J.ophthalmol.(Ukraine).2021;2:64-68.
|
http://doi.org/10.31288/oftalmolzh202126468 Received: 10 December 2020; Published on-line: 19 April 2021 Ocular manifestations of trigeminal autonomic cephalgias: analysis of cases V. V. Biloshytsky, V. A. Vasyuta, Ophthalmologist, M. V. Biloshytska SI "Romodanov Neurosurgery Institute, National Academy of Medical Sciences of Ukraine"; Kyiv (Ukraine) E-mail: vasyuta.v@ukr.net TO CITE THIS ARTICLE:Biloshytsky VV, Vasyuta VA, Biloshytska M. Ocular manifestations of trigeminal autonomic cephalgias: analysis of cases. J.ophthalmol.(Ukraine).2021;2:64-68. http://doi.org/10.31288/oftalmolzh202126468 Trigeminal autonomic cephalgias (TACs) are the most common group of cephalgias with ocular symptoms and can be subdivided into cluster headache, paroxysmal hemicrania, short-lasting unilateral neuralgiform headache attacks and hemicrania continua. The diagnostic criterion at least one of the following autonomic symptoms or signs, ipsilateral to the headache: conjunctival injection and/or lacrimation; nasal congestion and/or rhinorrhoea; eyelid edema; forehead and facial sweating; forehead and facial flushing; sensation of fullness in the ear; and miosis and/or ptosis. Symptoms of sympathetic blockade (ptosis, myosis, Horner’s syndrome) may be present. Another characteristic that TACs share is periorbital or retroorbital location of headache pain. The cases of TACs reported demonstrate potential diagnostic pitfalls and patterns of ocular symptoms and treatment of these diseases. These patients not uncommonly present to ophthalmologists. Paying close attention to autonomic symptoms during history collection and meticulous elucidation of headache characteristics will facilitate a diagnosis and first-line treatment decisions. Keywords: cephalgia, diagnostic criteria, autonomic symptoms, ophthalmalgia
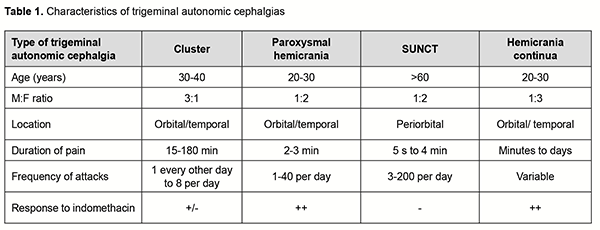
Introduction Headache of various etiologies is frequently accompanied by ocular impairments. Knowledge and an adequate assessment of the importance of major neuroophthalmic phenomena in different types of cephalgia can be helpful in the diagnosis and selection of adequate treatment strategy for this type of patients. Trigeminal autonomic cephalgias (TACs) are the most common group of cephalgias with ocular symptoms and can be subdivided into cluster headache, paroxysmal hemicrania, and short-lasting unilateral neuralgiform headache attacks and hemicrania continua. Short-lasting unilateral neuralgiform headache with conjunctival injection and tearing (SUNCT) and short-lasting unilateral neuralgiform headache attacks with cranial autonomic symptoms (SUNA) are considered to be rare primary headache disorders. Short lasting unilateral neuralgiform headache attacks can present either with conjunctival injection and tearing (SUNCT) or with cranial autonomic symptoms (SUNA). Trigeminal autonomic cephalgias are characterized by severe, strictly unilateral periorbital or retroorbital headache. Any trigeminal autonomic cephalgia has at least one of the following autonomic symptoms or signs, ipsilateral to the headache: conjunctival injection and/or lacrimation, nasal congestion and/or rhinorrhoea, eyelid edema, forehead and facial sweating, forehead and facial flushing, sensation of fullness in the ear, and miosis and/or ptosis. TACs subtypes differ in duration and frequency of the attacks, and some other clinical features. But what they primarily differ in is the response to treatment, which proves that they also differ in pathogenetic mechanisms and approaches to treatment (Table 1) [1].
