J.ophthalmol.(Ukraine).2020;6:70-73.
|
http://doi.org/10.31288/oftalmolzh202067073 Received: 28 August 2020; Published on-line: 21 December 2020 Strabismic amblyopia regression post refractive surgery Dr. Leopoldo Garduño Vieyra, Dr. Raúl Rúa Martínez, Dr. Raúl Macedo Cué Clínica Oftalmología Garduño,Guanajuato (Mexico) E-mail: ruamartinez@yahoo.es TO CITE THIS ARTICLE: Leopoldo Garduño Vieyra, Raúl Rúa Martínez, Raúl Macedo Cué. Strabismic amblyopia regression post refractive surgery. J.ophthalmol.(Ukraine).2020;6:70-3. http://doi.org/10.31288/oftalmolzh202067073 Background. Refractive laser surgery has absolute and relative contraindications. Among the relative ones is amblyopia and a history of strabismus. Caution should also be in cause of trauma, scar, or leukoma in the ablation site. Purpose. To present a case with regression of strabismic amblyopia after refractive surgery. Material and Methods. It was a pre-existing strabismus, which initially went unnoticed because it was a microtropia on left eye; the fixing right eye suffered a traumatic injury that produced a high ametropia and changed fixation. Results. The left eye developed excellent vision, but after the operation, somehow, momentarily the right eye became the fixator again, and the left eye saw very poorly. That situation was corrected quickly with right eye occlusion and lenses. That has happened because the eye had corrected its amblyopia for the years that the right eye was penalized. Once a good result was achieved, there was no change in fixation or visual loss. Conclusion. The change in ocular dominance and visual readjustment at the neuronal level that occurs in the postoperative period of refractive surgery stand out. Key words: refractive surgery, strabismus, amblyopia, ocular dominance, ocular trauma
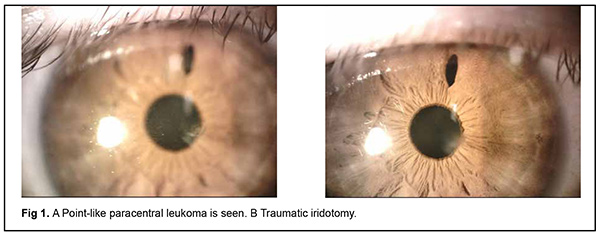
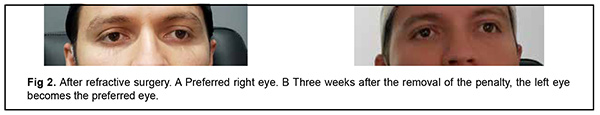
Introduction Amblyopia consists of a decrease in visual acuity in one or both eyes and occurs in the child's visual development period from birth to approximately 8 years of age. This decrease in visual acuity may be accompanied by other visual disturbances such as decreased contrast sensitivity, spatial distortion, and decreased or absent stereopsis [1]. There are several classifications of amblyopia considering numerous factors. Among them, the following stand out according to, visual acuity in each eye, the difference in visual acuity between both eyes, the type of fixation and the etiology. Within functional amblyopia, strabismic amblyopia is included, which if not detected in time leads to severe limitations of visual acuity in the future of the child. In these patients, a deviating eye image suppression mechanism occurs because each eye forms a different image. The eye where the suppression occurs will be the amblyopic eye [1, 2]. Generally, penalization of the eye with better vision is indicated, in this way the functioning of the amblyopic eye is stimulated. There are several types of penalization, pharmacological, refractive, occlusions with patches and filters, among others [2]. In the refractive penalty, inadequate refraction is induced in the dominant eye and an exact refraction in the amblyopic eye. Refractive laser surgery has absolute and relative contraindications. Among the relative ones is amblyopia and a history of strabismus. Caution should also be exercised when there is trauma, scar, or leukoma in the ablation site [3]. These features are present in the case described below. Case report A 22-year-old male patient who came to the clinic due to progressive decrease in visual acuity in the left eye of one month of evolution. As an important antecedent, the patient referred a penetrating corneal trauma to the right eye at age of 9, and photorefractive surgery (PRK) of 3 months of evolution. The ophthalmological examination revealed a preoperative visual acuity of the right eye of 20/400 that improved to 20/30 with RX correction 0.00 -4.00 x 30º. Slit lamp exam detected the presence of punctate paracentral leukoma, suggestive of an old penetrating wound, up to the endothelium, a wide anterior chamber, a reflective pupil, and the presence of traumatic iridotomy in the radius of 2. No lens injury was observed, and the fundus was normal. The preoperative visual acuity of the left eye of 20/60 that improves to 20/15 with correction RX -1.00 -2.00 x 180º. Transparent cornea, wide anterior