataract is an important cause of blindness in children and imposes a huge socio economic burden on society. Purpose. Aim of the study is to identify the visual outcome after cataract surgery in paediatric age group and to study the various factors which influence visual outcome and surgical complications in paediatric cataract surgery. Material and Methods. This prospective study conducted at a tertiary Eye care Hospital for the period of September 2016 to February 2017. 30 children who presented with developmental cataract or congenital cataract in the age group of 2months – 16 years included in this study. Visual acuity in children less than 5 years was assessed using picture chart, E charts and Cardiff acuity cards and by snellen’s chart for >5 years age children. Biomicroscopy, Fundus examination, and A scan were done. Children were reviewed every day for first day and then every week for first month and every 3 months for the first year after cataract surgery. Results. There were males (56.67%) dominance. Visual Inattentiveness/ defective vision was observed in 29(64.4%) of eyes. 13(33%) children had consanguity. Most of them were bilateral 26 (87%). Nystagmus was found to be the most common6 (20%) associated ocular anomaly. Vision at the time of presentation was less than 6/60 in better eye in 30 eyes (66.66%). Commonest type of cataract was total cataract 20(44.44%), followed by lamellar cataract 10 (22.22%). 45 eyes were operated, and IOL was implanted 73.33% of the eyes. Posterior capsulotomy with or without anterior vitrectomy was done in children less than 8 years of age. Following retinoscopic refraction, children were prescribed bifocal spectacles. Aphakic spectacles were prescribed in needed cases. Visual outcome at the end of 6 weeks was found to be greater than 6/24 in 66.66%. At the end of 12 months, vision greater than 6/24 was 48.88%. Posterior Capsule Opacification (PCO) was thick enough to require capsulotomy in 4 eyes. 3 Children underwent YAG capsulotomy. 1 eye needed surgical membranectomy. Complications other than PCO that was noted in this study were amblyopia which was seen in 5 eyes and optic capture in 2 eyes, anterior synaechiae in 1 eye and vitreous haemorrhage in 1 eye. Conclusion. Children less than 8 years who underwent primary posterior capsulotomy with or without anterior vitrectomy showed good visual outcome. PCO is the commonest complication and a major cause for visual obscuration following surgery, though the incidence of PCO has been brought down with modified surgical techniques and newer IOL designs. Children who underwent YAG/surgical capsulotomy had significant visual gain. Children with amblyopia who had strict adherence to occlusion therapy had significant improvement in visual acuity. Кey words: сhildhood cataract, visual acuity, YAG capsulotomy, amblyopia
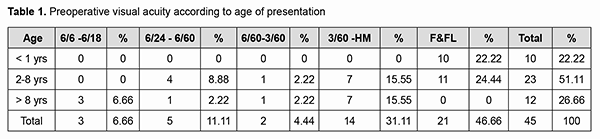
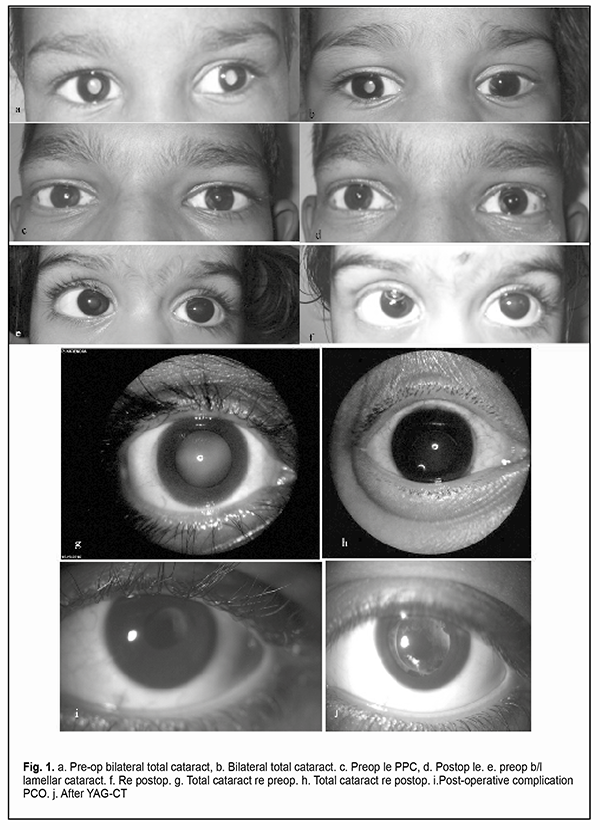
Introduction Visual impairment at an early age has far-reaching implications on a child’s life. It can hinder education, hamper personality development, and deprive the individual of career opportunities, thus increasing the socioeconomic burden on the family and the community [1]. Childhood blindness is one of the priority eye diseases within the disease control strategy of the “VISION 2020” initiative [2]. In developing countries like India 7.4 – 15.3% of childhood blindness is due to cataract [3-5]. Currently cataract remains one of the most important causes of treatable blindness in children [6]. The aim of paediatric cataract surgery is to provide and maintain a clear visual axis and a focused retinal image [7]. The visual outcome of cataract surgery in children have generally been poorer than in adults as blindness in children with cataract is not only attributed to cataract, but also to visual deprivation from early onset and delayed presentation, and thus delayed surgery, complications of surgery, and associated ocular abnormalities [8]. The risk of post-op complications is higher due to