J.ophthalmol.(Ukraine).2021;5:14-20.
|
http://doi.org/10.31288/oftalmolzh202151420 Received: 24 May 2021; Published on-line: 23 October 2021 Evaluation of corneal distortion characteristics in different eyes using Scheimpflug camera device Sbordone S., MD, Ragucci A., MD, Iaccarino G., MD, Scognamiglio G., MD, Serra L., MD, Gironi Carnevale U.A., PhD, Lanza M., MD, PhD Dipartimento Multidisciplinare di Specialità Mediche, Chirurgiche e Odontoiatriche, Università degli studi della Campania “L. Vanvitelli” Napoli (Italy) E-mail: mic.lanza@gmail.com TO CITE THIS ARTICLE: Sbordone S, Ragucci A, Iaccarino G, Scognamiglio G, Serra L, Gironi Carnevale UA, Lanza M. Evaluation of corneal distortion characteristics in different eyes using Scheimpflug camera device. J.ophthalmol.(Ukraine).2021;5:14-20.http://doi.org/10.31288/oftalmolzh202151420 Objective. To study the correlations between corneal distortion and morphological features in different kinds of eyes such as healthy ones (HE), ones previously undergone myopic PRK (PRKE), ones affected by keratoconus (KCE) and keratoconus eyes previously undergone corneal collagen crosslinking (CCCE). Materials and Methods. In this retrospective comparative study, a total of 106 HE of 106 patients, 58 PRKE of 58 patients, 33 KCE of 33 patients, 28 CCCE of 28 patients were included. A complete examination of all eyes was followed by tomographic (Pentacam, Oculus, Wetzlar, Germany) and biomechanical (Corvis ST, Oculus, Wetzlar, Germany) evaluation. Differences among Corvis ST (CST) parameters in the different groups have been analyzed. Linear regressions between central corneal thickness (CCT), intraocular pressure (IOP) and anterior corneal curvature measured with Simulated Keratometry (SK), versus corneal deformation parameters measured with Corvis ST in the different groups, have been run using SPSS software version 18.0. Results, HE showed a significant correlation between main curvature power of the cornea within the central 3 mm expressed in Diopters (KM) and 6 CST parameters; between CCT and 4 CST parameters and between IOP and 5 CST parameters. PRKE showed a significant correlation between KM and 3 CST parameters; between IOP and 4 CST parameters and none between CCT and CST parameters. KCE showed a significant correlation between SK and 3 CST parameters; between IOP and 3 CST parameters and none between CCT and CST parameters. CCCE showed a significant correlation between KM and 5 CST parameters; between CCT and 1 CST parameters and between IOP and 5 CST parameters. Discussion. Data of this study suggest that both corneal curvature and IOP could have a greater influence on the corneal deformation, compared to central corneal thickness (CCT). These results should be taken into account by further studies aiming to assess biomechanical corneal characteristics. Кey words: сorneal deformation; corneal crosslinking; Corvis ST, keratoconus, refractive surgery
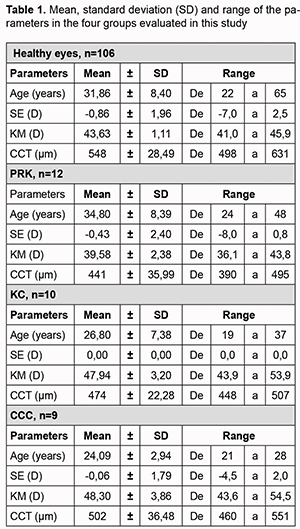
Introduction. Recent advances in technology applied to ophthalmology provide the possibility to study the corneal biomechanical properties, using the ocular response analyzer (ORA; Reichert Ophthalmic Instrument, Depew, NY, USA) [1]. This device was able to perform the first in vivo measurements of corneal properties such as corneal hysteresis (CH) and corneal resistance factor (CRF), using a collimated air pulse to applanate the central cornea [1]. This instrument allowed physicians to evaluate new corneal parameters more than central corneal thickness (CCT), curvature and transparency. Different studies showed that CH and CRF are somehow influenced also by corneal morphological parameters [2, 3, 4, 5], and this is one of the reasons why new technologies, such as optical coherence tomography, are recently applied to corneal biomechanical evaluation [6, 7, 8, 9]. A very accurate evaluation of corneal biomechanics would play a very important role in managing alterations due to corneal