J.ophthalmol.(Ukraine).2021;1:3-9.
|
http://doi.org/10.31288/oftalmolzh2021139 Received: 09 April 2020; Published on-line: 12 February 2021 Impact of corneal astigmatism on refractive outcomes after phacoemulsification with implantation of a spherical IOL N. G. Zavgorodnia, V. Iu. Novikova Zaporizhzhia State Medical University;Zaporizhzhia (Ukraine) VISUS clinic; Zaporizhzhia (Ukraine) E-mail: n.valeriya86@gmail.com TO CITE THIS ARTICLE: Zavgorodnia NG, Novikova VIu. Impact of corneal astigmatism on refractive outcomes after phacoemulsification with implantation of a spherical IOL. J.ophthalmol.(Ukraine).2021;1:3-9. http://doi.org/10.31288/oftalmolzh2021139 Background: To date, particular emphasis is being put to correction of preoperative corneal astigmatism in phacoemulsification, since approximately 30% of the world’s population has astigmatism of at least 0.75D which results in decreased visual acuity after cataract surgery. Purpose: To assess the effect of corneal astigmatism on refractive outcomes of phacoemulsification with implantation of a spheric intraocular lens (IOL). Material and Methods: We retrospectively analyzed the outpatient medical records of 39 patients (50 eyes) who received phacoemulsification with a spherical IOL and had corneal astigmatism of 0.5-3.75D (as assessed by keratometry). Eyes were divided into four groups based on the degree of corneal astigmatism. We assessed changes in visual acuity and corneal astigmatism and refractive outcomes of cylindrical correction at one month after surgery. Results: The greater the presurgical astigmatism, the lower was uncorrected visual acuity at one month after surgery. There was no significant difference (р > 0.05) in change in corneal astigmatism values after phacoemulsification. In group 1 (preoperative astigmatism of 0.75 D or less) and group 2 (preoperative astigmatism of 1.0 to 1.5 D), the mean increase in visual acuity after cylindrical refractive correction was 10% or less, and had no significant impact on the quality of vision. In group 3 (preoperative astigmatism of 1.75 to 2.5 D) and group 4 (preoperative astigmatism of 2.75 D or more), the mean increase in visual acuity was 15% and 25%, respectively. Conclusion: Surgically induced astigmatism after phacoemulsification had no substantial impact on refractive outcomes. When planning refractive outcomes for eyes with astigmatism after cataract surgery, it should be taken into account that implanting a spherical IOL is acceptable only for eyes with an amount of preoperative astigmatism of 0.75 D or less and vertical axis of astigmatism. Cataract patients with preoperative corneal astigmatism of >0.75 D will require implantation of a toric IOL or a plan for astigmatism correction with another method. Keywords: cataract, corneal astigmatism, phacoemulsification
Introduction Cataract phacoemulsification has become the gold standard and the most common type of cataract surgery which produces rather fast, well-predictable and accurate refractive outcomes [1]. A cataract surgeon should aim to achieve a less than or equal to 0.5D difference between target and actual refraction after phacoemulsification and intraocular lens implantation [2], taking into account the spherical component and astigmatism. Studies have demonstrated that inadequate vision in the presence of astigmatism can result in reduced quality of life and an increased incidence of trauma. In addition, even mild astigmatism is accompanied by a decrease both in visual acuity and capacity to perform daily tasks requiring discrimination (e.g., driving a car). Astigmatism axis orientation beyond the horizontal meridian substantially impedes reading rate [3-5]. Patients with a high degree of astigmatism who had cataract surgery with spherical intraocular lens (IOL) placement are often dissatisfied with treatment outcomes because their uncorrected distance visual acuity remains rather poor due to astigmatism [6, 7]. Approximately 30 percent of the world’s population has astigmatism of at least 0.75D which results in decreased visual acuity after surgery [8]. Therefore, particular emphasis is being put to preoperative corneal astigmatism, and a variety of approaches (such as selecting tunnel incision location and width; use of corneal or limbal relaxing incisions; use of the opposite tunnel incision; and toric IOLs) have been proposed for its correction [6]. Surgically induced astigmatism is being discussed in the literature, may be severe and depends not only on incision size, but also on major anatomic and functional characteristics of the eye, including preoperative corneal astigmatism, anteroposterior length of the eye, and corneal rigidity and thickness [9, 10, 11, 12]. Although to date ophthalmic surgeons prefer implanting toric IOLs and there have been attempts at improving the design both of these IOLs themselves and their haptics, the problem of their postoperative rotation has not been solved completely [13]. Postoperative rotation of a toric IOL is accompanied by a significant decrease in visual acuity and deterioration of quality of vision, which significantly restricts their wide application in the clinical practice. It is still being discussed whether it is reasonable to implant spherical IOLs in eyes with corneal astigmatism, but the impact of preoperative parameters (such as degree and axis of preoperative astigmatism) on refractive outcome, quality of vision and requirement for additional correction after surgery is yet to be established. The purpose of the study was to assess the effect of corneal astigmatism on refractive outcomes of phacoemulsification with implantation of a spheric IOL. Material and Methods This paper presents the results of a retrospective study at the VISUS clinic, the clinical setting of the Department of Ophthalmology at the Zaporizhzhia State Medical University. We retrospectively analyzed the outpatient medical records of 39 patients (50 eyes) who received phacoemulsification with a spherical IOL and had corneal astigmatism of 0.5-3.75D (as assessed by keratometry). Patient age varied from 30 to 83 years (mean age, 62 ± 1.89 years). The numbers of male and female patients were approximately equal (24 (48%) and 26 (52%)). Each study eye received a spherical IOL which was usually selected by the patient. Of the 50 implanted IOLs, 38 were monofocal, 9, multifocal, and 3, trifocal. The surgical procedures were performed by three surgeons with an induced astigmatism of ≤ 0.25 D. A tunnel incision was made at 160°–180°. No complications were observed during or after surgery. Follow-up duration was 1 month. Eyes were divided into four groups based on the degree of corneal astigmatism: group 1, astigmatism of not more than ± 0.75 D (13 eyes, 26%), group 2, astigmatism of ±1.0 to ±1.5 D (13 eyes, 26%), group 3, astigmatism of ± 1.75 to ± 2.5D (12 eyes, 24%), and group 4, astigmatism of ± 2.75D and more (12 eyes, 24%). An eye examination included visual acuity assessment, automated refraction with auto-ref/keratometer (Unicos URK-700, Korea), biomicroscopy, direct ophthalmoscopy, tonometry, perimetry, ultrasound A-scanning (Pacscan Series 300А; Sonomed, USA), endothelial microscopy (SP-3000P, Topcon Corporation, Tokyo, Japan), and optical biometry and IOL calculation (IOL Master 700 - Carl Zeiss Meditec AG, Jena, Germany). Of the 50 eyes, 35 (70%) had immature cataract; 2 (4%), mild cataract; 8 (16%), mature cataract; 1 (2) overmature cataract, and 4 (8%) underwent refractive cataract surgery due to hyperopia and presbyopia. Statistical analyses were conducted using Statistica 13.0 (StatSoft, Tulsa, OK, USA) software (License No. JPZ8041382130ARCN10-J). The level of significance p < 0.05 was assumed. Data are presented as mean (M) and standard error of mean (m). Shapiro–Wilk W test was used to test normality. Student t test was used for paired series if the data fit for normal distribution. Non-parametric Mann-Whitney test was used if variables were not normally distributed. Results We aimed to assess the results of phacoemulsification with implantation of spherical IOLs in eyes with various degrees of preoperative astigmatism, and the first thing we were interested in was the impact of induced astigmatism on refractive outcome. Table 1 presents corneal astigmatism values for eyes with various degrees of presurgical astigmatism before and 1 month after surgery. There was no significant difference in change in corneal astigmatism values after phacoemulsification. The mean increase in astigmatism magnitude varied from ± 0.01 D to ± 0.13 D. The most substantial increase in astigmatism magnitude (with presurgical astigmatism of 1.75D-2.5D), by 6.5%, was observed for eyes from group 3, but the difference for this group and any other group was not significant.