greater inflammatory response after paediatric intraocular surgery. To assure the best long-term outcome for cataract blind children, appropriate paediatric surgical techniques need to be applied and children have to be monitored and managed by a team comprising paediatric ophthalmologists, orthoptists, optometrists, skilled teachers, social workers and more importantly aware and patient parents. The purpose of this study is to assess the visual outcome after cataract surgery in children. Aim of the study is to identify the visual outcome after cataract surgery in paediatric age group; to study the various factors that influence visual outcome and surgical complications in paediatric cataract surgery. Materials and methods A hospital-based prospective study was done at a tertiary eye care centre. The target population enrolled in the present study were children with cataract, undergoing cataract surgery at tertiary eye care centers who were selected. 30 children who presented with developmental cataract or congenital cataract in the age group of 2 months - 16 years to Sankar Foundation Eye Hospital, Visakhapatnam during the period September 2016 to February 2017 were included in this study. Informed consent was obtained by the parents. Inclusion criteria were children who were diagnosed to have congenital or developmental cataract aged from 2 months to 16 years (further categorized as <2 years, 2-8 years and >8-16 years of age). Exclusion criteria were patients with traumatic cataract, complicated cataract, and other associated retinal anomalies. The sample size is taken as 30 (Cochrane formula t2*p(1-p)/d2; t – confidence interval which is taken as 1.96 when confidence level is 95%, p – prevalence, d – margin of error taken as 0.05). Study duration of 18 months period from September 2016 to February 2018. Each patient is followed on the 1st day,1st week,2nd week,4th week,6th week, 3 months, 6 months and 1 year postoperatively. Method. In children < 2 years, who are uncooperative for standard visual testing, fixation behaviour, fixation preference and objection to occlusion was checked. Visual acuity in children less than 5 years was assessed using picture chart, E charts and Cardiff acuity cards. In children >5 years Snellen’s chart was used. Anterior segment evaluation of the cornea, iris, anterior chamber and lens was carried out using slit-lamp biomicroscopy. Fundus examination was done using direct or indirect ophthalmoscopy. In children less than 5 years, examination was done under sedation or general anaesthesia. Examination under Anaesthesia (EUA) included Corneal Diameter measurement, IOL power, Intraocular tension and fundus examination. Cases that had poor fundus view and all unilateral cases were subjected to B-scan ultrasonography. Serological screening for congenital infections was done in selected cases. Presence of nystagmus and ocular deviation was noted. Children with strabismus underwent detailed orthoptic evaluation including prism bar cover test, tests for the presence of BSV and stereopsis. It was noted if the child could alternate fixation between the two eyes. Cycloplegic refraction was done in possible cases. Any associated anomalies were also noted. In children less than 1 year of age, IOL was deferred. A-scan axial length measurement and K reading was done for IOL power calculation. Lens aspiration with primary IOL implantation, primary posterior capsulotomy and anterior vitrectomy was planned for children aged less than 8 years and lens aspiration with primary IOL alone was planned for children aged greater than 8 years. After obtaining informed consent from the parent or the guardian, for the surgery and placement of IOL children were operated on under inhalational general anaesthesia. Surgical technique. Superior rectus bridle’s suture was applied. Fornix based conjunctival flap was raised. Wet field cautery was done to cauterize the bleeding vessels. Scleral tunnel was performed superiorly. Two side ports were made at 3 & 9’o clock positions. After