J.ophthalmol.(Ukraine).2021;4:3-8.
|
http://doi.org/10.31288/oftalmolzh2021438 Received: 04 March 2021; Published on-line: 16 August 2021 Сhanges in bacterial keratitis grade 2 in patients with diabetes mellitus O.V. Zavoloka 1, P.A. Bezditko 1, M.A. Karliychuk 2 1 Kharkiv National Medical University; Kharkiv (Ukraine) 2 Bukovinian State Medical University; Chernivtsi (Ukraine) E-mail: Olesya_zavoloka@yahoo.com TO CITE THIS ARTICLE: Zavoloka OV, Besditko PA, Karliychuk MA. Сhanges in bacterial keratitis grade 2 in patients with diabetes mellitus. J.ophthalmol.(Ukraine). 2021;4:3-8. http://doi.org/10.31288/oftalmolzh2021438 Background: The pathological changes in the immune system and inflammatory response in diabetes mellitus (DM) result in impaired wound healing and the chronicity of the immune response. Purpose: To determine the features of the longitudinal changes in bacterial keratitis grade 2 in patients with type 1 DM. Material and Methods: We retrospectively reviewed the outcomes of treatment of 19 patients (19 eyes; main group) with both bacterial keratitis grade 2 and type 1 DM and 15 patients (15 eyes; control group) with bacterial keratitis grade 2 only. All patients received topical antibiotic, ofloxacin. In addition, they received topical antiseptics, antioxidants, repairing agents, hyaluronic acid-based artificial tears, and mydriatics and systemic anti-inflammatory agents. Observations were performed within 24 days after initiation of treatment. Patients had a routine eye examination, bacteriological studies, fluorescein dye test, anterior eye OCT and non-contact corneal esthesiometry. Results: Compared to the controls, patients of the main group showed increased corneal sensitivity within the study period, increased corneal infiltrate depth and corneal edema depth beginning from day 3, and increased severity of pericorneal injection and corneal ulcer depth beginning from day 7 (р < 0.05). In addition, corneal infiltrate resolved in all patients of the main group four days later and corneal edema, seven days later than in controls (р < 0.05). Most patients of the main group had a more severe outcome than did controls. Particularly, on day 24, an ulcer defect was still present in 33.3% of patients of the main group, with corneal haze, nubecula corneae and macula corneae seen in 44.4% and 22.2%, respectively, of patients of this group, versus 93.3% and 6.7%, respectively, for controls (р < 0.05). Conclusion: The features of the longitudinal changes in bacterial keratitis grade 2 in patients with DM cause prolongation of the course and worsening of outcomes of therapeutic treatment of bacterial keratitis grade 2. Keywords: diabetes mellitus, bacterial keratitis, severity of bacterial keratitis, longitudinal changes in bacterial keratitis
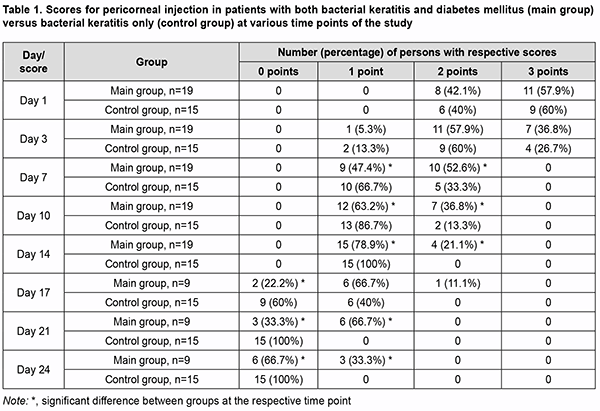
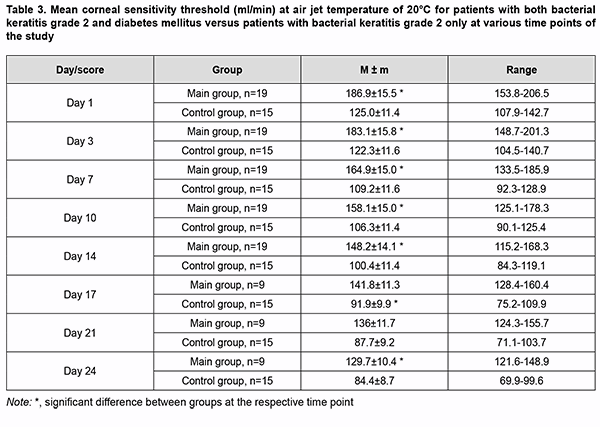