diseases (i.e., keratoconus) or to iatrogenic causes (i.e., refractive surgery). Moreover, it would help in better measuring the intraocular pressure (IOP), especially in eyes affected by corneal diseases, since the current gold standard, Goldmann applanation tonometry (GAT), has been largely proven to be biased by corneal properties [10, 11, 12]. The Corvis ST (Oculus, Wetzlar, Germany) (CST) is an innovative device able to investigate corneal deformation properties; it uses an ultrahigh-speed Scheimpflug camera that records the deformation process in 4330 frames/sec along an 8 mm horizontal corneal coverage, while an air puff indentation determines a corneal deformation [9]. Evaluating the most important papers previously published about CST evaluation of corneal deformation, it is clear that there are still veiled aspects of this analysis that this device is able to provide in different kind of eyes [9, 13, 14, 15, 16, 17]. The purpose of this study is to evaluate differences and correlations in corneal behaviors in healthy eyes (HE) and in ones with a very different structure and morphology such as eyes that underwent myopic PRK (PRKE), keratoconus affected eyes (KE), and keratoconus affected eyes that underwent corneal cross-linking (CCCE) using a Scheimpflug camera based device. Materials and Methods In this retrospective study, were included 106 HE of 106 healthy subjects with a mean refractive error of −0.65 ± 1.68D (measured as spherical equivalent); 58 PRKE of 58 patients previously undergone myopic PRK for a mean refractive defect of −5.93 ± 2.08D; 33 KE of 33 patients affected by keratoconus (stages 1, 2 and 3 of Amsler classification) and 28 CCCE of 28 patients affected by keratoconus. Every eye underwent a complete ophthalmic evaluation, a corneal tomography performed using Pentacam, a CST scan. IOP evaluation with Goldmann applanation tonometry was run at last, in order to not introduce any bias in corneal biomechanical evaluation. PRKE and CCCE were included if they had surgery at least 1 year before starting the present study. Patients with systemic and/or ocular diseases that could interfere with the corneal evaluation, such as diabetes, connective tissue disorders, dry eye, uveitis, corneal opacities and glaucoma were excluded from this study. Subjects wearing contact lenses were asked to stop using them at least 7 days before being evaluated. Details of different groups of patients are summarized in Table 1.
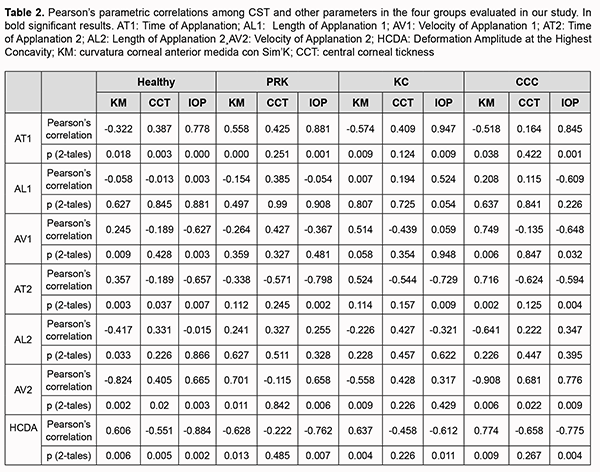
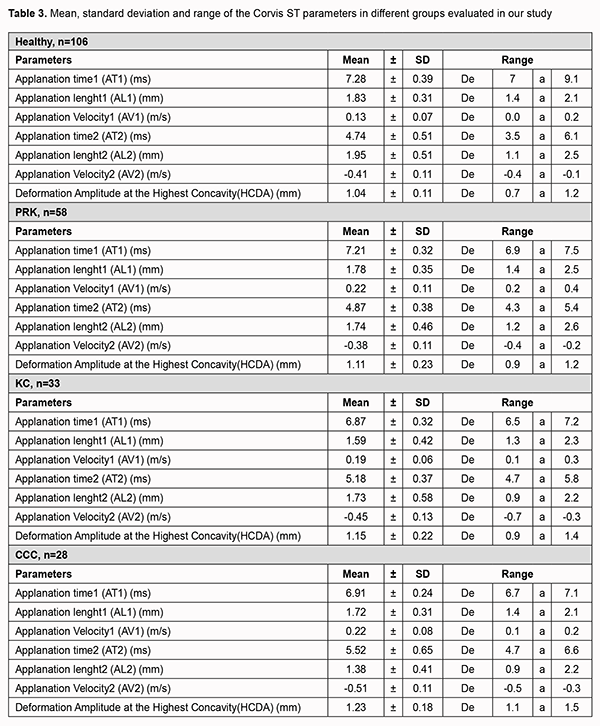
PRKE were enrolled in this study did not have any complications as corneal ectasia and/or corneal haze; they were evaluated at least 1 year after surgery, showing no refractive and topographic changes from the previous follow-up. KE received diagnosis and were staged according to Amsler classification (18 were at stage 1, 11 were at stage 2, and 4 were at stage 3). CCCE (15 were at stage 1, 8 were at stage 2 and 5 were at stage 3 of Amsler classification) underwent treatment with epithelium removal and according to the Dresden Protocol. These patients were evaluated at least 1 year after treatment and were enrolled only if they did not report any complications. Evaluations between data before and after procedures such as myopic PRK and CCC were not performed because these were patients referring to our Unit but treated in other hospitals, and data were not available. The Oculus Pentacam is a corneal tomographer utilizing a rotating Scheimpflug camera, largely used by ophthalmologists, and its working principles are well known [18]. For this study, the 25 images per scan option were chosen. The parameters provided by Oculus Pentacam that we evaluated in this study were central corneal thickness (CCT) at pupil center and anterior corneal curvature measured with simulated keratometry SK). The Corvis ST (CST) is a noncontact tonometer that measures corneal deformation; parameters included in this study were the