entering the anterior chamber with the keratome, the chamber was filled with viscoelastic. Manual continuous curvilinear capsulorhexis (CCC) was performed. Thorough cortical aspiration was done manually with Irrigation/Aspiration cannula. Posterior CCC smaller in size than the optic diameter was done, followed by anterior vitrectomy. Posterior capsule was left intact in children above 8years. PMMA IOL was placed in the bag. The surgical wound was sutured in all cases. Post operative care. All children received topical steroids hourly, moxifloacin eye drops 6 times a day and cycloplegics twice a day. Topical steroids were continued and tapered of in 4-12 weeks, antibiotics for 6 weeks and cycloplegics were discontinued after 2 weeks. Children were reviewed every day for the first day and then every week for the first month and every 3 months for the first year. Visual acuity for near and distance, with and without correction was recorded during each visit. Anterior segment examination was done with Slit lamp and Fundus was examined with direct or indirect ophthalmoscope under full dilatation. Retinoscopic refraction was done and refractive errors were corrected. Children were prescribed bifocal spectacles. Posterior Capsule Opacification (PCO) which caused visual obscuration were detected and taken up for either YAG laser or surgical capsulotomy. The eyes were well dilated before the procedure. Using a minimum energy of 1 to 2 mJ a sufficient opening was made in the centre of the posterior capsule. 1% prednisolone acetate eye drops, 2% homatropine eye drops, 0.25% timolol maleate eye drops were prescribed for a week after the procedure. Five cases received occlusion therapy as a part of amblyopia treatment. Statistics. Data was analysed by statistical software and Microsoft excel. Data was summarised by mean +/- SD for continuous data and percentages for categorical data. The comparison between variables was done by chi-square test/fisher’s exact test for categorical data. All p values <0.05 were considered statistically significant. Results Demographics. Majority of the eyes were between 2-8 years 23 (51.11%). < 1year 10 (22.22%) eyes and > 8-16 years 12 (26.66%) eyes were included in the present study. The mean age of presentation of the children was 5.84±4.3 years. In this study, boys outnumbered girls, 17 (56.67%) were boys, 13 (43.3%) were girls. Chief complaint of Visual Inattentiveness / defective vision was observed in 29 (64.4%) of eyes, and remaining 16 (35.5%) eyes had white opacity. In the present study 26 (87%) patients had bilateral cataract and 4 (13%) patients had unilateral cataract. Consanguinity. 67% of patients had no history of consanguinity. History of consanguinity among parents was present in 13 (33%) children. Morphology. The commonest type of cataract was found to be total cataract in the present study in 20 eyes (44.44%), followed by lamellar cataract in 22.22% (10) of eyes. This could account for the increased incidence of bilaterality in our study. Associated ocular anomalies. Nystagmus was present in 6 (20%) patients. Nystagmus was found to be common in children having defective vision since birth. Of the 5 (11.11%) cases of strabismus, 3 had exotropia and 2 had esotropia. Posterior lenticonus was seen in 2 (6.66%) eyes. Microcornea was seen in 1 (3.33%) patient. Associated systemic anomalies. In the present study, 4 cases had congenital heart disease (2 ASD,1 PA stenosis,1 PA stenosis with PDA. History of epilepsy associated with delayed birth cry is present in 2 children. A history of febrile seizures is present in 2 children. 1 case of thalassemia major is included. 1 child of Marfan’s syndrome is included in this study. Pre operative visual acuity. At the time of presentation, out of 45 eyes with cataract, 21 (46.66%) eyes had fixing and following light. 14 (31.11%) eyes presented with vision less than 3/60. 2 (4.44%) eyes had vision between 6/60 & 3/60,5 (11.11%) eyes had vision 6/24 -6/60 and 3 (6.66%) eyes had vision better than 6/18 (Table 1).