chamber, reflective pupil, transparent lens, and fundus without alterations. The strabological examination was performed preoperatively and was found within normal limits. In this examination, no deviation of the left eye was detected as this was the fixing eye. The stereopsy test was not performed as there was no alteration in the strabological examination. One week after surgery, PRK presented visual acuity of the right eye of 20/40 and the left eye of 20/25. Then three weeks after PRK the visual acuity of the right eye was 20/30 and the left eye was 20/15. Three months after surgery, the visual acuity of the right eye was 20/30 with refraction of +0.50 –0.50 x 180º, cornea with paracentral leukoma from old trauma reduced in diameter and clearer that does not involve the optic center. In the left eye of 20/100 with refraction of +0.50 with -0.75 x 0º. The rest of the eye exam in both eyes was normal. When refraction under cycloplegia was performed, it was found in the right eye +1.00 -1.00 x 180º that did not improve and the left eye +1.00 -1.25 x 0º that did not improve. Strabological examination was performed and exotropia of the left eye of 3 prismatic diopters was detected, that is why it was decided to penalize the right eye for 24 hours. At the revision of the visual acuity of the left eye 24 hours later, the right eye being penalized, the visual acuity of the left eye improved to 20/15. The right eye patch was removed, and visual acuity was 20/30. The exotropia of the left eye persisted again after 3 PD. Steriopsis test was performed and it was detected that the patient did not have it. This explains that the patient has a deep left eye amblyopia, with a significant improvement before refractive surgery as the right eye was penalized by a corneal trauma causing an irregular astigmatism of four diopters. Three weeks after the removal of the penalty, the left eye becomes the preferred eye, as it is the one with the best visual acuity (20/15) and is able to see far and near vision well. The 3 prismatic diopter exotropia persists but is now noticeable in the right eye and the patient has alternating vision and no fusion. Discussion Small angle strabismus, such as microtropia, often go unnoticed. If it is not detected and corrected in time, it may be sufficient cause to develop amblyopia and need occlusive therapy [4]. This patient had a pre-existing microtropia and was monocular. The fixating eye was the right, so it never had stereopsis, and the left eye had some degree of amblyopia. When the patient suffered trauma to the right eye, the elevated astigmatism that occurred acted as a method of penalty in that eye, and the left eye took fixation permanently. Due to the trauma self-induced occlusion therapy in the right eye, the left eye developed excellent visual ability, 20/15 with low refractive error. Many investigators have determined the efficacy and safety of PRK refractive surgery in patients with accommodative and non-accommodative strabismus [5]. Kirwan et al [6] report in their study that no patient had strabismus decompensation and the majority improved their visual acuity. This justifies the performance of refractive surgery in strabic patients, but the patient must be individualized and studied very well, and their visual prognosis explained. In this patient, after refractive surgery, a good result was obtained in that a low refractive error remained, similar in both eyes, and initially both eyes saw acceptably well. But in the short term, the right eye resumed fixation (due to loss of self-induced suppression), and the left eye showed significant visual loss, even with cycloplegic refraction it did not improve. Gómez [7] and co-authors report that there are several factors that can influence the decompensation of a strabismus or the appearance of diplopia after refractive surgery. In his study, Gómez identifies residual accommodative factor, hypermetropic refractive hypercorrection, visual instability, decompensation of a phory, loss of suppression, change in dominance and presbyopia. It is common for several of these factors to occur simultaneously in the same patient. For this reason, it was decided to patch the right eye to see if the left eye improved, and so it happened, it improved until 20/15, and it no longer deteriorated again, achieving an uncorrected acuity of 20/15, the right eye remained in 20/30 and no further improvement with symmetrical