following: Time of Applanation 1 (AT1): time from the start until an air puff causes the corneal flattening (first applanation); Length of Applanation 1 (AL1): length of the flattened cornea in the first applanation; Velocity of Applanation 1 (AV1): velocity of corneal deformation during the first applanation; Time of Applanation 2 (AT2): time from the highest concavity until cornea restores its standard curvature; Length of Applanation 2 (AL2): length of the flattened cornea in the second applanation; Velocity of Applanation 2 (AV2): velocity of corneal deformation during the second applanation; Deformation Amplitude at the Highest Concavity (HCDA): maximum deformation amplitude (from the start to the highest concavity) at the corneal apex. Three good quality Corvis ST measurements have been taken and every scan has been performed after 5 minutes from the previous one, aiming to avoid an underestimation or overestimation of the corneal biomechanical parameters. All subjects started with the Pentacam evaluation and then underwent the CST one, aiming to reduce bias in morphological measurements, since the air puff could introduce errors in corneal evaluation if Scheimpflug scan is performed after it. Two different and trained physicians used the two devices (GI used Pentacam and AR used CST) and they were not aware of the results obtained by the other. Despite the fact that all patients underwent bilateral evaluation, only the right eye data were included in the statistical analysis in order to eliminate any potential intra-subject effect that may occur if both eyes of the same patient were considered. All study participants gave their informed consent for using their data before starting every visit. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Università della Campania Luigi Vanvitelli as retrospective study. Statistical Analysis. The fulfilment of the data requirements for parametric analysis (normality, homogeneity of variance) was assessed by specific tests (Kolmogorov-Smirnov, Levene). All groups were compared with one-way factorial analysis of variance (ANOVA) for each parameter, followed by post hoc test LSD for single comparison. Moreover, the correlations among SK, CCT, IOP, and corneal deformation parameters measured with CST were evaluated using parametric (Pearson) test. For all tests adopted, the level of significance was set at p < 0.05. All analyses were performed using SPSS software version 18.0 (IBM Corp. Armonk, New York, USA). Results Age and main corneal parameters of the four groups are summarized in Table 1. Correlation between CST and Pentacam parameters are summarized in Table 2.
In particular, in HE AT1 showed positive correlations with CCT and IOP and inverse ones with SK. Similar correlations with IOP and SK are also present in KE and CCCE groups. Also in the PRKE group, correlations with IOP and SK are positive. AV1 showed a positive correlation with SK and a negative one with IOP in HE and CCCE groups. AT2 showed a positive correlation with SK and a negative correlation with pachymetry and IOP in the healthy group; the positive correlation with SK and the negative one with IOP were also present in the CCCE group. In the PRKE and KE groups AT2 was negatively correlated with IOP values. For AL2 there was only a negative correlation with SK in the healthy group. AV2 was correlated positively with pachymetry and IOP and negatively with SK in healthy and CCCE groups. Positive correlations with SK and IOP were present in the PRKE group. In the KE group AV2 was negatively correlated with SK values. HCDA showed a positive correlation with SK and a negative one with pachymetry and IOP in the healthy group. Similarly, positive correlations with SK and negative ones with IOP were present in KE and CCCE groups while negative correlations with SK and IOP appeared in the PRKE group. The means and ranges of corneal deformation parameters recorded in the different groups are summarized in Table 3.