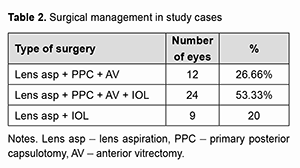
Surgical management. Out of 45 eyes operated 12 (26.66%) eyes underwent lens aspiration with primary posterior capsulotomy and anterior vitrectomy, 24 (53.33%) eyes underwent lens aspiration with primary posterior capsulotomy, anterior vitrectomy with IOL implantation and 9 (20%) eyes underwent only lens aspiration and IOL implantation (Table 2).
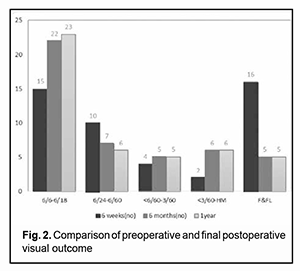
Post-operative visual outcome. After 6 weeks postoperatively, vision greater than 6/18 was seen in 15 eyes (33.33%). Vision within this category was seen in 23 eyes (51.11%) at the end of 12-months. Vision less than 6/18 was seen in 30 eyes (66.66%) at the end of 6 weeks, which reduced to 22 eyes (48.88%) by the end of 12 months (Figure 2). It shows significant improvement in visual acuity at 1 year postoperatively compared to preoperative visual acuity. p-value is <0.0001 indicates highly significant difference between pre and post-operative visual acuity.
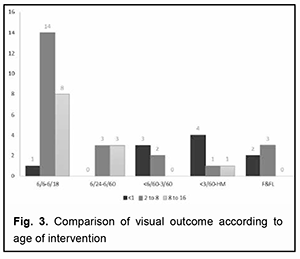
Comparison of visual outcome according to age of intervention. It shows a difference in visual acuity in different age groups because nearly half of the study population were between >1 to 8 years. P-value is 0.008 indicates a highly significant difference in visual acuity among different age groups. The postoperative visual acuity was observed to be better in patients between 1 to 8 years when compared to other age groups (Figure 3).
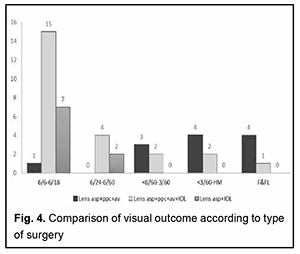
Comparison of visual outcome according to type of surgery. It shows a significant (p value=0.002) difference in visual acuity postoperatively in different types of surgery. This indicates better visual acuity in cases undergoing lens asp + ppc + av + IOL than other types of surgeries (Figure 4).
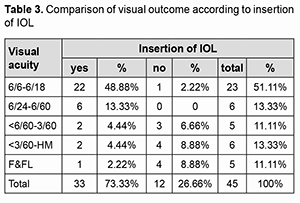
Comparison of visual outcome according to insertion of IOL. There is a significant (p value=0.0001) difference in visual acuity among patients who underwent IOL insertion and among those who did not undergo IOL insertion. In patients who underwent IOL insertion, visual acuity was comparatively better (Table 3).
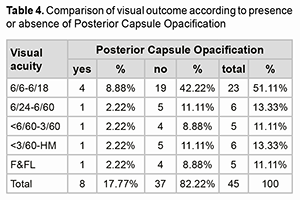
Comparison of visual outcome according to PCO. There is no significant (p value=1.000) difference in visual acuity among patients with or without the development of PCO. As the patients were followed regularly and underwent YAG CT when required no significant difference in visual acuity was observed (Table 4).
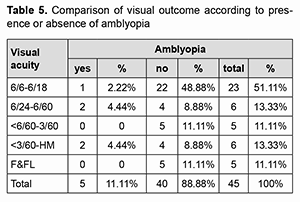
Comparison of visual outcome according to amblyopia. There is no significant (p value=0.081) difference found in final visual acuity among patients with or without amblyopia. As the patients underwent patching therapy improvement in visual acuity was observed at the final follow-up (Table 5).
