J.ophthalmol.(Ukraine).2020;5:75-78.
|
http://doi.org/10.31288/oftalmolzh202057578 Received: 19 May 2020; Published on-line: 27 October 2020 Prevalence of non-infectious corneal diseases P. M. Maharramov National Centre of ophthalmology named after acad. Zarifa Aliyeva; Baku (Azerbaijan) E-mail: maharramov@mail.ru TO CITE THIS ARTICLE:Maharramov PM. Prevalence of non-infectious corneal diseases. J.ophthalmol.(Ukraine).2020;5:75-78. http://doi.org/10.31288/oftalmolzh202057578 Purpose: To estimate the prevalence of non-infectious corneal diseases in the city of Baku. Material and Methods: We retrospectively reviewed databases of the outpatient polyclinics of the city of Baku in which the activities of ophthalmological departments were coordinated by the Acad. Zarifa Aliyeva National Ophthalmology Centre. Non-infectious corneal diseases were diagnosed on the basis of the clinical guidelines established by, and with involvement of specialists and equipment from the Acad. Zarifa Aliyeva National Ophthalmology Centre. Results: The most common clinical form was foreign body (54.0 ± 1.5 0⁄0000), followed by traumatic corneal erosion (47.7 ± 1.4 0⁄0000) and keratoconus (24.6±1.0 0⁄0000); chemical and thermal burns were less common (6.1 ± 0.5 0⁄0000). The age group of 0-9 years had the least prevalence (63.1 ± 4.3 per 100,000) and the age group of 101-9 years, a more than twice higher prevalence (120.9 ± 7.0 0⁄0000 per 100,000) of total non-infectious corneal diseases. The next two age groups had statistically increased prevalences of these diseases, 152.1 ± 6.1 and 262.5 ±9.2 0⁄0000, respectively. Conclusion: Estimated prevalence of non-infectious corneal diseases at a population level was 166.9 ± 2.7 0⁄0000, with the most common clinical form being foreign body (54.0 ± 1.5 0⁄0000), followed by traumatic corneal erosion (47.7 ± 1.4 0⁄0000), keratoconus (24.8 ±1.0 0⁄0000), and corneal dystrophy and degeneration (16.1 ± 0.8 0⁄0000). The age group of 60-69 years had the highest prevalence of total non-infectious corneal diseases (275.9 ± 12.6 0⁄0000), and foreign body prevalence was highest in the age group of 40-49 years (117.6 ± 6.2 0⁄0000), the prevalence of corneal dystrophy and degeneration was highest in the age group of 70-79 years (93.2 ± 12.0 0⁄0000), and the prevalence of traumatic corneal erosion was highest in the age group of 60-69 years (130.6 ± 8.7 0⁄0000). Key words: non-infectious diseases, cornea, prevalence
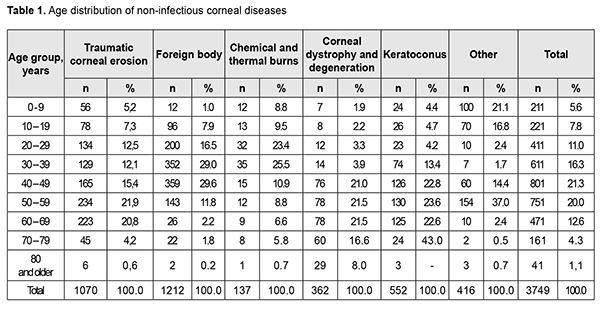
Introduction Corneal diseases are common eye disorders leading to severe medical, economical and social consequences. The results of the analysis of the overall burden and the epidemiology of keratitis in the United States by Collier and colleagues [1] showed that office and outpatient clinic visits occupied over 250,000 hours of clinician time annually, and episodes of keratitis and contact lens disorders costed an estimated $175 million in direct health care expenditures. Corneal diseases include dozens of nosologic entities that differ from one another in character of lesion and etiology [2]. Lee and colleagues [3] distinguish between three groups of corneal diseases, infectious, non-infectious and tumors. Non-infectious corneal diseases include bullous keratitis, corneal degeneration, chemical and thermal burns, corneal dystrophy, foreign body, neovascularization, staphyloma, keratoconus, Mooren’s ulcer and corneal leucoma. Epidemiological characteristics of these diseases