AT1 values in HE and post-PRK groups were statistically higher than the ones found in KC and post-CCC groups (p < 0.000). Post hoc least significant difference (LSD) test gave significant differences between the KC and the healthy group (−5.6%, p < 0.000), the CCC and the healthy group (−6.9%, p < 0.000), and the CCC and the PRK group (−4.5%, p < 0.016). ConverselY, AT2 values in healthy and post- PRK groups were statistically lower than the ones recorded in KC and post CCC groups (p < 0.000). Post hoc LSD test gave significant differences between the KC and the healthy group (+8.7%, p < 0.009), the CCC and the healthy group (+14%, p < 0.000), and the CCC and the PRK group (10.9%, p < 0.013). AL2 was significantly higher in the healthy eyes group than in the others (p < 0.007). Post hoc LSD test gave a significant difference only between the CCC and the healthy group (−25%, p < 0.001). Even AV2 was significantly higher in the healthy eyes group than in others (p < 0.000). For the healthy eyes group, post hoc LSD test gave significant differences versus PRK (−16.6%, p < 0.022), KC (−24.1%, p < 0.001), and CCC (−31.6%, p < 0.000). Finally, HCDA in healthy and post-PRK groups was statistically lower than the one found in KC and post-CCC groups (p < 0.000). Post hoc LSD test gave significant differences between the KC and the healthy group (+10.0%, p < 0.003), the CCC and the healthy group (+16.7%, p < 0.000), the KC and the PRK group (+8.8%, p < 0.031), and the CCC and the PRK group (+15.4%, p < 0.000). Discussion To accurately evaluate the biomechanical properties of the cornea could be crucial for the diagnosis and follow-up of different eye diseases. The possibility to evaluate corneal deformation with more than a device such as ORA and CST, provided to study it from a different point of view. To better understand corneal behavior during shape modifications due to external stress would be very important to improve our knowledge about problems of current practice such as [9]: • to obtain more precise values of IOP, especially after corneal surgery; • to better understand the pathological processes involved in corneal degenerative diseases like keratoconus, in which we observe a change both in shape and biomechanics; • to better screen corneas undergoing refractive surgery in order to avoid complications like corneal ectasia. It is important to highlight that AT2 values, as provided by CST, are the total of milliseconds calculated from the start of deformation until the flattened cornea rebounds from its highest concavity, reaching the second applanation. In order to achieve a better understanding of corneal shape-changing process, we used the value obtained subtracting AT2, provided by the device, to AT1 (time from the start of examination until an air puff causes the first corneal applanation). In this way, we obtained the time needed by the cornea to come back to a flat position after reaching the maximum deformation (HCDA) and, in our opinion, this value provides us a better idea of the time taken by the cornea to come back to its original shape after a deformation. AT2 in fact, as it is possible to read on CST display, is the total time from the start of the analysis, so if we had studied this parameter, our analysis about the difference between the corneal resistance to external modification and the capability of the cornea to return to its original shape after a deformation may have been biased. According to our results, corneas that are affected by KC, even if they underwent CCC, seem to reach applanation easier than healthy and post PRK ones, showing less resistance to outer deformation forces; moreover, it seems like they take longer time to return to the applanation position and so recover the original shape. It is interesting to observe that corneas after PRK did not show the same deformation characteristics, as if the corneal thinning they underwent during refractive surgery did not influence much their behavior compared to healthy corneas in answering stress coming from outside. Moreover, healthy and post-PRK eyes showed higher AT1 and lower AT2 compared to KC eyes and post- CCC eyes. Both KC and post-PRK corneas have morphological and structural differences with healthy ones; according to our data it is possible to imagine that KC induces deeper structural changes in the overall corneal cellular and extra-cellular structure making these tissues easier to modify. This kind of alteration seems to be related not just to the corneal thinning; furthermore, these changes prevent reaching the original shape after modifications due to external factors. The higher deformation