Early post operative complication. The most common early postoperative complications were striate keratopathy & corneal oedema in 4 (8.88%)eyes and AC cells in 4 (8.88%) eyes. Late postoperative complications.The most common late post-operative complication was PCO. Posterior capsular opacification was seen in 8 (17.77%) eyes, followed by Amblyopia, Optic capture, Anterior synaechiae, and Vitreous haemorrhage in 5 (11.1%), 2 (4.4%), 1 (2.2%), and 1 (2.2%) eyes respectively. Discussion The paediatric eye is not simply a miniaturised adult eye, surgery should be performed by an experienced surgeon and the postoperative course needs to be monitored carefully. Paediatric cataract surgery differs from adult cataract surgery in many ways. There may be a delay in a presentation associated with amblyopia, the sclera is less rigid, the axial length & refractive status keep on changing, chances of postoperative inflammation and PCO are higher. Hence, the visual results of paediatric cataract surgery are less spectacular than adult cataract surgery. Nonetheless, the intervention is very much needed as a child’s vision restored is a great achievement in terms of blind person-years saved. In this study, visual outcome after surgery was assessed in 45 eyes of 30 patients below the age of 16 years. 15 patients underwent bilateral cataract surgery during my study period. Most of patients belong to the age group of >1-8 years (51.11%). The mean age of presentation in the present study was 5.84 years with SD ± 4.3. The mean age of surgery in a study conducted by Rohit Khanna et al. [9] in South India was 55.2 months. In a study conducted by Nikhil et al in Maharashtra, the mean age of presentation was 7.6 years. The main reason for the late presentation being lack of awareness and poor socioeconomic status. The present study included 24 eyes (53.33%) of 17 boys and 21 eyes (46.66%) of 13 girls, thereby pointing slightly towards preponderance in boys. Out of 215, 131 (60.9%) patients were boys in South Indian study by Rohit Khanna et al. [9]. In a study conducted in Maharashtra by Nikhil et al., 55% were boys and 45% were girls[10]. The distribution of boys and girls were almost equal (52%) boys and (48%) girls in a study conducted in Nepal [11]. In a study in North east India by Damaris et al male preponderance with males (68.5%) and females (31.4%) was found [12]. The preponderance of boys is more likely the result of the greater value accorded to male children in traditional societies, rather than to an increased incidence of cataract in boys. In the present study, a total of 87% patients had bilateral cataract. There was no significant difference in visual acuity in bilateral and unilateral cataracts because patients with unilateral cataracts were given occlusion therapy and thereby showed significant improvement in visual acuity at 1 year follow up period. Increased ratio of bilateral cataract had been observed in other studies as which were conducted in Maharashtra (73.6%) by Rishikesh Nikhil et al., China (72.4%) by Fanguin M et al. Nepal by Santosh Chaudary et al., [13] (80%)and in Nepal (83%) by Thakur et al. [11]. The possible reason of bilaterality might be due to exclusion of traumatic cataracts, which are most of the time unilateral. History of consanguity among parents in the present study was present in 33% of patients. This was found to be similar in south Indian study where history of consanguity was present in 37.7%. In the present study, the most common morphological types of cataract were total (44.44%) and lamellar (22.22%). In a study conducted in Nepal by Thakur et al., the most common type of cataract was total (32%) followed by lamellar (31%). Wilson et al also showed total cataract (68.5%) as the most common morphological variant. Damaris Magdalene et al found that 48.08% were a lamellar type of cataract in his study [14]. This might be one of the reasons for late presentation in developing countries like ours i.e unless the cataract is fully mature and white, it goes undetected. The commonest symptom of presentation in the present study was defective vision/ visual inattentiveness (64.44%). In a study conducted in Nepal by Santosh Chaudary et al, the most common chief complaint was a defective vision (53.3%). Whereas in a study conducted in Nepal by Gurung R. L. the commonest presenting complaint was white