A doctor dealing with patients with TACs may have two problems. On the one hand, the presence of ocular symptoms associated with headache may be helpful for differential diagnosis. However, in practice, a patient with TAC fails to report autonomic, particularly, ocular symptoms due to severity of pain, whereas his/her consulting doctor fails to ask relevant questions. As a result, the correct diagnosis is not made, and the patient does not receive appropriate treatment as per guidelines and protocols. On the other hand, given the severe pain in the ocular region (ophthalmalgia), the patient may consult an ophthalmologist for this symptom. However, in the period between attacks, an examination fails to reveal an eye disease. As a result, the patient also does not receive the correct diagnosis and appropriate treatment. The purpose was to study ocular manifestations of trigeminal autonomic cephalgias. Methods Cases with various types of trigeminal autonomic cephalgias were considered. Patients underwent a routine eye examination (visual acuity assessment, perimetry, biomicroscopy, and ophthalmoscopy), magnetic resonance imaging (MRI) and multislice computed tomography (MSCT) of the brain and neck, transcranial Doppler ultrasound, and Doppler neck ultrasound. In addition, visual analog scale (VAS) for pain was used. Results The cases of TACs given below demonstrate (a) the difficulties in diagnosis and (b) patterns of treatment of these diseases, and (c) characteristics of relevant ocular symptoms. Cluster headache The International classification of headache disorders, 3d edition (or ICHD-3), defines cluster headache as that characterized by attacks of severe, strictly unilateral pain which is orbital, supraorbital, temporal or in any combination of these sites, lasting 15-180 minutes and occurring from once every other day to eight times a day. The pain is associated with ipsilateral conjunctival injection, lacrimation, nasal congestion, rhinorrhoea, forehead and facial sweating, miosis, ptosis and/or eyelid oedema, and/or with restlessness or agitation [2]. Diagnostic criteria: A. At least five attacks fulfilling criteria B-D. B. Severe or very severe unilateral orbital, supraorbital and/or temporal pain lasting 15-180 minutes (when untreated). C. Either or both of the following: 1. at least one of the following symptoms or signs, ipsilateral to the headache: – conjunctival injection and/or lacrimation – nasal congestion and/or rhinorrhoea – eyelid oedema – forehead and facial sweating – miosis and/or ptosis 2. a sense of restlessness or agitation D. Occurring with a frequency between one every other day and 8 per day. E. Not better accounted for by another ICHD-3 diagnosis. Cluster headache presents in two distinct clinical forms: episodic and chronic. The most common is the episodic form which affects 85% of patients. In episodic cluster headache, attacks occur in series lasting for weeks or months (so-called cluster periods or bouts) separated by remission periods usually lasting months or years. In chronic cluster headache, attacks recur for > 1 year without remission periods or with remission periods lasting < 1 month. Cluster headache is an orphan condition with a prevalence of up to 0.1%. The classification does not specify some features of cluster headache like circadian pattern of attacks (cluster headache has been noted to occur with alarm clock periodicity at the exact same time of the day as well as seasonal recurrences). Cluster headache is typically seen in men, commonly among present of former smokers. Alcohol may significantly contribute to the severity of attacks. The pain of the cluster attack (as well as that of the trigeminal neuralgia attack) may be so severe that it has been called a "suicide headache" [3-5]. Sample case 1 A 28-year-old man presented to the Chronic Pain Department, Romodanov Neurosurgery Institute, with a chief complaint of attacks of severe pain in the right eye area and the retro-orbital region. The patient reported attacks lasting 1.5-2 hours approximately at the same time of the day (4 AM). At some days he had been experiencing another attack, less severe and lasting about 60 minutes, at about 7-8 PM. He described his pain as unbearable (rated 10 out of a possible 10 in intensity) and deep boring ache, but not pulsating and accompanied by no nausea. The patient also reported a history of periods of autumnal-and-wintry