J.ophthalmol.(Ukraine).2021;6:69-72.
|
http://doi.org/10.31288/oftalmolzh202166972 Received: 12 April 2021; Published on-line: 21 December 2021 A case of OCT evidence of retinal breaks in a myopic patient woman at 38 weeks of gestation O. V. Ivanytska, O. Iu. Terletska, G. V. Levytska SI "The Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine"; Odesa (Ukraine) TO CITE THIS ARTICLE: Ivanytska OV,. Terletska OIu, Levytska GV. A case of OCT evidence of retinal breaks in a myopic patient woman at 38 weeks of gestation. J.ophthalmol.(Ukraine). 2021;6:69-72. http://doi.org/10.31288/oftalmolzh202166972 Background: An eye examination of a pregnant woman is a mandatory phase of her preparation for delivery, with a special attention given to ophthalmic symptoms and relevant recommendations for delivery management. Purpose: To examine spectral domain ocular coherence tomography (SD-OCT) changes in retinal periphery and to provide grounds for the tactics of preparing a pregnant woman for delivery by performing preventive peripheral laser photocoagulation (PPLP). Material and Methods: A 35-year-old myopic woman at 38 weeks of gestation underwent a routine eye examination (visual acuity assessment, refractometry, tonometry, perimetry, biomicroscopy, and ophthalmoscopy), ultrasound biometry and SD-OCT (Heidelberg Engineering). Results: The patient was diagnosed with mild myopia along with peripheral lattice degeneration and peripheral cystic degeneration of the retina in both eyes and local retinal detachment with atrophic retinal breaks in the right eye. The peripheral vitreoretinal lattice degeneration was arrested and the local retinal detachment was limited by laser-induced chorioretinal adhesions. Conclusion: Spectral domain ocular coherence tomography provides an objective picture of the state of both the macular and the periphery of the retina, and, along with biomicroscopy and ophthalmoscopy, provides grounds for the tactics of care for pregnant women for preventing retinal detachment. The outcome of timely preventive laser treatment allowed us to conclude that the patient had no ocular contraindications to vaginal delivery. Keywords: peripheral retinal degeneration, rhegmatogenous retinal detachment, spectral domain ocular coherence tomography, myopia, pregnancy, retinal laser photocoagulation
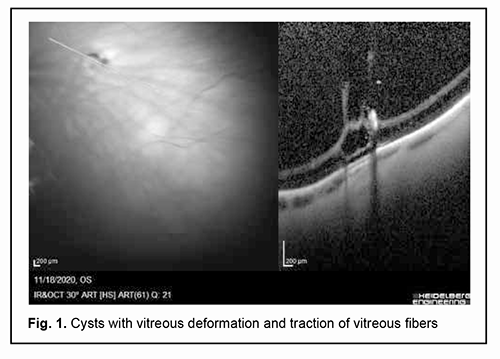
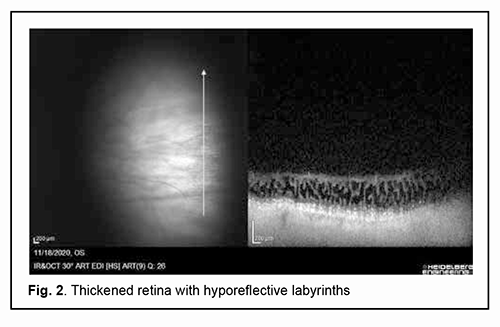
Introduction An eye examination of a pregnant woman is a mandatory phase of her preparation for delivery, with a special attention given to ophthalmic symptoms and relevant recommendations for labor and/or cesarean delivery management. Approaches to this issue are controversial. It was long thought that high myopia as a threat of retinal detachment was an ocular indication for cesarean delivery. According to the Ministry of Health regulations (Order No.977 ‘Indications for a Planned Cesarean Section‘ of December 27, 2011) [1], the list of ocular indications for a planned cesarean section included only hemorrhagic retinopathy, perforated corneal ulcers, penetrating globe injury, and a fresh burn injury to the eye. It is noteworthy that high myopia has been excluded from the list of indications for a planned cesarean section due to the advances in medical technologies and the increased potential for performing peripheral laser photocoagulation. Preventive peripheral laser photocoagulation (PPLP) is effective for prevention of rhegmatogenous retinal detachment (RRD) and is performed if peripheral retinal degeneration is detected, with the type and severity of this degeneration determined by mydriatic ophthalmoscopy. It has been reported that