J.ophthalmol.(Ukraine).2020;5:43-50.
|
http://doi.org/10.31288/oftalmolzh202054350 Received: 16 June 2020; Published on-line: 27 October 2020
Pediatric orbital fractures: clinical and CT features and criteria for selecting a treatment option A. S. Slobodianiuk1, I. V. Chepurnyi 1,2,3, V. P. Efimenko 3, Iu. V. Shuklina 3, A. V. Kopchak 2,3, O. V. Petrenko4, L. M., Iakovenko3, S. O. Rykov4 1 Center for Maxillofacial Surgery and Dentistry, Kyiv Regional Clinical Hospital; 2 Bogomolets National Medical University; 3 Dobrobut LLC; 4 Shupik National Academy of Post-Graduate Education; Kyiv (Ukraine) E-mail: 80667788837@ukr.net TO CITE THIS ARTICLE: Slobodianiuk AS, Chepurnyi IV, Efimenko VP, Shuklina IuV, Kopchak AV, Petrenko OV, Iakovenko LM, Rykov SO. Pediatric orbital fractures: clinical and CT features and criteria for selecting a treatment option. J.ophthalmol.(Ukraine).2020;5:43-50. http://doi.org/10.31288/oftalmolzh202054350 Background: Pediatric traumatic orbital injuries have a number of clinical and CT features. Purpose: To assess the clinical and CT features of pediatric orbital fractures and the influence of these features on the choice among treatment options, and to develop practical recommendations on the basis of the review of long-term treatment outcomes for this type of trauma. Material and Methods: Medical records and CT scans of 27 pediatric patients with orbital wall fractures were retrospectively reviewed. We reviewed traumatic event circumstances, patient age and gender, type and frequency of clinical symptoms, terms and extent of care provided, and CT findings. Results: The most common clinical symptom was diplopia (55.5%). Limited eye movement was found in 37%, and enophthalmos, in 44.4% of patients. Trapdoor fractures were found in 51.9% of patients. Conclusion: The major clinical signs of pediatric orbital wall fractures were diplopia and limited upward eye movement. Trapdoor fracture was the most common type of orbital injury among patients of this study. Because radiography showed no evidence of impairment of orbital wall bones in 22.2% of patients of this study, findings of clinical examination become essential evidence in the diagnosis of pediatric fractures. Time of care provision and active surgical management are important when treating pediatric patients with orbital fractures. Keywords: orbit reconstruction, pediatric orbital trauma, diplopia
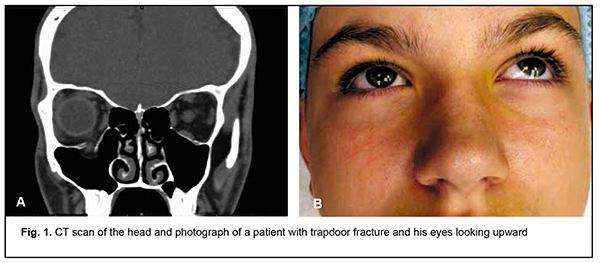
Introduction Improving management of patients with orbital wall fractures is essential for maxillofacial surgery practice and of high medical and social importance. This type of trauma is relatively common and accounts for 2% to 10% of all facial bone fractures [1, 2]. Algorithms for treating adults with orbital wall fractures have been described in detail in the literature. In addition, these algorithms continue to improve through implementation of novel diagnostic and treatment methods, particularly, trauma analysis systems and applications of patient-specific implants [1-3]. There are, however, differences in clinical and CT findings between pediatric and adult patients with traumatic orbital injuries [1,4-6]. Although these injuries are less common in children than in adults, their possible complications make them medically and socially important [1,4-6]. Best management strategy in children with orbital trauma remains controversial, particularly with regard to selecting treatment tactics, optimal time point and the method to be employed (customary ) for surgical treatment [1,6]. This is due to the structure and development of the pediatric viscerocranium as well as lack of consensus on the effect of treatment measures on midface development [1,4-7]. Adequate verbal contact between the doctor and the pediatric patient cannot be obtained, and psychoemotaional status of pediatric patients is age-specific; this contributes to difficulties in the diagnosis and treatment of pediatric orbital trauma. Objective factors also contribute to difficulties in the diagnosis, when increasing symptoms of traumatic brain injury and concomitant facial bone fractures mask the presence of functional abnormalities and anatomical changes resulting from orbital trauma [4-6, 8-10]. Orbital roof fractures tend to occur in children younger than 8 years, whereas orbital floor fractures, in older children, which is caused by stage of craniofacial skeletal development and tooth eruption in children [4-6, 11]. In addition, resilient bone tissue is characteristic for pediatric viscerocranium. It is this that causes orbital-floor blowout fractures of the trapdoor variety, first described by Soll and Poley [5, 8]. In this type of fracture, local damage to the orbital wall results from abrupt dislocation of the eye globe after the eye sustained a blow. A bone fragment from the thinnest site of the orbital floor gets displaced to the maxillary sinus. The resulting defect gets displaced and retraction of the inferior rectus takes place. However, the bone fragment restores its initial position due to above mentioned tissue elasticity, leading to entrapment of soft tissue structures between bone fragments (Fig. 1).