cephalgia one and three years before presentation; these periods were lasting one and a half months and one month, respectively. He said that his “current exacerbation” began a week before presentation. The man had seen ophthalmologists many times for his pain, but no eye disease had been found. At his most recent visit to an ophthalmologist, the latter suggested that patient’s pain had a neurological origin. A meticulous history collection confirmed that pain attacks were accompanied by right eye redness and lacrimation, and ipsilateral signs of lid hyperemia and swelling, and nasal congestion and rhinorrhoea. The patient also noted significant photophobia during attacks of pain. On examination he was found to be somatically and neurologically normal. He reported that he had been a smoker from the age of 15. Brain MRI and transcranial Doppler ultrasound (TDS) showed no pathological intracranial changes. Mild degenerative changes in the neck were found by neck MRI. TDS and Doppler neck ultrasound were within the normal range for patient’s age. On examination of the eye, visual acuity was 1.0 OU and IOP, 15 mmHg OD and 16 mmHg OS. No visual field changes were elicited. The conjunctiva was pale pink. The media were transparent and the fundus unremarkable. The patient was diagnosed with episodic cluster headache according to the ICHD-3 criteria and recommended to receive zolmitriptan 5 mg intranasally, followed by steroids in the form of bilateral greater occipital nerve block. This treatment resulted in remission of the condition. Paroxysmal hemicrania The diagnostic criteria according to the ICHD-3 are as follows: A. At least 20 attacks fulfilling criteria B-E. B. Severe unilateral orbital, supraorbital and/or temporal pain lasting 2-30 minutes. C. Either or both of the following: 1. at least one of the following symptoms or signs, ipsilateral to the headache: – conjunctival injection and/or lacrimation – nasal congestion and/or rhinorrhoea – eyelid oedema – forehead and facial sweating – miosis and/or ptosis 2. a sense of restlessness or agitation D. Occurring with a frequency of >5 per day E. Prevented absolutely by therapeutic doses of indomethacin F. Not better accounted for by another ICHD-3 diagnosis [2, 6, 7]. Sample case 2 A 41-year-old female patient, a nurse, presented to the Chronic Pain Department, Romodanov Neurosurgery Institute, with a chief complaint of attacks of severe headache (rated 6 to 9 or 10 out of a possible 10 in intensity) which had bothered her since early summer of 2015. The patient described this headache as boring, progressive, and radiating from the left superior-posterior neck to the left mandible, maxilla, eye, ear and half of the nose. This headache was accompanied by left eyelid swelling, eye lacrimation, nasal congestion and/or rhinorrhoea, and upper lid ptosis. She also complained of sweating of the left face during nocturnal attacks. The frequency was 5 to 13 attacks a day, each with a duration between 15 and 20 minutes at the beginning of the disease, and between 25 and 30 minutes at presentation. Physical examination findings included pain with palpation of the left greater and lesser occipital nerves. She had seen ophthalmologists many times, but no eye disease had been found during a period between attacks. On examination of the eye, uncorrected visual acuity (UCVA) was 0.7 OD and 0.6 OS, and best-corrected visual acuity (BCVA) was 1.0 OU with a spherical equivalent refraction of -0.75D. The media were transparent. The optic discs were pale pink, with well-defined margins, and no change in vessel caliber was present. The patient was diagnosed with mild myopia in both eyes. The neurological diagnosis was chronic paroxysmal hemicranias (ICHD-3). The patient was recommended to take indometacin chronically at a low dose (25 mg twice a day) for pain relief with minimal side effects on her digestive tract. Short-lasting unilateral neuralgiform headache attacks According to the ICHD-3, there are two types of short-lasting unilateral neuralgiform headache attacks: short-lasting unilateral neuralgiform headache with conjunctival injection and tearing (SUNCT) and short-lasting unilateral neuralgiform headache attacks with cranial autonomic symptoms (SUNA) [2, 8, 9]. Both SUNCT and SUNA share the diagnostic criteria as follows: A. At least 20 attacks fulfilling criteria B to D B. Moderate or severe unilateral head pain, with