have been poorly studied, although numerous reports have been published on some nosologic entities [4 – 9]. The purpose of the study was to estimate the prevalence of non-infectious corneal diseases in the city of Baku. Material and Methods We retrospectively reviewed databases of the outpatient polyclinics of the city of Baku in which the activities of ophthalmological departments were coordinated by the Acad. Zarifa Aliyeva National Ophthalmology Centre. Non-infectious corneal diseases were diagnosed on the basis of the clinical guidelines [1] established by, and with involvement of specialists and equipment from the Acad. Zarifa Aliyeva National Ophthalmology Centre. Diagnoses of non-infectious corneal diseases of 3749 patients were confirmed within the calendar year of 2017; data on the age composition of these patients are shown in Table 1. Data on the age composition of the population were obtained from the State Statistics Committee. Prevalences of particular corneal diseases per 100,000 population were calculated for particular age groups. Methods of qualitative data analysis were employed for statistical analyses [10]. Mean error for annual prevalence per 100,000 population was calculated using the following formula: (√p*(100000-p)/n), where p is the prevalence per 100,000 population, and n is the population size.
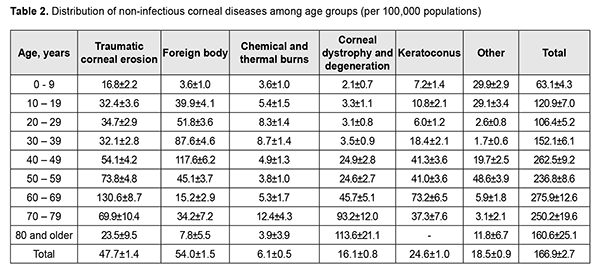
Results The most common age groups for total non-infectious corneal diseases were 40-49 years (21.3%), 50-59 years (20.0%) and 30-39 years (16.3%). There were differences in age composition among groups of patients with traumatic corneal erosion, corneal dystrophy and degeneration, keratoconus and other non-infectious corneal diseases. The 50-59 years and 60-69 years were the two most common age groups for traumatic corneal erosion (21.9 and 20.8%), corneal dystrophy and degeneration (21.5 and 21.5%) and keratoconus (23.6 and 22.6%). Table 2 shows prevalences of total and particular non-infectious corneal diseases for different age groups. The total prevalence of non-infectious corneal diseases was 166.9 ± 2.7 per 100,000. The most common clinical form was foreign body (54.0 ± 1.5 0⁄0000), followed by traumatic corneal erosion (47.7 ± 1.4 0⁄0000) and keratoconus (24.6 ± 1.0 0⁄0000); chemical and thermal burns were less common (6.1 ± 0.5 0⁄0000). Age-related changes in prevalence for total non-infectious corneal diseases when examined on decadal basis were non-linear (Table 2), with the age group of 0-9 years having the least prevalence (63.1±4.3 per 100,000) and the age group of 101-9 years, a more than twice higher prevalence (120.9±7,0 0⁄0000). There was no substantial difference in the prevalence of total non-infectious corneal diseases between the age group of 20-29 years (106.4±5.2 0⁄0000) and the age group of 10-19 years. The next two age groups had statistically increased prevalences of these diseases, 152.1±6.1 and 262.5±9.2 0⁄0000, respectively. The age group of 50-59 years had lower prevalence of total non-infectious corneal diseases than the age group of 40-49 years, although the difference was not significant (236.8 ± 8.6 0⁄0000 versus 262.5 ± 9.2 0⁄0000, p ˃ 0.05). In addition, this was true for the comparison between the age group of 60-69 years (275.9 ± 12.6 0⁄0000) and the age group of 70-79 years (250.2 ± 19.6 0⁄0000). It was well seen that the prevalence of total non-infectious corneal diseases was high and stable for the age range of 40-79 years.