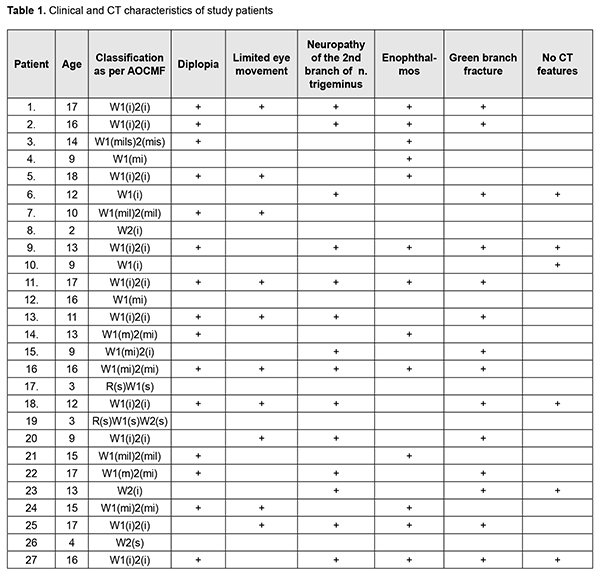
As publications on this topic are scarce, we believe it is important to summarize and overview the experience of treating this type of trauma in children. The purpose of this study was to assess the clinical and CT features of orbital fractures in children and their influence on the choice among treatment options, and to develop practical recommendations on the basis of the review of long-term treatment outcomes for this type of trauma. Material and Methods Of the 578 medical records of patients who were treated for midface fractures at the Center for Maxillofacial Surgery and Dentistry of Kyiv Regional Clinical Hospital, Head and Neck Surgery Department of Dobrobut Medical Network, and Pediatric Surgical Dentistry and Maxillofacial Surgery Department of Bogomolets National Medical University during 2014 through 2019, 27 satisfied the criteria and were included in this retrospective study. Inclusion criteria were age younger than 18 years, presence of isolated orbital wall fractures, and history of zygomatic complex reposition and fixation. Exclusion criteria were zygomatic complex fractures associated with orbital wall fractures; gunshot wounds; posttraumatic neurological abnormalities of central origin; non-compliance or no informed consent for the study; or no potential to collect complete medical data for analysis. All patients were examined as per routine (complaint and history taking,, and assessing clinical symptoms and the ocular status). We reviewed traumatic event circumstances, patient age and gender, type and frequency of clinical symptoms, terms and extent of care provided, and CT findings. All patients had CT scanning of the head. Assessment of ocular status comprised visual acuity and field testing; follow the finger eye test; traction test; exophthalmometry, and orbital volume assessment. Patients were diagnosed according to the AOCMF craniomaxillofacial fracture classification system [12]. The study protocol was approved at the meeting of the Bioethics Expert Committee at Bogomolets National Medical University (Meeting Minutes No. 126 dated November 13, 2019). Measures to ensure safety, health, rights and dignity of patients and to adhere to ethical standards were taken when conducting the study. Procedures related to the current study were performed in accordance with the principles of the Declaration of Helsinki, Convention for Human Rights and Biomedicine of the Council of Europe, and relevant laws of Ukraine. Data are presented as mean and standard deviation (SD). Differences between parameters were examined by Mann-Whitney test or Pearson chi-square test. The level of significance p ≤ 0.05 was assumed. Statistical analyses were conducted using SPSS software (IBM SPSS, USA). Results Orbital wall fractures accounted for 9.94% of all traumatic injuries of the viscerocranium in pediatric patients. Most pediatric patients were male, and the male-to-female ratio was 3:1. Patient age varied from 3 to 18 years (mean age, 12.33 ± 4.4 years). Crime-related traumas (as a result of assault or fighting) were most common (51.9%), followed by traffic-accident related (22.1%), home-related (18.5%), and