pupillary reflex (54%). Associated ocular anomalies. Nystagmus was observed in the patients with early bilateral cataract in whom treatment was delayed or who showed poor compliance with postoperative rehabilitation. Nystagmus was associated with cataract in 15.55% patients eyes. In South Indian study by Rohit Khanna et al. [9] study the association was 35.8% and in Dahod study by Mehul A. Shah, it was 17% [15]. The existence of nystagmus plays an important role in functional visual prognosis. As expected, nystagmus persisted in all the cases post-operatively. Early surgery associated with immediate optical correction may eliminate this problem. Squint was present in 11.11% eyes in the present study. It was found to be similar to South Indian study by Rohit Khanna (14.4%) and also study in North Carolina (19%). Preoperative visual acuity. Preoperatively visual acuity was most commonly recorded by Snellen’s chart (53.33%) and fixation pattern (46.66%). In Rohit Khanna study the methods of recording preoperative visual acuity were fixation pattern (59.5%) and Snellen’s pattern (35.3%). In our study, 30 eyes (66.66%) had visual acuity < 6/60 in better eye (defined as poor fixation and visual acuity <6/60). In Rohit Khanna study preoperative visual acuity <6/60 in the better eye was found in 47.4% patients. This explains delayed presentation in our study 13 (28.88%) had visual acuity <6/60 in better eye post-operatively when compared to 30 (66.66%) eyes preoperatively with visual acuity <6/60 in better eye. In this study, we used SRK/T, HofferQ, Holladay and Haigis formulae. In the present study hydrophobic and three-piece IOL’s were implanted in the bag. The material and design of IOL greatly influence the incidence of PCO following cataract surgery. Gagandeep et al. showed that the implantation of square-edged PMMA and hydrophobic acrylic lens had a similar outcome on PCO in paediatric cataract surgery [16]. Surgical technique. Usually, lens aspiration (lens asp) + primary posterior capsulotomy (PPC), anterior vitrectomy (AV) was done in children < 1 year. Lens asp + PPC + AV + IOL was done in between age 2 to 8 years. Lens asp + IOL implantation was done in children > 8 years of age. Children less than 8 years had undergone primary posterior capsulotomy with anterior vitrectomy, as children above 8 years were found to be less prone to PCO formation and mature enough to co-operate for YAG capsulotomy if needed. The following 4 eyes are special conditions in which the surgery according to age was not performed. - In a child of age 15 months IOL was deferred as there is associated microcornea and nystagmus. - In a child of 13 months of age with posterior lenticonus, IOL was deferred as the child was found to have insufficient PC support. - In a 12-year patient ppc and av were also done as he was having posterior lenticonus. - 1 child of age 9 years who is mentally retarded underwent posterior capsulotomy with anterior vitrectomy as it is anticipated that he may not co-operate for YAG capsulotomy. 73.33% eyes had primary IOL implantation in the present study. The placement of IOL in children and infants undergoing cataract surgery is gaining wider acceptance. Whereas in Rohit Khanna study it was 62.3%. In our study, 80% of patients in the present study underwent ppc and av whereas it was found to be about 50% in other studies. Most of the children presented in the present study were of age group 2-8 years who were subjected to lens aspiration + ppc + av + IOL. This explains the higher percentage of patients undergoing lens aspiration + PPC + AV in our study. Best Corrected Visual Acuity (BCVA) at one-year postoperative period: The comparison of best-corrected visual acuity at 1 year of age in the present study with other studies. In the present study at 1-year postoperative period, visual acuity of more than 6/60 was observed in 64.44% eyes whereas in Rohit Khanna et al study it was 82.3%. This was explained by delayed presentation and poor pre-operative visual acuity in the present study. 