that KC and post CCC corneas could have is confirmed by the higher values of HCDA observed, compared with healthy and post-PRK ones. Observing results of this study, KM shows a significant correlation with some of the CST parameters analyzed (AT1, AT2, VA2, and HCDA) whereas CCT does not show a significant correlation in the post-PRK, KC, and post-CCC groups. Both KM and CCT show a significant correlation with AT1, AT2, VA2, and HCDA in healthy corneas. This could mean that KM is able to deeper influence the corneal deformation compared to CCT in diseased corneas. This influence, however, does not seem to be the same in the four groups studied. In particular, AT1 showed values negatively correlated to SK in HE, KE and CCCE, meaning a higher difficulty in applanating flatter corneas; whereas in PRKE that an opposite correlation has been observed. Previous data suggest that KE and CCCE corneas seem to be easier to modify in shape, so it is simple to imagine that the higher the corneal curvature is in healthy eyes, the less the time it takes to applanate them. In PRKE, however, the opposite tendency has been observed, so it seems that the flatter the cornea is, the easier it is to applanate. A possible explanation for this behavior is that the tissue ablation in PRKE makes corneas weaker to external deformations. Thus, the greater the flattening is, the faster it is possible to achieve the corneal applanation. Interestingly, in this study the same correlations between CST parameters and CCT has not been observed. IOP values are directly correlated with AT1 and AV2 and inversed correlated with AV1, AT2, and HCDA in every group analyzed. Only in KE AV2 is directly related but without significant value. These results mean that the resistance that IOP apply to deformation and the help that it lends in restoring the original corneal shape are effective in HE, KE, PRKE and CCCE. The not significant value observed in AV2-IOP correlation in KE could be due to two factors: (1) the small number of KE group biased the analysis; (2) IOP could not influence the corneal speed to come back at its original shape after a deformation, but this characteristic could depend by some other ultra-structural properties. Values provided by CST in different groups studied let think that corneal deformation induced by keratoconus (such as corneal curvature and thinning) is deeper and affects more the whole cornea, making it easier to deform, compared to corneal deformation induced by PRK treatment. Corneal deformation analysis is a very interesting topic because understanding how the corneas (both healthy and altered ones) react to external stress could let physicians to better understand how make earlier diagnosis and how to better manage corneal diseases. This study confirms some of the findings previously published [8,19,20,21] and provides some different results compared to other ones [22,23,24,25]. Differences observed in the different studies could be related to many reasons: populations analyzed are very different, so are the inclusion and exclusion criteria adopted. One of the main limits of this study is its design: it’s a retrospective study. This did not allow to provide further analysis and evaluations that could have been very useful such as the comparison of the CST data and the correlations with other features studied before and after surgery and over time. Another limitation is the dimensions of the evaluated samples; of course these data need to be confirmed in larger population study. Even if this kind of study has just been purposed, it is important to confirm some findings in different studies to provide more strength to the recent discoveries. Conclusions In conclusion, this study suggests some considerations not deeply investigated such as the differences in reaction between KCE and PRKE ones or the heavier influence of SK on corneal deformation compared to CCT. Further studies, with larger populations and more data are needed to fully understand how to use the corneal deformation parameters provided by CST in clinical practice to screen eyes undergoing refractive surgery, eyes with keratoconous at early stage, ectatic corneas, or other corneal diseases.