the peripheral retinal degeneration requiring PPLP was detected not only in patients with high myopia, but also in those with moderate myopia, mild myopia, emmetropia or hypermetropia [2, 3]. Among patients with any peripheral retinal degeneration, those with vitreoretinal forms like lattice degeneration and snail-track degeneration bear the highest risk of retinal detachment [4-8]. A PPLP should be performed not later than 4 weeks before estimated delivery date to allow enough time for laser-induced chorioretinal adhesions to form, since it is these adhesions that prevent retinal detachment [1, 9]. Below we report a case that may be of interest to practitioners in the area. Material and Methods A 35-year-old woman at 38 weeks of gestation presented with complaints of decreased vision. She reported that when she was of school age she was diagnosed with mild myopia and wore glasses. At the age of 32 years, she was seen by an ophthalmologist at a private clinic who made a diagnosis of mild myopia and retinal degeneration with breaks in the periphery of the right eye. The patient received a preventive peripheral laser photocoagulation OD. The unaided visual acuity was 0.2 OD and 0.2 OS. Her best-corrected visual acuity was 1.0 OD with -2.0 D sph, and 1.0 OS with -2.0 D sph. Her spherical refraction as assessed by autorefractometry was -1.75 D OD and -1.75 OS. Refraction at presentation was -2.25 D sph., -0.25 D cyl., axis 166° OD and -2.25 D sph., -0.5 D cyl., axis 171° OS. The unaided visual acuity was 0.15 OD and 0.15 OS. Her best-corrected visual acuity was 0.9-1.0 OD with -2.5 D sph, and 1.0 OS with -2.5 D sph. The intraocular pressure (IOP) was 16.0 mmHg OD and 15.0 mmHg OS. Axial length measured by ultrasound was 24.04 mm OD and 23.94 mm OS. Corneal thickness was 0.477 mm OD and 0.474 mm OS. On examination, the anterior segment was unremarkable, and there was destruction of the vitreous body OU. In addition, mydriatic ophthalmoscopy (1% cyclomed) showed initial posterior hyaloid detachment OU. In the right eye, foci of annular PPLP were seen somewhat peripherally near the equator, but the lattice degeneration in the superior temporal retinal quadrant as well as the local retinal detachment with atrophic retinal breaks was not arrested. The left eye showed a zone of lattice degeneration with thinned retina. In addition, the patient was diagnosed with cystic retinal degeneration. She underwent SpectralisTM Spectral Domain-Optical Coherence Tomography (SD-OCT, Heidelberg Engineering GmbH, Heidelberg, Germany) to clarify the status of the retina and optic nerve. A routine OCT examination of the macula, optic nerve and peripapillary retina was followed by examination of the peripheral temporal and superior peripheral temporal zones of the retina. Scanning was performed with a medically dilated pupil and with the head turned in the direction of the maximum possible eye movement to allow for the maximum angle of view. During scanning, refraction was corrected to enable the optimum image sharpness and signal power. Of the linear scans acquired, the sharpest and most informative images were selected. Our OCT data analysis showed concave (myopic) deformation of the retina, with no changes in the retinal contour, thickness or structure in the macular region in both eyes. The optic nerve was intact, and the peripapillary nerve fiber thickness was not decreased in both eyes. OCT examination of the peripheral temporal and superior peripheral temporal zones of the retina with the patient’s head turned in the direction of the maximum possible eye movement demonstrated signs of peripheral retinal degeneration (Figs 1, 2).
