J.ophthalmol.(Ukraine).2021;4:67-71.
|
http://doi.org/10.31288/oftalmolzh202146771 Received: 12 June 2021; Published on-line: 16 August 2021 Efficacy of orthokeratology lenses depending on topograpy pupil diameter and lens optical zone size R. A. Parkhomets Kharkiv National Medical University; Raduzhka Pediatric Ophthalmology Center; Kharkiv (Ukraine) E-mail: radaparhomets@gmail.com TO CITE THIS ARTICLE: Parkhomets RA. Efficacy of orthokeratology lenses depending on topograpy pupil diameter and lens optical zone size. J.ophthalmol.(Ukraine). 2021;4:67-71. http://doi.org/10.31288/oftalmolzh202146771 Background: Management of progressive myopia is a major issue in current optometry and oph-thalmology in general. Refractive therapy with orthokeratology lenses (OKL) has become an in-creasingly popular technique for controlling the progression of myopia. Purpose: To assess the efficacy of orthokeratology lenses depending on the topography pupil size and lens optical zone (OZ) size. Material and Methods: Sixty children (117 eyes) with mild or moderate uncomplicated myopia were involved in this study. They underwent a comprehensive eye examination, corneal topography and pupillometry. Statistical analysis of correlations between the pupil diameter and axial elongation was performed. In order to conduct longitudinal surveillance of myopia, we compared two OKL designs, one with a conventional OZ diameter, and another with a smaller OZ diameter, for the efficacy of myopia control. Results: The pupil diameter was inversely correlated with the axial elongation both in mild myopes (r = -0.48, p < 0.001) and in moderate myopes (r = -0.7, p < 0.001). Patients showed slower axial length progression when treated with a 5.5-mm OZ lens design than with a conventional 6.0-mm OZ lens design. Conclusion: When examining a child with progressive myopia, it is important to pay attention to the photopic pupil size because the size may be a predictor of myopia progression and exert an influ-ence on the choice of correction. Orthokeratology lenses with a smaller (5.5-mm) optical zone diam-eter are more effective for myopia control, which should be taken into consideration when selecting a lens design for children. Keywords: myopia, refractive therapy, orthokeratology lenses, corneal topography, pupil diameter
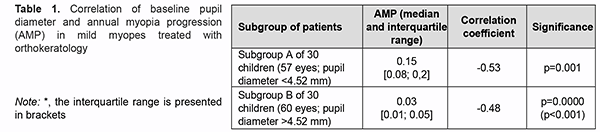
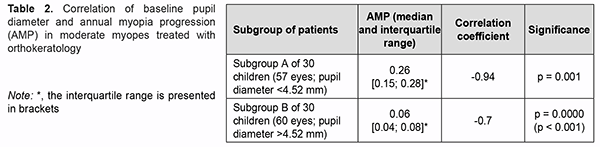
Introduction The prevalence of myopia has been growing globally in recent years, reaching epidemic levels in some countries [1-7]. Myopia ac-counts for 12.38% of ocular disease, and is the second most common ocular disease among the Ukrainian population aged 18 years or older [1, 4]. According to a Ukrainian national statistical report for the years 2014 to 2017, myopia prevalence rate was 35.57 and 84.86 for every 1000 children aged 7 to 14 years, and 15 to 17 years, respectively, which was ten-fold higher and 23-fold higher, re-spectively, than (3.68) for every 1000 children aged 6 years or younger [3]. In addition, progressive myopia is a major disabiliting disease, accounting for 80% of cases of childhood visual disability and 32.7% of cases of pediatric blindness in Ukraine [4, 6, 8]. Refractive therapy with orthokeratology lenses (OKL) of various designs has become an increasingly popular technique for controlling the progression of myopia. There are several potential mechanisms of myopia control with OKL such as a myopic shift in peripheral refractive error that results in peripheral myopic defocus after or-thokeratology. Myopic defocus involves refraction of the rays falling upon the paracentral and peripheral retina. In myopic peripheral defocus, the amount of refraction is greater at the periphery than at the center, whereas in hy-peropic peripheral defocus, the amount of refraction is greater at the center than at the periphery of the retina [9-13]. Thus, the size of the pupil determines the amount of light that enters the eye. A narrow pupil will intercept a particularly large share of peripheral light rays. Studies demonstrated that OKL cause a myopic shift in peripheral defocus at far periphery (30°). From this point of view, the size of the pupil may influence the contribution of my-opic peripheral defocus to the efficacy of refractive therapy with OKL. Foreign studies investigated the influence of the size of the pupil on the axial elongation in myopic patients after refractive therapy with OKL. Thus, Chen and colleagues [14] concluded that a large pupil increases the efficacy of OKL, slowing axial elongation in myopia. However, Downie and Lowe [15] found no significant association of the size of the pupil with the reduction in the rate of progression of