References 1.Luce DA. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. Journal of Cataract and Refractive Surgery. 2005;(31):156-162. 2.Martinez-de-la-Casa JM, Garcia-Feijoo J, Fernandez-Vidal A, Mendez-Hernandez C, Garcia-Sanchez J. Ocular Response Analyzer versus Goldmann Applanation Tonometry for Intraocular Pressure Measurements. Investigative Ophthalmology & Visual Science. 2006;(47):4410-4414. 3.Terai N, Raiskup F, Haustein M, Pillunat LE, Spoerl E.Identification of biomechanical properties of the cornea: the ocular response analyzer. Current Eye Research. 2012;(37):553-562. 4.Hurmeric V, Sahin A, Ozge G, Bayer A. The relationship between corneal biomechanical properties and confocal microscopy findings in normal and keratoconic eyes. Cornea. 2010;(29):641-649. 5.McMonnies CW. Assessing corneal hysteresis using the Ocular Response Analyzer. Optometry and Vision Science. 2012;(89):E343-349. 6.Kotecha A, Elsheikh A, Roberts CR, Zhu H, Garway-Heath DF. Corneal Thickness and Age Related Biomechanical Properties of the Cornea Measured with the Ocular Response Analyzer. Investigative Ophthalmology & Visual Science. 2006;(47):5337-5347. 7.Narayanaswamy A, Chung RS, Wu RY, Park J, Wong WL, Saw SM et al. Determinants of corneal biomechanical properties in an adult Chinese population. Ophthalmology. 2011;(118):1253-1259. 8.Ma, J.; Wang, Y.; Wei, P.; Jhanji, V. Biomechanics and structure of the cornea: implications and association with corneal disorders. Surv Ophthalmol. 2018, 63, 851-861 9.Lanza, M.; Iaccarino, S.; Bifani, M. In vivo human corneal deformation analysis with a Scheimpflug camera, a critical review. J Biophotonics. 2016, 9, 464-77 10.Ortiz D, Piñero D, Shabayek MH, Arnalich-Montiel F, Alió JL.Corneal biomechanical properties in normal, post-laser in situ keratomileusis, and keratoconic eyes. Journal of Cataract and Refractive Surgery. 2007;(33):1371-1375. 11.Liu J, Roberts CJ. Influence of corneal biomechanical properties on intraocular pressure measurement: quantitative analysis. Journal of Cataract and Refractive Surgery. 2005;(31):146-155. 12.Kara N, Altinkaynak H, Baz O, Goker Y. Biomechanical Evaluation of Cornea in Topographically Normal Relatives of Patients With Keratoconus. Cornea. 2013;(32):262-266. 13.Kotecha A. What biomechanical properties of the cornea are relevant for the clinician?. Survey Ophthalmology. 2007;(52):109-114. 14.Lanza M, Cennamo M, Iaccarino S, Romano V. et al., Bifani M, Irregolare C, Lanza A. Evaluation of corneal deformation analyzed with a Scheimpflug based device. Cont Lens Anterior Eye. 2015 Apr;38(2):89-93. 15.Rosa N, Lanza M, De Bernardo M, Signoriello G, Chiodini P. Relationship Between Corneal Hysteresis and Corneal Resistance Factor with Other Ocular Parameters. Semin Ophthalmol. 2015;30(5-6):335-339 16.Huseynova T, Waring GO 4th, Roberts C, Krueger RR, Tomita M. Corneal biomechanics as a function of intraocular pressure and pachymetry by dynamic infrared signal and scheimpflug imaging analysis in normal eyes. American Journal of Ophthalmology.2014;157:885-893 17.Ma, J.; Wang, Y.; Wei, P.; Jhanji, V. Biomechanics and structure of the cornea: implications and association with corneal disorders. Surv Ophthalmol. 2018, 63, 851-861 18.Reznicek L, Muth D, Kampik A, Neubauer AS, Hirneiss C. Evaluation of a novel Scheimpflug-based non-contact tonometer in healthy subjects and patients with ocular hypertension and glaucoma. British Journal of Ophthalmology. 2013;97:1410-1414. 19.Kuryan, J.; Cheema, A.; Chuck, R.S. Laser-assisted subepithelial keratectomy (LASEK) versus laser-assisted in-situ keratomileusis (LASIK) for correcting myopia. Cochrane Database Syst Rev. 2017, 2, CD011080. 20.Herber, R.; Vinciguerra, R.; Lopes, B.; Raiskup, F. et al. Repeatability and reproducibility of corneal deformation response parameters of dynamic ultra-high-speed Scheimpflug imaging in keratoconus. J Cataract Refract Surg. 2020, 46, 86-94. 21.Yu, M.; Chen, M.; Dai, J. Comparison of the posterior corneal elevation and biomechanics after SMILE and LASEK for myopia: a short- and long-term observation. Graefes Arch Clin Exp Ophthalmol. 2019, 257, 601-606. 22.Hashemi, H.; Asgari, S.; Mortazavi, M.; Ghaffari, R. Evaluation of Corneal Biomechanics After Excimer Laser Corneal Refractive Surgery in High Myopic Patients Using Dynamic Scheimpflug Technology. Eye Contact Lens. 2017, 43, 371-377. 23.Lanza M, De Rosa L, Sbordone S, Boccia R, Gironi Carnevale UA, Simonelli F. Analysis of Corneal Distortion after Myopic PRK. J Clin Med. 2020 Dec 28;10(1):82. doi: 10.3390/jcm10010082. 24.Guo, H.; Hosseini-Moghaddam, S.M.; Hodge, W. Corneal biomechanical properties after SMILE versus FLEX, LASIK, LASEK, or PRK: a systematic review and meta-analysis. BMC Ophthalmol. 2019, 19, 167. 25.Abd Elaziz, M.S.; Elsobky, H.M.; Zaky, A.G.; Hassan, E.A.M.; KhalafAllah, M.T. Corneal biomechanics and intraocular pressure assessment after penetrating keratoplasty for non keratoconic patients, long term results. BMC Ophthalmol. 2019, 19, 172.
Conflict of interest statement: None. Funding sources: None
Received 24.05.21
|