low refractive errors in both eyes of around +1.00 with -1.00. Anisometropia is a major cause of loss of binocularity. Feng8 reports that patients with myopic anisometropia corrected with refractive surgery had abnormal ocular sensory dominance. Situation that improved after weeks of refractive adaptation. This study demonstrated that refractive adaptation plays a critical role in restoring sensory ocular balance in these operated patients. This effect of correction of ocular dominance does not occur immediately after surgery, it takes at least 16 weeks to be effective. Once that time has passed, in patients in whom the ocular imbalance persists, it is explained that it is more related to neural changes in ocular dominance than to residual refractive errors or those induced by the surgery performed, especially in high order aberrations [8]. Pseudovs comments in his study that patients who underwent refractive surgery in the first 10 weeks improve their vision due to a neuronal readjustment rather than the refractive change induced by the surgery [9]. In these patients with imbalance in ocular dominance, after 16 weeks of refractive adaptation, it is suggested to perform binocular therapies such as those described in the protocols for the correction of amblyopia in adults. Conclusion What is interesting about this case is that there was a pre-existing strabismus, which initially went unnoticed because it was a microtropia, the fixing eye suffered an injury that produced a high ametropia and the fixation changed, the left eye developed excellent vision, but after surgery, somehow, momentarily, the right one returned to be the fixator (because that is how the patient must have been originally before his accident), and the left saw very badly, which was quickly corrected with occlusion of the right eye and lenses since the eye had His amblyopia was corrected for the years that the right eye was penalized, and once a good result was achieved, there was no change in fixation or visual loss. The patient is stable, sees well, is satisfied, and will surely remain that way. For this reason, it is vitally important to perform a binocularity or stereopsy test as a routine test in the preoperative of refractive surgery. Even in patients who are in orthotropia, it must be done.
Bibliography 1.Melero Sánchez R. Ambliopía. [Master's Thesis]. España: Escuela de Formación Superior SAERA; 2017. Available in: http://www.saera.eu/wp-content/uploads/2017/09/Ambliopia_RosaMariaMelero... 2.Ugarte Gutiérrez JC. Efectividad de la penalización farmacológica con atropina y parche ocular en el tratamiento de la ambliopía, hospital regional de tumbes II - 2, durante el periodo de enero 2018 a diciembre del 2018. [Undergraduate Thesis]. Perú: Universidad Privada Antenor Orrego; 2019. Available in: http://repositorio.upao.edu.pe/handle/upaorep/5461 3.Miranda Hernández I, Barroso Lorenzo R, Perea Hevia L, Ramos Perera Y. Selección del paciente para cirugía refractiva: actualización. Rev Cubana Oftalmol [Internet]. 2015 Sep [citado 2020 Ago 11]; 28(3). Available in: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0864-21762015000... 4.Lysons D, Tapley J. Is microtropia a reliable indicator of the presence of amblyopia in anisometropic patients? Strabismus. 2018 Sep;26(3):118-121. doi:10.1080/09273972.2018.1503308. Epub 2018 Jul 30. 5.Hoyos JE, Cigales M, Hoyos-Chacón J, Maldonado-Bas A. Hyperopic laser in situ keratomileusis for refractive accommodative esotropia. J Cataract Refract Surg. 2002 Sep;28(9):1522-9. 6.Kirwan C, O´keefe M, O`múllanle GM, Sheehan C. Refractive surgery in patients with accommodative and non-accommodative strabismus: 1-year prospective follow-up. Br J Ophthalmol. 2010 Jul;94(7):898-902. doi: 10.1136/bjo.2009.162420. Epub 2009 Nov 30. 7.Gómez de Liaño-Sánchez R, Borrego-Hernando R, Franco-Iglesias G, Gómez de Liaño-Sánchez P, Arias-Puente A. Strabismus and diplopia after refractive surgery. Arch Soc Esp Oftalmol. 2012 Nov;87(11):363-7. doi: 10.1016/j.oftal.2011.12.006. Epub 2012 Jul 19. 8.Feng L, Lin H, Chen Y, Wang J, Wang Y, Lio R et all. The effect of Lasik surgery on myopic anisometropes' sensory eye dominance. Sci Rep. 2017 Jun 15;7(1):3629. 9.Pesudovs K. Involvement of neural adaptation in the recovery of vision after laser refractive surgery. J Refract Surg. Mar-Apr 2005;21(2):144-7.
Received 28.09.20
No conflict of interest was declared by the authors.
|