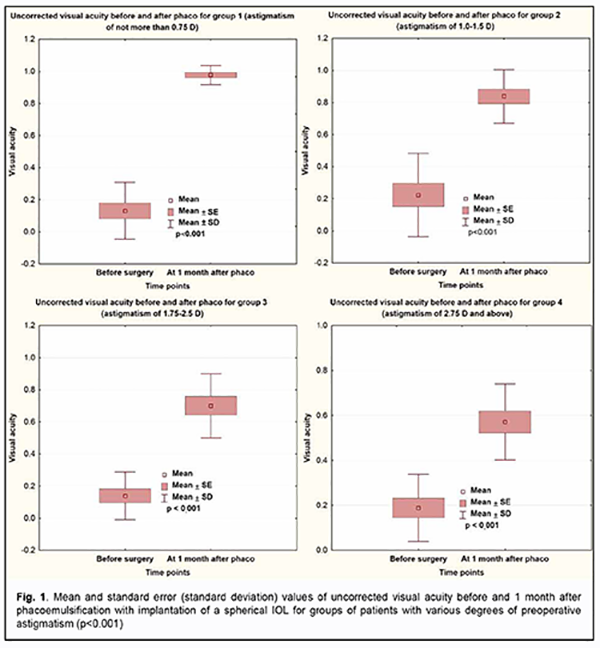
Visual acuity was the main efficacy measure and improved significantly in all groups. Fig. 1 presents uncorrected visual acuity (UCVA) values before and 1 month after surgery, and increases in UCVA for eyes with various degrees of preoperative astigmatism. One month after surgery, uncorrected visual acuity values increased significantly from 0.13 ± 0.04 to 0.89 ± 0.05 for group 1; from 0.22 ± 0.07 to 0.83 ± 0.04 for group 2; from 0.13 ± 0.04 to 0.7 ± 0.05 for group 3; and, somewhat less, from 0.18 ± 0.04 to 0.57 ± 0.04 for group 4 (with astigmatism of ± 2.75D and more). The results were statistically significant (p < 0.001) for all groups. The greater the presurgical astigmatism, the lower was uncorrected visual acuity.
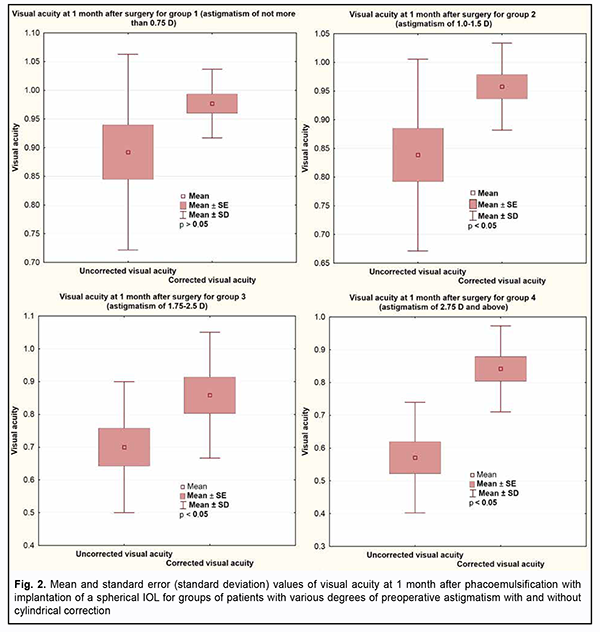
Fig. 2 presents best-corrected visual acuity (BCVA) values for eyes of the study. In groups 1 and 2 with preoperative astigmatism of 1.5 D or less, the mean increase in visual acuity after cylindrical correction was 10% or less, and had no significant impact on the quality of vision. In group 3 and group 4, cylindrical correction improved visual acuity by 15% and 25%, respectively.