Introduction Bacterial keratitis is more common in diabetes mellitus (DM) than in general population [1]. The pathological changes in the immune system and inflammatory response in DM result in impaired wound healing and the chro-nicity of the immune response [2]. It is reasonable to assume that the longitudinal changes in bacterial keratitis in patients with DM are characterized by some features, but the literature is scarce on this subject. There is no general-ly accepted classification of keratitis with regard to severity, and none of the currently available classifications [3, 4] accounts for the neurotrophic condition of the cornea. That is why we developed a scheme for determining the severity of bacterial keratitis with consideration of the amount of reduction in corneal sensitivity which will be help-ful for improved characterization of the clinical condition of patients with DM, selection of adequate treatment, and determination of disease prognosis with greater accuracy. The purpose of this study was to determine the features of the longitudinal changes in bacterial keratitis grade 2 in patients with type 1DM. Material and Methods We reviewed the outcomes of therapeutic treatment of 19 patients (19 eyes; main group) with both bacterial keratitis grade 2 and type 1DM and 15 patients (15 eyes; control group) with bacterial keratitis grade 2 only in whom the pathogen was found to be sensitive to ofloxacin by a bacteriological study performed before administra-tion of treatment. Bacterial keratitis was diagnosed on the basis of typical clinical picture and the diagnosis was bacteriologically confirmed. The severity of keratitis was determined as per our scheme for the determination of severity of bacterial keratitis (a total score of 15 to 21 and no threat of loss of the eye). The scheme includes eight parameters, with each parameter scored from 0 to 3: lesion location (1: peripheral; 2: paracentral; 3: central); inflammatory response in the anterior eye (1:mild, 5 to 10 cells in the field of vision; 2:moderate, 10 to 50 cells in the field of vision; 3:severe, >50 cells in the field of vision, fibrin deposits, hypopion); pericorneal injection (1: mild; 2: moderate; 3: marked); size of ulcer defect (1: < 2 mm; 2: 2-5 mm; 3: >5 mm); OCT-measured depth of the corneal ulcer (1: < 1/3 of the corneal thickness; 2: 1/3-2/3 of the corneal thickness; 3: >2/3 of the corneal thickness); corneal infiltration (1: epithelial; 2: stromal; 3: diffuse); corneal edema (1: epithelial; 2: stromal; 3: diffuse); and reduction in corneal sensitivity threshold measured by non-contact air-jet corneal esthesiometer at an air jet temperature of 20 °С (1: mild, 80-130 mL/min; 2: moderate, 130-150 mL/min; 3: marked, >150 mL/min). A single pathogen was found in 17/19 eyes (89.5%) of the main group. Particularly, a Gram positive species was identified in 15 (88.2%) of the 17 eyes, with Staphylococcus epidermidis being the most common (9 eyes; 52.9%), followed by Staphylococcus aureus (3 eyes; 17.6%), Streptococcucus viridans (2 eyes; 11.8%), and Staphylococcus saprophyticus (1 eye; 5.9%). In addition, a Gram negative species was identified in 2 (11.8%) of the 17 eyes (Moraxella species, 1 (5.9%) and Esherichia coli, 1 (5.9%)). Moreover, mixed microflora (Staphylococcus aureus and Staphylococcus epidermidis) was evident in 2 (10.5%) of the 17 eyes. A single pathogen was found in 13/15 eyes (86.7%) of the control group. Particularly, a Gram positive species was identified in 7 eyes (46.7%), with Staphylococcus epidermidis being the most common (3 eyes; 20%), followed by Staphylococcus aureus (2 eyes; 13.3%), Streptococcucus viridans (1 eye; 6.7%), and Staphylococcus