sport-related (7.4%) traumas. The mean time between the traumatic event and presentation was 13.57 ± 25.74 days. In addition, 51.9% of patients presented within a week after the traumatic event. The mean time between presentation and surgical treatment was 5.5 ± 5.1 days. Approximately 37% of patients received surgical intervention within two days after presentation. Orbital floor fractures were most common (87%). Of the orbital floor fractures, 37% were associated with an orbital medial wall fracture, and 11.1%, with an orbital lateral wall fracture. Orbital roof fractures were found in 14.8% of patients. No isolated orbital medial or lateral wall fracture was found. Orbital fractures were associated with fractures of other facial bones in 51.9% of patients, and with traumatic brain injury, in 22.2% of patients. The most common clinical symptom was diplopia (55.5%). Limited eye movement was present in 37%, and neuropathy of the second branch of the trigeminal nerve, in 55.5% of patients. Enophthalmos was found in 44.4% of patients, and was the only change in globe position found among patients. No exophthalmos, hypophthalmus, or superior orbital fissure syndrome was found. Only one patient exhibited reduced visual acuity. Trapdoor fractures were found in 51.9% of patients. All patients with trapdoor fractures exhibited diplopia and limited upward eye movement. In addition, radiography showed no evidence of bone impairment in 22.2% of patients. A diagnosis was established on the basis of clinical findings as well as a comparison of complaints with history data. The presence of adipocele in the maxillary sinus lumen and CT evidence of a break in the inferior rectus with intraoperative finding of inferior rectus entrapment at the site of defect (Table 1) were considered indirect signs of orbital fracture.
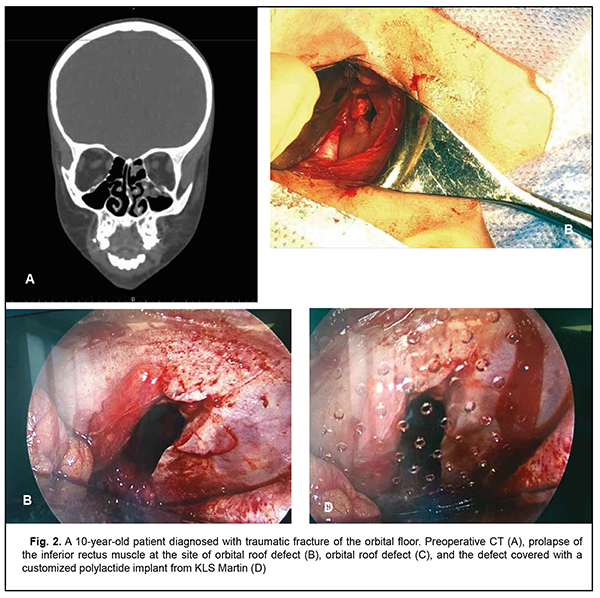
Of the 27 study patients, 24 (88.9%) required surgical treatment, and the rest 3 (11.1%) were judged to be suitable for observation and conservative management. Surgery aimed to restore the structural integrity of the viscerocranium, release entrapped extraocular muscles and retrobulbar cell tissue at the bone defect site, and reconstruct orbital wall defects. The main indications for surgery were diplopia, severely limited eye movement and cosmetic abnormalities caused by displacement of the globe. Reconstruction of orbital wall defects was performed in 88.9% of patients. Patient-specific implants and conventional titanium plates were utilized in 51.9% and 44.4% of patients, respectively, and a polylactide implant, in one patient. Mean post-surgical follow-up was 18.6 ± 6.4 months. Active surgical management resulted in substantial improvement or resolution of functional and cosmetic abnormalities. On month 3 after surgery, 18.5% of patients still had diplopia. In addition, over the follow-up period, enophthalmos was found in 11.1% of patients, and we managed to suppress oculomotor impairment and neuropathy of the second branch of the trigeminal nerve in all patients who underwent surgical management. Surgery outcome did not depend on the method used for implant-assisted reconstruction of orbital wall defects (Fig. 2).