5 eyes with poor pre-operative vision (fixing & not following light) had poor postoperative visual acuity. The reduction in the mean Snellen acuity in 4 eyes (2 at 1 year postoperatively and 2 at 6 months postoperatively) is due to development of posterior capsular opacification & vitreous haemorrhage in 1 eye. Good visual outcome could be attained in 64.44% of patients (6/60 and more) due to adoption of secure incisions, hydrodissection, primary posterior capsulotomy and anterior vitrectomy in our study. Binocular vision in good percentage of cases could be attained if the patient is taken for surgery at an earlier date. Postoperative complications: The most common postoperative complication (PCO) after paediatric cataract surgery was found to be posterior capsule opacification. In the present study PCO was seen in 8 eyes (17.77%). In Rohit Khanna et al study its incidence was 27.4%. PCO rate was comparatively lower in the present study when compared to Rohit Khanna et al because the percentage of eyes undergoing ppc+av in the present study was 80% whereas in Rohit Khanna et al study was 47.5%. PCO rate was anticipated to be lower in eyes with ppc and av. Visual Axis Opacification (VAO) was not present at initial follow-ups, however, the number increased to 2 (4.44%) on 6th month and 6 (13.33%) by 1 year. PCO was thick enough to require capsulotomy in 4 eyes. The 2 cases presented during 6 months of postoperative period and 1 case during the 1-year postoperative period underwent YAGCT. Surgical membranectomy was needed in 1 eye (1-year postoperative period). Only 1 patient did not show improvement in vision after YAGCT. The results of PCO were controversial in this study as there was more number of children who underwent ppc and av in the present study, insufficient ppc & av and inflammatory response were suspected to contribute to increased incidence of PCO in the present study. 5 (11.11%) eyes had amblyopia. They were given occlusion therapy according to their age. These cases showed significant improvement in visual acuity after effective patching. Pupillary capture, IOL decentration was also responsible for decreased vision in 2(4.44%) eyes. 1 case underwent anterior vitrectomy at 6 weeks postop period for PAS. One serious complication occurred in a child with thalassemia major. The patient developed CRVO with vitreous and subhyaloid haemorrhage and secondary glaucoma postoperatively. Damaris Magdalene et al. (2017) in their study, they observed the most common associated ocular condition was nystagmus in 20% eyes. The most important factor associated with poor visual outcome was amblyopia (38.2%) [14]. Santosh Chaudhary et al. (2017) conducted a prospective study in eastern Nepal on factors affecting the visual outcome of paediatric cataract surgery. Early age of presentation, presence of nystagmus and poor preoperative visual acuity were found to be statistically associated with poor visual outcome postoperatively while sex, duration, laterality, strabismus, cataract morphology and IOL implantation had no association with visual outcome. Primary posterior capsulotomy with anterior vitrectomy significantly reduces the chance of visual axis opacification [13]. In a study by Anjita Hirachan et al. (2018), there was a statistically significant improvement in postsurgical BCVA (p<0.001) [17]. Gurung et al. (2018) study revealed that statistically significant improvement in vision was observed postoperatively in all the eyes (p < 0.0001). Visual axis opacification was the most common postoperative complication seen in 26% of total eyes by the end of 6 months18. Limitations of the study include children attending our hospital does not represent the incidence of congenital cataract in the community. As the children are in growing age more complications tend to occur as the age advances. Their follow-up period of at least 2years is ideal. There is no standard protocol to compare visual acuity in different age groups like fixing and following pattern, Cardiff cards and Snellen’s chart. Therefore, we were unable to categorise visual outcome exactly. Strengths of the study include this study was well executed as children < 8 years underwent lens aspiration+pp+av+IOL and children > 8 years underwent lens aspiration+IOL so that we can get a better visual outcome. As it is a tertiary eye care centre, the number of cases included in the study were relatively more. All the patients had timely follow-up and any complication observed was managed at the appropriate time. Conclusion There was male predominance in this study. Total cataract and lamellar cataract were the common type of cataract, which led to significant reduction in visual function. Most