saprophyticus (1 eye; 6.7%). In addition, a Gram negative species was identified in 6 (40%) of the 15 eyes (Pseudomonas aeruginosa, 4 (26.7%), Moraxella species, 1 (6.7%) and Esherichia coli, 1 (6.7%)). Moreover, mixed microflora (Staphylococcus aureus and Staphylo-coccus epidermidis) was evident in 2 (13.3%) of the 15 eyes. All patients received topical ofloxacin before the bacteriological results confirming the absence of pathogens in corneal scrapings and smears were available. In addition, they received topical antiseptics, antioxidants, repairing agents, hyaluronic acid-based artificial tears (0.15-0.4% hyaluronic acid), and mydriatics and systemic anti-inflammatory agents. Observations were performed on day 1 and days 7, 14, 17, 21 and 24. At day 14, the treat-ment scheme for 10 patients of the main group was changed, and these patients were excluded from the study at days 17, 21 and 24. In the main group, patient age ranged from 18 to 48 years, with a mean age of 32.1±8.9 years. Of the 19 pa-tients of this group, 8 (42.1%) had a diabetes duration of 5 to 10 years, and 11 (57.9%) had a diabetes duration of more than 10 years. In addition, of the 19 patients, 6 (31.6%) had inadequately controlled diabetes (defined as he-moglobin A1c (HbA1c) level of 7.1-7.5%), and 13 (68.4 %) had out-of-control diabetes (defined as HbA1c ≥7.5%). Diabetic polyneuropathy (DPN) was found in all patients. Of the 19 patients, 10 (52.6%) had symptomatic DPN, and 9 (47.4%) had disabling DPN as per the classidication of Dyck (1999) [5]. In the control group, patient age ranged from 18 to 49 years (mean, 32.3±8.5 years), and there was no significant difference (р>0.05) in age between the groups. The study protocol was approved by the Bioethics Committee (Committee Minutes No. 11 dated 5.12.2018). The conduct of the study adhered to the Declaration of Helsinki. Patients had a routine eye examination (visual acuity, tonometry, and slit-lamp biomicroscopy of anterior and posterior eye segments), bacteriological studies, fluorescein dye test, anterior eye OCT (TOPCON 3D OCT-2000) and non-contact corneal esthesiometry (using the device and methods we developed [6]). Mean and standard deviation (SD) values as well as ranges for corneal sensitivity threshold were calculated. The Mann-Whitney rank test was used to compare the scores for patients of the main group to those for controls. The level of significance p ≤ 0.05 was assumed. Excel 2010 was used to develop the primary data base, and Stata 12 software (Stata Corp., College Station, TX) was used for statistical analyses. Results The most common lesion location was paracentral (63.2%), followed by central (26.3%), and peripheral (10.5%) for the main group versus paracentral (60%), followed by central (26.7%), and peripheral (10.5%) for the control group, and there was no significant difference (р>0.05) in lesion location between the groups. In the main group, pericorneal injection was marked (57.9%) or moderate (42.1%) at visit 1, and was more se-vere than in most patients of the control group beginning from day 7 (р<0.05). In addition, pericorneal injection was mild in 33.3% of patients of the main group at day 24, whereas all patients of the control group exhibited normal pale pink conjunctiva at day 21 (Table 1).