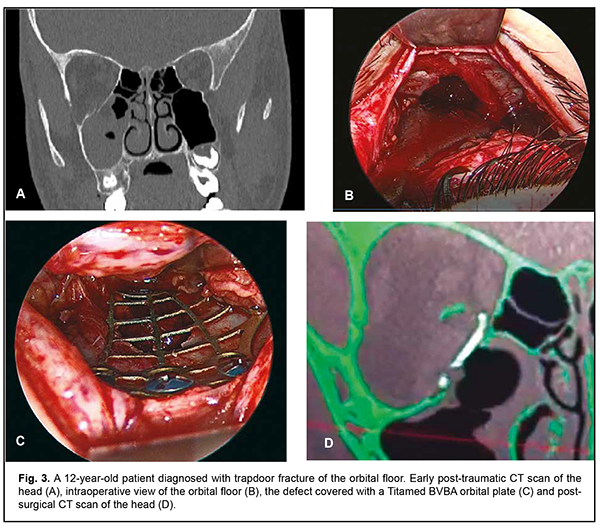
The difference in volume between healthy and affected orbits decreased statistically significantly from 1.2 ± 1.6 cm3 pre-surgery to 0.4 ± 0.5 cm3 post-surgery. In addition, among the 14 patients with trapdoor fracture, the difference in volume between healthy and affected orbits decreased from 0.3 ± 0.3 cm3 pre-surgery to 0.22 ± 0.28 cm3 post-surgery, but was not significant (p = 0.240). Discussion Although not common, pediatric orbital trauma is important due to the potential for visual impairment (particularly, diplopia, and/or loss of visual acuity and visual fields) and importance of visual function for the human quality of life [1, 4-6]. In pediatric orbital trauma, not only the osseous walls of the orbit, but also the eye as a functional organ of the body are affected. Progressive orbital swelling, imminent retrobulbar hematoma, and commotio oculi contribute to the risk of visual impairment, and, if present in eyes with retinal detachment and optic atrophy, contribute to the risk of blindness. Extraocular muscle entrapment, oculomotor nerve impairment and impairment of orbital fascial structures are accompanied by oculomotor abnormalities and diplopia. Prolapse of orbital content into adjacent cavities and atrophy of the retrobulbar cellular tissue may become a precondition for the development of enophthalmos. That is why early diagnosis of this type of trauma and selecting an optimal treatment strategy requires a multispecialist approach [1, 2, 6, 8-10]. The issues related to treatment of orbital wall fractures in children are still being debated. Particularly, the influence of surgical intervention on the growth and development of the viscerocranium is still controversial. Berger (2012) [7] reported that the orbits complete half of their postnatal growth within the first 2 years of life, with adult dimensions of the orbital cavities usually attained by 7 years of age. Therefore, on the basis of the data from studies on orbital growth with age, it has been concluded that conventional orbital reconstruction methods (particularly, titanium plates and mashes, and patient-specific implants) for orbital wall fractures can be used in children of 7 years and older [1, 4, 8-10]. In addition, our findings confirm the notion that orbital roof fractures tend to occur in children younger than 8 years. Particularly, of our 4 orbital wall trauma patients younger than 8 years, only one was diagnosed with orbital floor fracture. On the contrary, of our 23 orbital wall trauma patients older than 8 years, most had orbital floor defects that were rarely associated with orbital medial- or lateral wall defects, and only one was diagnosed with orbital roof fracture. Most researchers believe that the reasons why certain types of orbit fractures tend to occur in specific age groups are (1) the features of the adjacent paranasal sinuses, (2) the mechanisms of craniofacial skeletal development associated with secondary dentition and (3) predominance of traumatic brain injury resulting from direct damage to the frontal skull bone, particularly due to falls. In children younger than 8 years, the orbital roof is thin and, in the absence of the frontal sinus, frequently affected in traumatic brain injury [1, 7-9, 11]. In addition, in the mixed dentition period, permanent tooth germs are located directly beneath the orbital floor, and the inferior orbital wall is reinforced by this arrangement of permanent tooth germs as well as undeveloped maxillary sinus. Subsequently, with increasing age and orbital and maxillary bone volumes, tooth germs become located closer to alveolar bones, and this affects biomechanical characteristics and load distribution in the midface [7, 9]. In neonates, the ethmoidal cells are structures filled with water. They grow until the age of 12. With increasing growth of the ethmoid bone, the medial orbital wall becomes thinner. Consequently, by the time the individual reaches the adulthood, the ethmoid bone becomes more susceptible to fractures [1, 7, 11]. Without a doubt, orbital traumas in children are less common than in adults; they account for 2-10% of face bone fractures in adults [1, 2]. However, pediatric orbital trauma is characterized by a high risk of ocular abnormalities (diplopia and limited eye movement), which was confirmed by our studies [1, 5, 8-11]. This is caused by another feature of pediatric viscerocranium, marked elasticity of the bone tissue and ligaments. The elasticity of canthal ligaments, tarsal fascia, and periosteum contributes to the stability of osseous orbit walls and the globe. Orbital ligaments can retain bone fragments during the traumatic event, thus resisting the displacement of the eye [9-11]. Apart from resisting the development of impairment, this feature is important in the development of trapdoor fractures as mentioned above. Trapdoor fractures were seen in 51.9% of patients of the current study. Muscle entrapment results in muscle ischemia, leading to limited eye movements and diplopia. However, impairment of orbital walls may not be seen on CT scan if the affected bone fragment restores its initial position [4, 8-10]. That is why, in this series of observations, diplopia, limited upward eye movement and negative traction test were the prevailing symptoms of trapdoor fractures. In addition, more than 20% of cases had no CT evidence of fractures, and the orbital floor fracture was confirmed intraoperatively (Fig. 3).