orbital, supraorbital, temporal and/or other trigeminal distribution, lasting for 1 to 600 seconds and occurring as single stabs, series of stabs or in a sawtooth pattern C. At least 1 of the following cranial autonomic symptoms or signs, ipsilateral to the pain: - conjunctival injection and/or lacrimation - nasal congestion and/or rhinorrhea - eyelid oedema - forehead and facial sweating - forehead and facial flushing - sensation of fullness in the ear - miosis and/or ptosis D. Attacks have a frequency of at least 1 a day for more than half of the time when the disorder is active E. Not better accounted for by another ICHD-3 diagnosis The diagnostic criteria of SUТCT are as follows: A. Attacks fulfilling criteria for 3.3 short-lasting unilateral neuralgiform headache attacks B. Both of conjunctival injection and lacrimation (tearing) [10]. Sample case 3 A 31-year-old man presented to the Chronic Pain Department, Romodanov Neurosurgery Institute, with a chief complaint of short-lasting attacks of severe pain in the right forehead, above the upper margin of the right eyelid. The patient described the pain attacks as electric-shock–like. The frequency of the attacks varied along the course of the disease, with a maximum of 50-300 attacks a day. Half of the attacks lasted 5–6 seconds, while the others, 1–2 seconds. Longer attacks were rated 8, and shorter attacks, 1-2 out of 10 on the VAS. A longer attack was with a time to peak pain severity 2-3 seconds, and of abrupt relief. Headaches were accompanied by lacrimation, and, if the time between attacks was as small 10 seconds, by redness of the conjunctiva of the right eye. Occasionally, attacks may be provoked by brisk movements, e.g., rising from the horizontal to the vertical position or bending forward, or by skin irritation of the right nasal dorsum. A series of attacks may be followed by a latency period of 15-20 minutes during which the above brisk movements do not provoke pain. Neuroimaging studies (MSCT with intravenous contrast and brain angiography, brain MRI with intravenous contrast) found a venous angioma in the right pons and right middle cerebellar peduncle, which was described as “an anomalous 22-mm-long venous vessel with a diameter of 2.6 mm or less”. Vascular neurosurgeons found no association between patient’s complaints and the vascular abnormality. The ophthalmologist concluded that the eye was normal. The patient was diagnosed with short-lasting unilateral neuralgiform headache with conjunctival injection and tearing according to the ICHD-3. SUNCT are successfully treated with anticonvulsants such as lamotrigine, topiramate, and gabapentin. Occipital nerve stimulation and electrical stimulation of deep brain structures (DBS of the ipsilateral posterior inferior hypothalamus) have been used in refractory SUNCT. Hemicrania continua Hemicrania continua is a relatively rare trigeminal autonomic cephalgia. The diagnostic criteria of hemicrania continua (ICHD-3) are as follows: A. Unilateral headache fulfilling criteria B-D B. Present for >3 months, with exacerbations of moderate or greater intensity C. Either or both of the following: 1. at least one of the following symptoms or signs, ipsilateral to the headache: – conjunctival injection and/or lacrimation – nasal congestion and/or rhinorrhoea – eyelid oedema – forehead and facial sweating – miosis and/or ptosis 2. a sense of restlessness or agitation, or aggravation of the pain by movement D. Responds absolutely to therapeutic doses of indomethacin Other common ocular features include foreign body sensation in the eye, eye itching and photofobia. Some patients have reported contact lens intolerance. A high dose of indomethacin (300 mg to 500 mg a day) may be required to produce treatment effect [11, 12]. Hemicrania continua is usually unremitting, but can occur in the remitting subtype where there are pain free periods lasting at least a day without treatment. Unremitting hemicrania continua are characterized by continuous pain for at least 1 year, without any symptom-free period. Sample case 4 A 56-year-old man presented to the Chronic Pain Department, Romodanov Neurosurgery Institute, with a chief complaint of his right face pain and right headache which had been present for the last four months. He described his pain as continuous with variable intensity and rated the maximum intensity of pain as intolerable (VAS 10/10). Exacerbations radiated