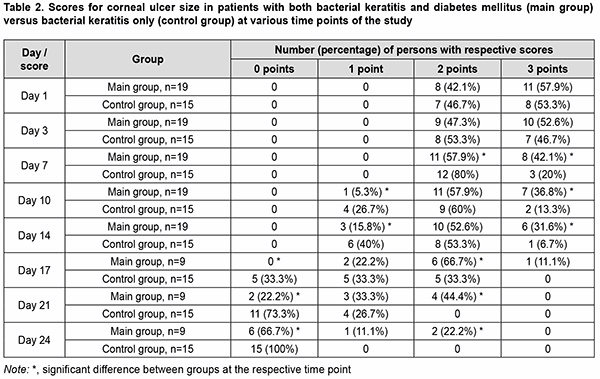
The size of ulcer was >5 mm in most (57.9%) and 2-5 mm in the rest (42.1%) patients, and OCT-measured depth of the corneal ulcer was 1/3-2/3 of the corneal thickness in most (52.6%) and < 1/3 of the corneal thickness in the rest (47.4%) patients of the main group at visit 1. Beginning from day 7, the ulcer was larger and its depth was greater in most patients of the main group than in patients of the control group (р<0.05). On day 24, an ulcer defect was still present in 33.3% of patients of the main group; the defect sized less 2 mm and was as deep as less than 1/3 of the corneal thickness in 11.1%, and sized 2-5 mm and was as deep as 1/3-2/3 of the corneal thickness in 22.2% of patients of the main group, whereas all patients of the control group exhibited corneal re-epithelialization (Table 2).
At visit 1, most patients of both groups showed stromal corneal infiltration. Beginning from day 3, most patients of the main group showed deeper corneal infiltration than patients of the control group (р<0.05). Corneal infiltra-tion resolved in all patients of the main group on day 21, four days later than in patients of the control group. At visit 1, edema of the corneal tissue surrounding the ulcer was diffuse, epithelial and stromal in 42.1%, 31.6% and 26.3%, respectively, of patients of the main group. Beginning from day 3, most patients of the main group showed deeper corneal edema than patients of the control group (р<0.05). Corneal edema resolved in all patients of the main group on day 24, seven days later than in patients of the control group. At visit 1, compared to controls, patients of the main group showed 59.5%, 53.8%, 49.5%, 46.2% and 44.4% higher mean corneal sensitivity threshold at air jet temperature of 5°С, 15°С, 20°С and 40°С, respectively. At all study time points, compared to controls, patients of the main group showed higher mean corneal sensitivity thresh-old at air jet temperature of 20°С. Particularly, compared to controls, it was 49.7% higher at day 3; 51% higher at day 7; 48.7% higher at day 10; 47.6% higher at day 14; 54.3% higher at day 17; 55.1% higher at day 21; and 53.7% higher at day 24 (Table 1). Reduction in corneal sensitivity threshold at air jet temperature of 20°С was marked in all patients of the main group at visit 1, and mild and moderate in 77.8% and 22.2%, respectively, of patients of the main group on day 24. At all study time points, most patients of the main group showed greater re-duction in corneal sensitivity threshold at air jet temperature of 20°С than did controls (р<0.05). At visit 1, mean corneal sensitivity threshold at air jet temperature of 20°С in the fellow eye was 35% higher in patients of the main group (81.2±5.4 ml/min; range, 73.7 to 89.3 ml/min) than in controls (60.0±9.1 ml/min; range, 44.2 to 70.1 ml/min) (р<0.05). The course of bacterial keratitis grade 2 was prolonged in all patients of either group. The outcome of therapeutic treatment depended on the presence DM, and most patients of the main group had a more severe outcome than did controls (р<0.05). Thus, on day 24, an ulcer defect was still present in 33.3% of patients of the main group; the defect sized less 2 mm and was as deep as less than 1/3 of the corneal thickness in 11.1%, and sized 2-5 mm and was as deep as 1/3-2/3 of the corneal thickness in 22.2% of patients of the main group. This is why these patients were recommended to undergo surgery, namely, curative keratoplasty. In addition, corneal healing was observed in 66.7% of patients of the main group, with corneal haze, nubecula corneae and macula corneae in 44.4% and 22.2%, respectively, of patients of this group. Moreover, corneal healing was ob-served in all controls, with corneal haze, nubecula corneae and macula corneae, in 93.3% and 6.7%, respectively, of patients of this group.