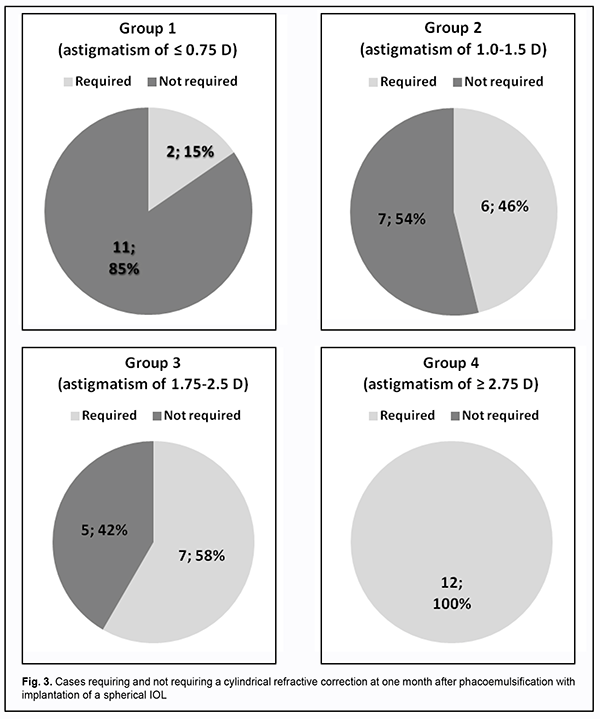
It is known that patients with astigmatism (especially, those with mild astigmatism) sometimes do not use refractive correction due to adequate adaptation of their visual and nervous systems. That is why clarification was sought as to whether this adaptation would still be preserved after phacoemulsification with a spherical IOL implantation. Because the impact of visual acuity on patient’s quality of life commonly depends on a number of sociological factors (such as occupation, habits and way of life), we performed an analysis of the cases requiring a cylindrical refractive correction after surgery (Fig. 3). Postoperative cylindrical correction was used in 2/13 eyes (15%) from group 1 (postoperative astigmatism of not more than ± 0.75 D), 6/13 eyes (46%) from group 2, 7/12 eyes (58%) from group 3, and all eyes from group 4 (postoperative astigmatism of more than ± 2.75 D).
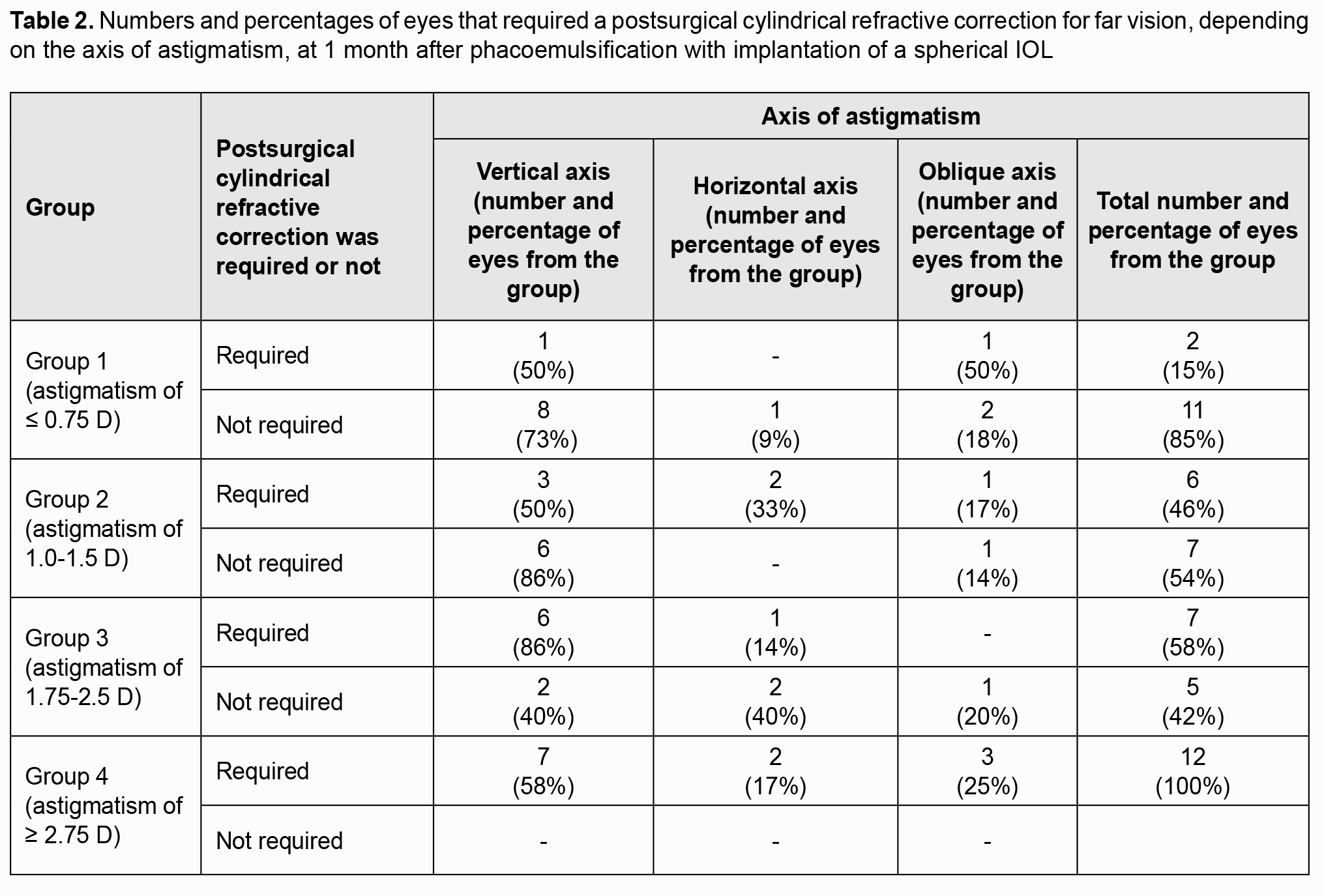
The axis of astigmatism was also important for subjective adaptation of the operated-on eye. Table 2 presents the numbers and percentages of eyes that required a postsurgical cylindrical correction, depending on the axis of astigmatism. It is worthy of note that, among patients from groups 1 to 3, those with a vertical (or close to vertical) axis of astigmatism felt themselves more comfortable and did not need postsurgical cylindrical correction. Thus, among the eyes from groups 1, 2 and 3 that did not need postsurgical cylindrical correction, 8 (73%), 6 (85%) and 2 (40%), respectively had a vertical axis of astigmatism.
Discussion Our findings on refractive outcomes of phacoemulsification with implantation of a spheric IOL in eyes with various degrees of preoperative astigmatism demonstrate a need for a differential approach in selecting the correction for astigmatism. Thus, we found that implanting a spherical IOL can be reasonable in preoperative astigmatism of not more than ±0.75 D, especially in eyes with a vertical (or close to vertical) axis of astigmatism. In these patients, visual acuity without correction was 0.89±0.05, and with a cylindrical correction, 0.97±0.06. The difference, however, was not significant, and such refractive