The literature recommends that surgery for trapdoor orbital floor fracture should be performed within 48 hours after the traumatic event, to prevent irreversible changes in fatty tissue and the inferior rectus muscle [1, 7, 9, 11]. Surgery for conventional orbital floor or medial wall blowout fractures should be performed 5 to 14 days after the traumatic event [1, 2, 4, 8]. It is noteworthy that there was an extremely long time between the traumatic event and presentation in the presence of a high frequency of functional abnormalities for our patients with these fractures. In addition, there was a long time between diagnosis and surgical treatment. We believe that this was caused by the low level of awareness among Ukrainian specialists about the features of pediatric orbital fractures as well as the absence of substantial CT evidence of abnormalities. Expectant management in pediatric orbital trapdoor fractures has been reported to result in degenerative changes in the extraocular muscles and long postoperative rehabilitation times [1, 4, 8, 10]. Given the results of the analysis of changes in orbital volume and the above features, pediatric orbital trauma is characterized by a high risk of ocular abnormalities (diplopia and limited eye movement) in the presence of insignificant structural abnormalities of the orbital walls (predominantly, the inferior orbital wall). Therefore, if major abnormalities are caused by entrapped extraocular muscles, given a relatively low risk of enophthalmos and globe displacement, it is early diagnosis, active surgical management and time of care provision rather than a particular method for reconstruction of orbital floor defects (titanium plate, bioresorbable polymeric plate or patient-specific implants) that is important in planning treatment measures. Bioresorbable plates and clamps should be given a higher priority in the management of blow-out fractures of the orbital walls in children younger than seven or eight years, whereas adult clinical protocols may be used in the management of these fractures in older children.
References 1.Kwon JH, Moon JH, Kwon MS, Cho JH. The differences of blowout fracture of the inferior orbital walls between children and adults. Arch Otolaryngol Head Neck Surg. 2005;131(8):723-7. 2.Astapenko OO, Malanchuk VO, Chepurnyi YV, Logvinenko IP. [Peculiarities of the first aid to patients with orbital injuries]. Oftalmol Zh. 2015; 2:32-8. Ukrainian. 3.Chepurnyi Y, Chernogorskyi D, Kopchak A, Petrenko O. Clinical efficacy of peek patient-specific implants in orbital reconstruction. J Oral Biol Craniofac Res. 2020;10(2):49-53. 4.Dubois L, Steenen SA, Gooris PJ, Bos RR, Becking AG. Controversies in orbital reconstruction-III. Biomaterials for orbital reconstruction: a review with clinical recommendations. Int J Oral Maxillofac Surg. 2016; 45(1):41-50. 5.Soll DB, Poley BJ. Trapdoor variety of blowout fracture of the orbital floor. Am J Ophthalmol. 1965 Aug; 60:269-72. 6.Hink EM, Wei LA, Durairaj VD. Clinical features and treatment of pediatric orbit fractures. Ophthalmic Plast Reconstr Surg. Mar-Apr 2014; 30(2):124-31. 7.Berger AJ, Kahn D. Growth and development of the orbit. Oral Maxillofac Surg Clin North Am. 2012; 24(4):545-55. 8.Abdulkerimov TH, Mandra UV, Gerasimenko VI, Tseh DV, Samatov NR, Mandra EV, et al. [Epidemiology of the orbital wall fractures. Retrospective study]. Problemy stomatologii. 2019; 15(2):46–9. Russian. 9.Koltai PJ, Amjad I, Meyer D, Feustel PJ. Orbital fractures in children. Arch Otolaryngol Head Neck Surg. 1995;121(12):1375-9. 10.Stotland MA, Do NK. Pediatric orbital fractures. J Craniofac Surg. 2011; 22(4):1230-5. 11.Oppenheimer AJ, Monson LA, Buchman SR. Pediatric orbital fractures. Craniomaxillofac Trauma Reconstr. 2013;6(1):9-20. 12.Kunz C, Audigé L, Cornelius CP, Buitrago-Téllez CH, Rudderman R, Prein J. The Comprehensive AOCMF Classification System: Orbital Fractures - Level 3 Tutorial. Craniomaxillofac Trauma Reconstr. 2014; 7(Suppl 1): S092-102.
The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|