Discussion The current study found that DM contributes to prolongation of the course and worsening of treatment out-comes of bacterial keratitis grade 2. We believe that this might be associated with the pathological changes in in-flammation in patients with DM due to “metainflammation”, chronic low-grade metabolically-induced inflamma-tion [7, 8]. Chronic low-grade metabolically-induced inflammation in patients with DM results in expression of pro-inflammatory factors (IL-1α, IL-1β and IL-1 receptor antagonist) and changes in body response to damage [9]. We believe that the features of the longitudinal changes in bacterial keratitis grade 2 in patients with DM are also asso-ciated with the pathological changes in corneal nerve fibers resulting from diabetic neuropathy, because it is known that the neurotrophic condition of the cornea exerts an impact on corneal defect healing in patients with keratitis, determining disease severity, duration and treatment outcomes [1]. The features of the longitudinal changes in bac-terial keratitis grade 2 in patients with DM necessitate a comprehensive approach to treatment, taking into consid-eration all provoking factors. Conclusion The features of the longitudinal changes in bacterial keratitis grade 2 in patients with DM cause prolongation of the course and worsening of outcomes of therapeutic treatment of bacterial keratitis grade 2. On day 24, an ulcer defect was still present in 33.3% of patients with both bacterial keratitis grade 2 and DM, and corneal healing was observed in all patients with bacterial keratitis grade 2 only. The features of the longitudinal changes in bacterial keratitis grade 2 in patients with DM necessitate a comprehensive approach to treatment, taking into consideration all provoking factors.
References 1.Wang B, Yang S, Zhai H, Zhang Y, Cui C, Wang J, Xie L. A comparative study of risk factors for corneal infection in diabetic and non-diabetic patients. Int J Ophthalmol. 2018;11(1):43–7. 2.Peleg AY, Weerarathna T, McCarthy JS, Davis TM. Common infections in diabetes: pathogenesis, management and relationship to glycaemic control. Diabetes Metab Res Rev. 2007;23(1):3-13. 3.Vital MC, Belloso M, Prager TC, Lanier JD. Classifying the severity of corneal ulcers by using the "1, 2, 3" rule. Cornea. 2007;26(1):16-20. 4.Sitnik GV. [Current approaches to the treatment of corneal ulcers]. Meditsinskii Zhurnal. 2007;4:100-14. Russian. 5.Dyck PJ, Dyck PJB: Diabetic polyneuropathy: section III. In: Diabetic Neuropathy. 2nd ed. Dyck PJ, Thomas PK, Eds. Philadelph-ia: W.B. Saunders. 1999; p. 255–78. 6.Zavoloka OV, Bezditko PA, Lukhanin OO. Efficacy of a novel non-contact corneal esthesiometer in assessing the neurotrophic status of the cornea in type I diabetic patients with bacterial keratitis. J Ophthalmol (Ukraine). 2019;6:29-33. 7.Tsai S, Clemente-Casares X, Revelo XS, Winer S, Winer DA. Are obesity-related insulin resistance and type 2 diabetes autoim-mune diseases? Diabetes. 2015;64(6):1886-97. 8.Gregor MF, Hotamisligil GS. Inflammatory mechanisms in obesity. Annu Rev Immunol. 2011;29:415-45. 9.Esser N, Legrand-Poels S, Piette J, Scheen AJ, Paquot N. Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res Clin Pract. 2014;105(2):141-50. Conflict of Interest Statement: The authors declare no conflict of interest which could influence their opinions on the subject or the materials presented in the manuscript.
|