The diagnosis made was as follows: complicated mild myopia, vitreoretinal peripheral degeneration with retinal breaks, and destruction of the vitreous body (incomplete posterior hyaloid detachment) OU; and the state after preventive peripheral laser photocoagulation with a local rhegmatogenous retinal detachment OD. Given the patient’s history, SD-OCT data, and ophthalmoscopic and slit lamp exam findings (to be exact, prognostically unfavourable bilateral peripheral lattice degeneration and three retinal holes), a decision was made to perform a repeat laser photocoagulation. A laser photocoagulation was performed to prevent expansion of the retinal detachment in the right eye as well as to prevent retinal detachment in the left eye. The zone of lattice degeneration in the symmetric meridians in the superior temporal retinal quadrants was surrounded by laser burn spots, whereas the extension of the inferior temporal retinal detachment with atrophic retinal breaks beyond the orra serrata in the right eye was limited by laser-induced chorioretinal adhesions. The intervention was performed under mydriasis induced by 1% cyclomed (one drop was instilled three times, 15 minutes apart) 3 days after performing a diagnostic assessment and making a diagnosis, with no intraoperative or postoperative complications. At two-weeks, follow-up examination found that the lattice degeneration was arrested, and the retinal detachment was limited by adequate chorioretinal adhesions. Discussion and Conclusion The reasons why this case may be of interest to practitioners in the area are as follows. The presence of the peripheral retinal degeneration requiring PPLP in a female patient with mild myopia, which confirms the findings of others that the zones of peripheral vitreochorioretinal degeneration (PVCRD) in the fundus may be detected in pregnant women with moderate myopia, mild myopia, emmetropia or hypermetropia [3, 6, 8]. In this connection, some authors [2, 5, 8] believe that barrier laser photocoagulation of PVCRD zones and retinal tears with a creation of a strong laser coagulation barrier around these zones or tears is an effective means for preventing retinal rhegmatogenous detachment. In addition, an SD-OCT apparatus (Heidelberg Engineering GmbH) was used to visualize structural changes in the retina in a patient with peripheral retinal degeneration. We have managed to find in the literature only a few images of these changes, and all these images had been obtained with time-domain OCT systems whose resolution is substantially worse than that of an SD-OCT apparatus. Our patient received a PPLP for preventing retinal detachment at 38 weeks of gestation, which is a rather late time point in a routine period of woman’s preparation for delivery. However, adequate laser-induced chorioretinal adhesions formed by the time of delivery, which allowed for uncomplicated vaginal delivery. The outcome of timely preventive laser treatment allowed us to conclude that the patient had no ocular contraindications to vaginal delivery. These findings highlight the value of receiving a preventive medical examination by myopic pregnant women and a compulsory mydriatic fundus periphery examination irrespective of the severity of myopia (1% cyclomed was found to be effective for this purpose and had no negative consequences). A high-resolution SD-OCT system (Heidelberg Engineering) allows objective and clear imaging of structural changes in retinal periphery and relevant vitreous compartments; this provided grounds for conducting PPLP with proper details and with an adequate dose of laser energy for these changes. Ongoing monitoring of PPLP treatment outcome is mandatory, given the possibility of post-PPLP progression of posterior vitreous detachment, increased retinal traction and development of retinal tears or detachment.
References 1.[Order of the Minister of Health of Ukraine No. 977 of December 27, 2002 “An Obstetrics Protocol for Cesarean Delivery”]. Ukrainian. 2.Pasyechnikova NV. [Laser treatment for pathology of the fundus]. Kyiv: Naukova Dumka; 2007. Ukrainian. 3.Popova NV, Fabrikantov OL, Goidin AP. [Frequencies of various clinical forms of peripheral vitreoretinal lattice degeneration for myopia of different severities]. Vestnik TGU. 2017;22(6):1484-6. Russian. 4.Astakhov IS, Lukovskaia NG. [Retinoschisis. 1. Diagnosis, classification, examination methods]. Vestn Oftalmol. Jan-Feb 2004;120(1):26-9. Russian. 5.Neroev VV, Zakharova GY, Kondratieva YP. [Laser photocoagulation for retinoschisis]. In: [Proceedings of the 6th Russian National Ophthalmological Forum: Collection of Papers]. Moscow; October 1-3, 2013. p.59-62. Russian. 6.Shaimova VA, Pozdeeva OG, Shaimov TB, et cal. [Optical hoherence tomography in the diagnosis of peripheral vitreoretinal degeneration]. Oftalmologiia. 2013;10(4):32-9. Russian. 7.Dragoumis I, Richards A, Alexander P, et al. Retinal detachment in severe myopia. Lancet. Lancet. 2017 Jul 8;390(10090):124. 8.Kottow M. Peripheral retinal degenerations and breaks. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1980;214(1):53-60. 9.Kolenko OV, Sorokin EL, Fil AA. [Ophthalmological criteria for choice of optimal mode of delivery in pregnant women with myopia]. Akusherstvo, ginekologiia i reproduktsiia. 2019;13(2):155-163. https://doi.org/10.17749/2313-7347.2019.13.2.156-163. Russian. Conflict of Interest: The authors declare no conflict of interest which could influence their opinions on the subject or the materials presented in the manuscript.
|