outcome was not perceived by patients as a substantial improvement in visual acuity. Because approximately half (46%-58%) of patients with postoperative refractive astigmatism of 0.75 D to 2.75 D and all patients with postoperative refractive astigmatism of more than 2.75 D will require a cylindrical correction, the patient should be notified about this requirement in advance, and have a discussion about the method of subsequent correction of astigmatism. Studies by Kolomiets, Dmitriev and Lazar demonstrated [9, 10] that an amount of surgically induced astigmatism may vary within a wide range and depend not only on incision size, but also on major anatomic and functional characteristics of the eye, including preoperative corneal astigmatism, anteroposterior length of the eye, and corneal rigidity and thickness. Novytskyi [11, 12] found that the development of postoperative corneal astigmatism is mostly impacted by tunnel incision type and width and preoperative corneal astigmatism and less impacted by corneal diameter, intraocular pressure and axial length of the eye. In the current study, we found that surgically induced astigmatism had no substantial impact on refractive outcomes, since a change in amount of astigmatism following surgery was of 0.8% to 6.5%. Therefore, the results of this study demonstrate a need for a differential approach in considering the need for spherical IOL correction of astigmatism and allow us to conclude the following. First, surgically induced astigmatism following phacoemulsification had no substantial impact on refractive outcomes in eyes with preoperative astigmatism, since a change in the amount of astigmatism was less than 0.13 D with conventionally located tunnel incisions and ports. Second, when planning refractive outcomes for eyes with astigmatism after cataract surgery, it should be taken into account that implanting a spherical IOL is acceptable only for eyes with an amount of preoperative astigmatism of 0.75 D or less and vertical (or close to vertical) axis of astigmatism. Finally, cataract patients with preoperative corneal astigmatism of >0.75 D require implantation of a toric IOL or a plan for astigmatism correction with another method.