from the right nasal dorsum to the glabellar, right superciliary region, and frontal and temporal areas. Because the patient was taking non-steroidal anti-inflammatory agents (like Nimesulid and/or Ketorolac) to relieve pain, he could not accurately define duration of pain exacerbation periods. Headache exacerbations were associated with swollen right superior face and eyelids, incomplete right eye closure (not because of ptosis, but rather because of edema), scleral redness and tearing on the right side. On examination there was severe soft tissue edema in the right periorbital region and right superior cheek. Physical examination findings included pain with palpation of the right occipital area, 1-1.5 cm to the right of and 1.5 cm below the protuberantia occipitalis externa. The neurological status was unremarkable. Brain MRI was normal. On examination of the eye, visual acuity was 1.0 OU. There was mild right lid edema, grade 1 ptosis. The conjunctiva was pale pink and the cornea transparent. There was mild miosis, and the pupil light response was preserved. The optic discs were pale pink, with well-defined margins, and there was no change in vessel caliber or macular region. The initial provisional diagnosis was hemicrania continua (ICHD-3). Indomethacin was administered and followed by a right occipital nerve block. The patient improved with the treatment. Discussion All patients with various types of trigeminal autonomic cephalgia exhibited ocular manifestations which required a meticulous differential diagnosis. Conjunctival injection, lacrimation, lid edema and ptosis should be considered as autonomic symptoms [2, 8, 9]. The management of these disorders requires meticulous history collection, determination of chief complaints, and eye examination. If the eye examination is normal, the patient should be referred to the neurologist to rule out various types of cephalgia. Therefore, trigeminal autonomic cephalgias are a heterogeneous group of diseases sharing several characteristics including periorbital or retroorbital location of headache pain and autonomic ocular symptoms resulting from parasympathetic activation (conjunctival injection and tearing) or sympathetic blockade (ptosis, myosis, Horner’s syndrome). These patients not uncommonly present to ophthalmologists. Paying close attention to autonomic symptoms during history collection and meticulous elucidation of headache characteristics will facilitate a diagnosis and first-line treatment decisions. Establishing centers and/or emergency rooms for headache problems in Ukraine based on the experience of the developed countries would be reasonable. The work of such services will require a multidisciplinary approach to the diagnosis and management of persons with headache, with contributions from several medical and surgical specialties like ophthalmology, neurology and neurosurgery.
References 1.Dafer MR, Jay WM. Headache and the eye. Curr Opin Ophthalmol. 2009 Nov;20(6):520-4. 2.International Classification of Headache Disorders. 2nd edition. Cephalalgia 2004;24 (Suppl):9-160. 3.Hoffmann J, May A. Diagnosis, pathophysiology, and management of cluster headache. Lancet Neurol. 2018;17(1):75-83. 4.Ljubisavljevic S, Zidverc Trajkovic J. Cluster headache: pathophysiology, diagnosis and treatment. J Neurol. 2019;266(5):1059-66. 5.Matharu M, Goadsby P: Cluster headache—update on a common neurological problem. Pract Neurol. 2001;1:42–9. 6.Goadsby PJ, Cittadini E, Cohen AS. Trigeminal autonomic cephalalgias: paroxysmal hemicrania, SUNCT/SUNA, and hemicrania continua. Semin Neurol. 2010;30(2):186-91. 7.Prakash S, Patell R. Paroxysmal hemicrania: an update. Curr Pain Headache Rep. 2014 Apr;18(4):407. 8.Lambru G, Matharu MS. SUNCT, SUNA and trigeminal neuralgia: different disorders or variants of the same disorder? Curr Opin Neurol. 2014;27(3):325-31. 9.Pomeroy JL, Nahas SJ. SUNCT/SUNA: A Review. Curr Pain Headache Rep. 2015;19(8):38. 10.Williams M.H., Broadley S.A., SUNCT and SUNA: clinical features and medical treatment. J Clin Neurosci. 2008; 15:526-34. 11.Pareja JA, Antonaci F, Vincent M. The hemicrania continua diagnosis. Cephalalgia. 2001;21(10):940-6. 12.Vincent MB. Hemicrania continua. Unquestionably a trigeminal autonomic cephalalgia. Headache. 2013;53(5):863‐868. The authors declare no conflict of interest which could influence their opinions on the subject or the materials presented in the manuscript.
|