of the children brought, were less than or equal to 8 years of age, even if their cataract wasn’t visually significant, showing awareness amongst the parents, teachers and paediatricians. Strabismus due to visual deprivation in this study stresses the need for early intervention, especially in unilateral cases. Children less than 8 years who underwent primary posterior capsulotomy with or without anterior vitrectomy showed good visual outcome, supporting the role of primary posterior capsulotomy and anterior vitrectomy. PCO is the commonest complication and a major cause for visual obscuration following surgery, though the incidence of PCO has been brought down with modified surgical techniques and newer IOL designs. The incidence of Pupillary capture and IOL decentration was less probably due to the, in the bag fixation of the IOL, made possible by CCC. Children who underwent YAG/surgical capsulotomy had significant visual gain. Children with amblyopia who had strict adherence to occlusion therapy had significant improvement in visual acuity. References 1.Taylor HR. Refractive errors – Magnitude of the Need. J Community Eye Health 2000;13:1-2. 2.World Health Organization. Prevention of blindness and deafness.Global Initiative for the Elimination of Avoidable Blindness. WHO Document WHO/PBL/97.61 Rev 2. Geneva: WHO; 2000. 3.Gilbert CE, Canovas R, Hagan M, Rao S, Foster A. Causes of childhood blindness: Results from west Africa, south India and Chile. Eye (Lond) 1993;7(Pt 1):184-8. 4.Dandona L, Williams JD, Williams BC, Rao GN. Population-based assessment of childhood blindness in southern India. Arch Ophthalmol 1998;116:545-6. 5.Rahi JS, Sripathi S, Gilbert CE, Foster A. Childhood blindness in India: Causes in 1318 blind school students in nine states. Eye(Lond) 1995;9(Pt 5):545-50. 6.Giles K, Cristelle D,Y annick B, Fricke OH, Wiedemann P (2016).Cataract surgery with intraocular lens implantation in children aged 5-15 in local anaesthesia:visual outcomes and complications.Pan Afr.Med J;24:200. 7.Ma F, Wang Q, Wang L. Advances in the management of the surgical complications for congenital cataract. Front Med. 2012; 6(4):360–5. 8.Clare G (2009).Worldwide causes of blindness in chidren, in: Paediatric Ophthalmology: Current Thought and A Practical Guide. Springer, Berlin: 47-60 9.Khanna RC, FosterA, KrishnaiahS, MehtaMK, GogatePM. Visual outcomes of bilateral congenital and developmental cataracts in young children in south India and causes of poor outcome.Indian J Ophthalmol 2013;61:65-70. 1. Gilbert C. New issues in childhood blindness. Commun Eye Health J. 2001;14:53–56PPMID: 17491932 10.Nikhil R, ShubhiT, AnushreeKA, SudhirT, MadanD. Evaluation of visual outcomes after paediatric cataract surgery in a tertiary eye care hospital in western Maharashtra. J Clin Ophthalmol Res 2016;4:13-8. 11.Thakur J, Reddy H, Wilson ME Jr, Paudyal G, Gurung R, Thapa S, Tabin G, Ruit S. Pediatric cataract surgery in Nepal. J Cataract Refract Surg. 2004; 30(8):1629–35. 12.BarSela SM, Spierer A. Astigmatism outcomes of scleral tunnel and clear corneal incisions for congenital cataract surgery. Eye (Lond)2006;20:1044 8. 13.Chaudary S et al, Visual outcome of Paediatric Cataract surgery, Nepal J Ophthalmol 2017;Vol 9(18): 143-148 14.Damaris Magdalene et al. Pediatric cataract blindness management and outcomes in North East India hospital based study Damaris Magdalene 1 , Indian Journal of Clinical and Experimental Ophthalmology, January-March,2017;3(1): 112-114 15.Shah MA, Shah SM, Appleware AH, Patel KD, Rehman RM, Shikhange KA, et al. Visual outcome of traumatic cataract in pediatric age group. Eur J Ophthalmol 2012;22:956 63. 16.Brar GS, Grewal DS, Ram J, Singla M, Grewal SP. Square-edge polymethylmethacrylate intraocular lens design for reducing posterior capsule opacification following paediatric cataract surgery: initial experience. Clinical & experimental ophthalmology. 2008 Sep;36(7):625-30. 17.Hirachan A, Bajracharya K, Rai SK, Bhari AM, Chandra A. Visual outcome of congenital and developmental cataract surgery in Lumbini Eye Institute. Asian Journal of Medical Sciences. 2018 Mar 1;9(2):36-9. 18.Gurung RL, Adhikari S, Shrestha UD, Ruit S. Outcome of Paediatric Cataract Surgery at Tilganga Institute of Ophthalmology, Nepal. Birat Journal of Health Sciences 2018;3(1)5 : 331-337. Conflict of interest: None. Funding sources: None
|