childhood myopia. Therefore, new OKL designs try to increase myopic peripheral defocus and take into consideration an increased contribution of higher-order aberrations from larger pupil diameters [16-17]. These lenses are being developed with a smaller optical zone in attempts to produce a more powerful midperipheral ring closer to the pupil center. To the best of our knowledge, only two studies have reported on the effects of orthokeratology lens design on the cornea [18-19]. Carracedo and colleagues [19] aimed to evaluate the effect of the optical zone diameter (OZ) in or-thokeratology contact lenses regarding the topographical profile in patients with high myopia (-4.00 D to -7.00 D) and to study its effect over the visual quality. They found that, compared with a larger diameter optical zone (6 mm), a smaller diameter optical zone (5 mm) in orthokeratology lenses has a very different keratometric profile in the X-axis, with the changes between central cornea and peripheral ring more abrupt, increasing higher-order aberra-tions. This profile difference means that smaller OZ produces a narrower treatment area and a wider and steeper peripheral ring, closing the steepening ring to the pupil center. Since there is paucity of studies on this subject, further research was required. The purpose of the study was to assess the efficacy of orthokeratology lenses depending on the topography pupil size and optical zone of the lens. Material and Methods The study adhered to the Declaration of Helsinki. Written informed consent was obtained from parents. Sixty children (117 eyes; age, 7 to 15 years) with mild or moderate uncomplicated myopia were involved in this study. Of these, 37 (61.7%) were female, and 23 (38.3%) were male. Fifteen individuals (27 eyes (23.1%)) had mild myopia (3 D or less) and 45 (90 eyes (76.9%)) had moderate myopia (3.25 D – 6.0 D). All study subjects Moonlens orthokeratology lenses (manufactured by SkyOptix, Moscow, Russia, under license from KATT Design Group, Vancouver, British Columbia, Canada). They underwent surveillance over 24 months. At baseline, they underwent a comprehensive eye examination, including visual acuity assessment with a Chart projector (CCP-3100; Huvitz, South Korea), subjective and objective refraction, and autorefractometry with an Opto Chek Plus Autorefrac-tor/Keratometer (Reichert; USA). Refraction measurements were performed in the first half of the day. Refraction was measured separately for each eye before and after pharmacological cycloplegia (40 minutes after the first in-stillation) which was achieved by double instillation of 1% cyclopentolate eye drops (Alcon, Fort Worth, Texas, USA) as per the manufacturer’s instructions. An ultrasonic A-scanner (Pirop® Ultrasonic Biometer A-Scan, Echo-Son, Krancowa, Poland) was used to perform ocular biometry, and a slit lamp (SL9900, CSO, Florence, Italy) was used to perform anterior eye biomicroscopy. In addition, an Oculus Easygraph corneal topographer (Oculus, Dutenhofen, Germany) was employed to perform corneal topography before orthokeratology lenses were pre-scribed and at each scheduled visit. Easygraph software was used to visualize the results on four topography maps. Keratometry and pupillometry readings were taken, and corneal eccentricity in the flat meridian and the steep me-ridian as well as corneal diameter was determined. The study included two phases: Phase I, determining the effect of the pupil size on axial length growth, and Phase II, comparing optical zones of OKL of various diameters for the effectiveness of myopia control. Statistica 10.0 (StatSoft, Tulsa, OK, USA) software was used for statistical analysis. The Kolmogorov–Smirnov test, Lilliefors and Shapiro-Wilk tests were used to explore data distribution normality. Data are presented in the form of the number of observations in the group, median and interquartile range (IQR), since, in most cases, data distribution was not normal. The Mann-Whitney rank test was employed to assess differences between the groups. The level of significance p ≤ 0.05 was assumed. Results The baseline pupil diameter, as assessed by pupillometry, ranged from 2.78 mm to 6.30 (median, 4.52 mm; IQR, 4.07 to 5.02). Patients were divided into two subgroups of 30 children each, based on the diameter of the pupil: subgroup A (57 eyes; 48.7%) with a pupil diameter smaller than the median (< 4.52 mm), and subgroup B (60 eyes; 51.3%) with a pupil diameter larger than the median (> 4.52 mm). In patients with mild myopia, the baseline pupil diameter was inversely correlated with the annual axial length progression, that is, the smaller the diameter, the greater the annual myopia progression (Table 1).