References 1.Leaming D. Practice styles and preferences of ASCRS members —2003 survey. J Cataract Refract Surg. 2004 Apr;30(4):892-900. 2.Wallace RB. Refractive cataract surgery and multifocal lOLs. Thorofare, NJ: SLACK Incorporated. 2000. 3.Vitale S. Prevalence of refractive error in the United States, 1999-2004. Arch Ophthalmol. 2008 Aug;126(8):1111-9. 4.Maliugin BE, Filippov VO. [Our first experience of correcting corneal astigmatism during phacoemulsification using a spherocylindrical IOL]. Novoe v oftal'mologii. 2001;1:15–6. Russian. 5.Black A, Wood J. Vision and falls. Clin Exp Optom. 2005 Jul;88(4):212-22. 6.Melnyk VO. [Experience of implanting an AcrySoft IQ Toric IOL during phacoemulsification in eyes with a high degree of astigmatism]. Proceedings of the Filatov Memorial Lectures conference with international speakers. 24-25 May; Odessa; 2012. p. 74. Ukrainian. 7.Bachuk N Yu. [Experience of implanting a toric intraocular lens in cataract patients with corneal astigmatism]. Mezhdunarodnyi medicinskii zhurnal. 2013;1:112–7. Russian. 8.Khripun КV. [Surgical correction of astigmatism during and after cataract extraction]. Cand Sc (Med) Thesis. St Petersburg, 2016. Russian. 9.Kolomiets VA, Dmytriiev SK, Lazar YuM. [Features of surgically induced astigmatism after phacoemulsification of age-related cataract with IOL implantation]. Oftalmol Zh. 2012;2:5-9. 10.Kolomiets VA, Dmitriev SK, Lazar YuM. [Surgically-induced astigmatism values after phacoemulsification in eyes with different IOP levels and corneal rigidity]. Oftalmol Zh. 2012;6:14-20. Russian. 11.Novytskyi О. [Clinical study of the potential for developing postoperative corneal astigmatism after cataract extraction with tunnel incision]. Cand Sc (Med) Thesis. Kyiv: NMAPO; 2002. Ukrainian. 12.Tyazhev МYu, Shanturova MA, Yur'eva TN, Antipin AG. [Traditional keratotomy and femtolaser arcuate corneal incisions for correcting astigmatism during phacoemulsification]. Sovremennye tekhnologii v oftal'mologii. 2017;6:119-121. Russian. 13.Fediashev GA, Egorov VV, Egorova AV. [Evaluating rotational stability of an AcrySoft IQ Toric IOL after senile cataract phacoemulsification]. Proceedings of the Modern Technologies in Cataract and Refractive Surgery conference with international speakers. Moscow; 2011. p. 210-2. Russian.
The authors declare no conflict of interest which could influence their opinions on the subject or the materials presented in the manuscript.
|