Similar results were obtained for patients with moderate myopia. Particularly, the highest inverse correlation of -0.94 (p < 0.001) (Table 2) was observed for subgroup A (patients with a pupil diameter smaller than the median).
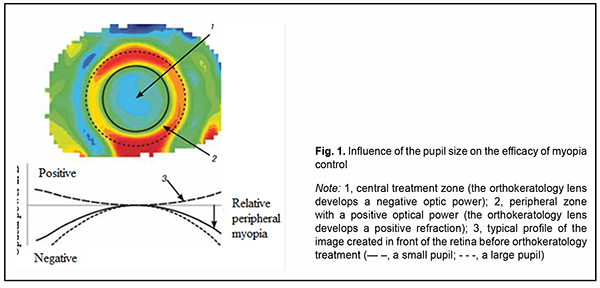
We suggest that these findings may be explained by the fact that, the larger the pupil, the larger the amount of light reaching the periphery of the retina. As OKL cause a myopic shift in peripheral defocus at far periphery, the size of the pupil may influence the development of the process. In addition, giving the role of high-order aberrations in arresting myopia progression, it is higher-order aberrations from a large pupil that have a role in myopia control in the presence of OKL (Fig. 1).
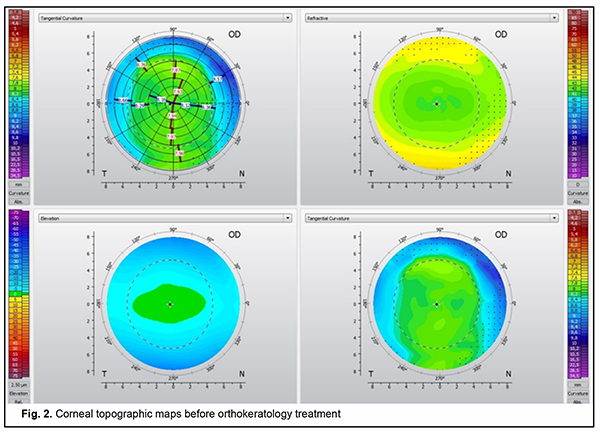
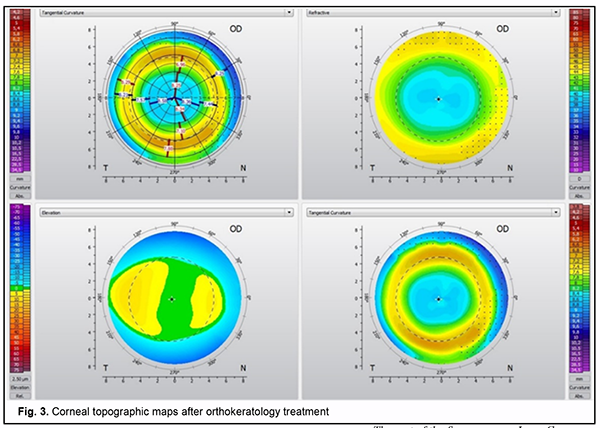
Only thirty patients (57 eyes) with a pupil diameter smaller than the median (<4.52 мм) were involved in Phase II of the study, and, consequently, myopia control was less efficacious. These children were fitted with custom-designed orthokeratology lenses with a 5.5-mm optical zone diameter for the second year of the study. Subsequent-ly, we compared OKL with a conventional 6.0-mm optical zone diameter used in the first year with custom-designed OKL with a 5.5-mm optical zone diameter used in the second year of the study in the same patient with regard to myopia control efficiency. Patients were optimally fit with lenses with adequate centration during the first and the second years. Corneal topographic profile undergoes changes with orthokeratology like central corneal flattening and in-creased peripheral ring refraction at the 6-mm zone. These changes are demonstrated by the differential corneal topography map (Figs. 2 and 3).
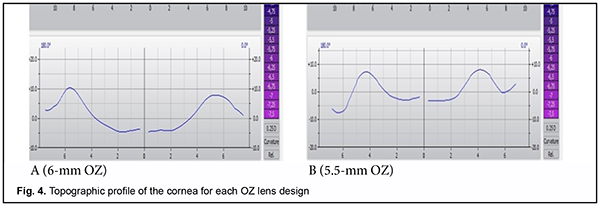
Fig. 2 shows axial, tangential, and refractive and elevation topography maps of the cornea before OKL selec-tion. Fig. 3 shows post-orthokeratology topography maps of the cornea, with the formation of the optical zone and the peripheral refractive ring corresponding to the return zone of the lens. The keratometry profile of the cornea forms in each patient depending on the diameter of the optical zone of the lens which we believe subsequently will exert a major influence on the formation of peripheral defocus. The keratometric or topographic profile of the cornea for each OZ lens design is shown in Fig. 4A, B.
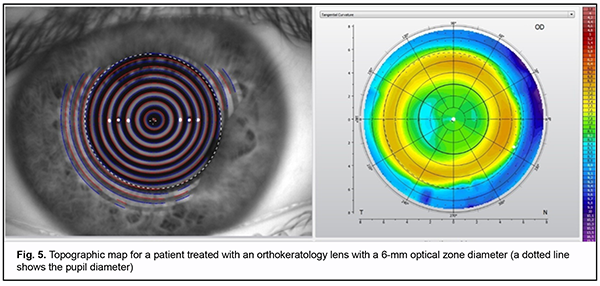
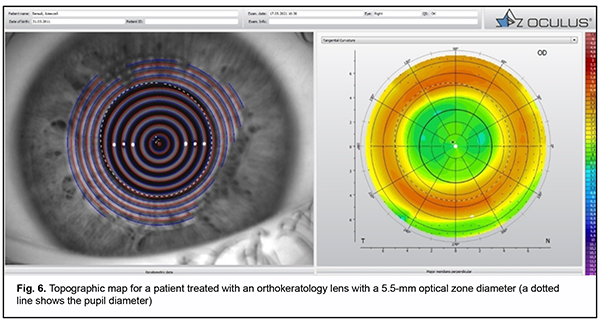
The 5.5-mm OZ lens design produced greater central flattening greater midperipheral steepening than the 6.0-mm OZ lens design (Fig. 4). In patients with the 6.0-mm OZ lens design, the pupil was partially in the treatment zone, whereas in those with a pupil diameter smaller than the median, the pupil was not in the treatment zone (Figs 5 and 6). In patients with the 5.5-mm OZ lens design, the pupil was completely within the treatment zone, suggesting a more efficient myopia control.
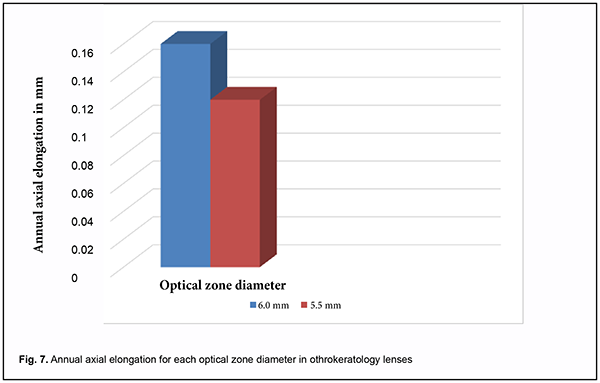
During a year of refractive therapy with the 6.0-mm OZ lens design, the median annual increase in axial length was 0.16 mm (IQR, 0.1 mm to 0.23 mm). This was larger than the median annual increase in axial length of 0.12 mm (IQR, 0.1 mm to 0.2 mm) for a year of refractive therapy with orthokeratology lenses with a 5.5-mm optical zone diameter for the same patients (Fig. 7).
Discussion Our findings are in agreement with the recent findings of Carracedo and colleagues [19] who found that com-pared with a larger diameter optical zone, a smaller diameter optical zone in OKL has a very different keratometric profile in the X-axis, increasing higher-order aberrations. That is, this difference in the keratometric profile means that a smaller diameter optical zone in OKL produces a wider and steeper corneal peripheral ring which completely embraces the zone of pupil projection, and likely increases the effect of higher order aberrations on myopia control. We, however, believe that, when selecting the orthokeratology lens OZ diameter for a pediatric patient, it is the pupil diameter that is the most important to take into consideration, since it can be considered the most significant prog-nostic factor for effective myopia progression control by orthokeratology. We found that refractive therapy with orthokeratology lenses enabled the most efficient myopia control in pro-gressive myopia and a baseline pupil diameter smaller than 4.52 mm. Orthokeratology lenses with a smaller (5.5-mm) optical zone diameter exerted a more profound arresting effect on axial elongation, and, correspondingly, are more effective for myopia control, which should be taken into consideration when selecting a lens design for chil-dren. In general, when examining a child with progressive myopia, it is important to pay attention to the photopic pupil size because the latter may be a predictor of myopia progression.
References 1.Pan CW, Ramamurthy D, Saw SM. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt. 2012; 32(1): 3–16. 2.Smirnova IIu, Larshyn AS. [Current visual status among schoolchildren: prospects and challenges]. Glaz. 2011;3:2-8. Russian. 3.Moiseienko EO, Golubchikov MV, Mykhalchuk VM, Rykov SO. [Ophthalmological care in Ukraine in 2014-2017]. Kropyvny-tskyi: Polium; 2018. Ukrainian. 4.Poveshchenko IuL. [Clinical characteristics of disabling myopia]. Medychni perspektyvy. 1999;3:66-9. Ukrainian. 5.Mingazova EM, Samoilov Shiller SI. [Role of social and medical factors in the development of myopia]. Kazanskii meditsinskii zhurnal. 2012;6:958-61. Russiаn. 6.Lytvynchuk LM, Sergiienko AM, Rikhard G, et al. [Frequency of retinal complications in high myopia]. Ukrainskyi medychnyi almanakh. 2012; 5:109–10. Ukrainian. 7.Vitovska OP, Savina OM. [[The structure and sickness rate of eye and adnexa diseases in children in Ukraine]. Medicni perspek-tivi. 2015;3:133-8. Ukrainian. 8.Rykov SO, Varyvonchyk DV. [Pediatric blindness and visual impairment in Ukraine: a situation analysis]. Kyiv: Logos; 2005. Ukrainian. 9.Lee EJ, Lim DH, Chung TY, Hyun J, Han J. Association of axial length growth and topographic change in orthokeratology. Eye Contact Lens. 2018; 44:292–8. 10.Chakraborty R, Read SA, Collins MJ. Hyperopic defocus and diurnal changes in human choroid and axial length. Optom Vis Sci. 2013; 90(11):1187–98. 11.Charman WN, Jennings JA. Longitudinal changes in peripheral refraction with age. Ophthalmic Physiol Opt. 2006;26:447–55. 12.Charman WN, Radhakrishnan H. Peripheral refraction and the development of refractive error: a review. Ophthalmic Physiol Opt. 2010;30:321–38. 13.Chen X, Sankaridurg P, Donovan L, et al. Characteristics of peripheral refractive errors of myopic and nonmyopic Chinese eyes. Vision Res. 2010;50:31–5. 14.Chen Z, Niu L, Xue F et al. Impact of pupil diameter on axial growth in orthokeratology. Optom Vis Sci. 2012;89(11):1636-40. 15.Downie LE, Lowe R. Corneal Reshaping Influences Myopic Prescription Stability (CRIMPS): an analysis of the effect of or-thokeratology on childhood myopic refractive stability. Eye Contact Lens. 2013;39:303–10. 16.Faria-Ribeiro M, Navarro R, González-Méijome J, et al. Effect of Pupil Size on Wavefront Refraction during Orthokeratology. Optom Vis Sci. 2016; 93(11):1399-1408. 17.Faria-Ribeiro M, Queirós A, Lopes-Ferreira D, et al. Peripheral refraction and retinal contour in stable and progressive myopia. Optom and Vis Sci. 2013;90(1):9-15. 18.Marcotte-Collard R, Simard P, Michaud L. Analysis of two orthokeratology lens designs and comparison of their optical effects on the cornea. Eye Contact Lens.2018;44(5):322–9. 19.Carracedo G, Espinosa-Vidal TM, Martínez-Alberquilla I, Batres L. The Topographical Effect of Optical Zone Diameter in Or-thokeratology Contact Lenses in High Myopes. J Ophthalmol. 2019 Jan 2;2019:1082472. doi: 10.1155/2019/1082472.
|