The age group of 0-9 years had the least prevalence of foreign body (the most common clinical form among non-infectious corneal diseases), followed by the age group of 80 years and older (3.6±1.0 0⁄0000 and 7.8 ± 5.5 0⁄0000), whereas the age group of 40-49 years had the highest prevalence of this disorder. Foreign body prevalence increased for the age groups 0-9 to 40-49, and decreased for the age groups 50 and over. Prevalence of corneal traumatic erosion tended to increase linearly from birth to the age of 69 years; it, however, tended to decrease with age after 69 years due to low incidence of outpatient visits. There was no substantial difference in prevalence of this disorder between the age groups 10-19, 20-29, 30-39 (32.4 ± 3.6, 34.7 ± 2.9 and 32.1 ± 2.8 0⁄0000, respectively). Keratoconus was the third most common non-infectious corneal disease. The onset of the disease relatively frequently occurs in young individuals, but prevalence increased with age in a clearly linear fashion due to accumulation effect. The age group of 0-9 years had the least annual keratoconus prevalence (7.2 ± 1.4 0⁄0000). Prevalence was relatively stable until the age of 30 (10-19 age group, 10.8 ± 2.1 0⁄0000; 20-29 age group, 6,0±1,2 0⁄0000; p ˃ 0.05), and substantially increased for the age group of 30-39 years (18.4 ± 2.1 0⁄0000). The prevalence of corneal dystrophy and degeneration by age was low until the age of 40 (0-9 years, 2.1 ± 0.7 0⁄0000; 10-19 years, 3.3 ± 1.9 0⁄0000; 20-29 years, 3.1 ± 0.8 0⁄0000; 30-39 years, 3.5 ± 0.9 0⁄0000), and increased thereafter with a peak in individuals older than 80 years (13.6±21.1 0⁄0000). For these disorders the age trend was linear. The accuracy of the linear regression equation describing changes in the prevalence of these disorders with age was 80.5% (R²=0.805). Chemical and thermal burns of the cornea were infrequent in all age groups, with a prevalence ranging from 3.6 ± 1.0 to 12.4 ± 4.3 0⁄0000 (p ˃ 0.05). Therefore, nosologic entities of non-infectious corneal diseases differed in epidemiological characteristics. Discussion Although the age composition of our study patients with non-infectious corneal diseases differed from that of patients from a Chinese study [3], the two studies shared some common age-related features, with patients 40-49 years of age constituting the largest group, and patients aged 80 years and older constituting the smallest group. Leucoma, keratoconus, Murren ulcer, corneal dystrophy and chemical burns were the five most common non-infectious corneal diseases in the Chinese study. The most common non-infectious corneal disease in the current study was foreign body, followed by corneal erosion, keratoconus, corneal dystrophy and degeneration, and chemical and thermal burns. It is well seen that a high proportion of corneal erosions among non-infectious corneal diseases is characteristic for a Baku population. The frequency of keratoconus and corneal degeneration in a cohort of Italian patients with obstructive sleep apnoea were significantly higher than in the present study (12% versus 0.024% and 0.7% vs 0.016%, respectively). The prevalence of keratoconus among a Palestinian population [6] was more than 50 times higher than in a Baku population (1500 versus 24.6 0⁄0000). Therefore, prevalence of non-infectious corneal diseases in the city of Baku has distinctive features that may have an effect on the character of eye care. To conclude, estimated prevalence of non-infectious corneal diseases at a population level was 166.9 ± 2.7 0⁄0000, with the most common clinical form being foreign body (54.0 ± 1.5 0⁄0000), followed by traumatic corneal erosion (47.7 ± 1.4 0⁄0000), keratoconus (24.8 ±1.0 0⁄0000), and corneal dystrophy and degeneration (16.1 ± 0.8 0⁄0000). The age group of 60-69 years had the highest prevalence of total non-infectious corneal diseases (275.9 ± 12.6 0⁄0000), and foreign body prevalence was highest in the age group of 40-49 years (117.6 ± 6.2 0⁄0000), the prevalence of corneal dystrophy and degeneration was highest in the age group of 70-79 years (93.2±12.0 0⁄0000), and the prevalence of traumatic corneal erosion was highest in the age group of 60-69 years (130.6 ± 8.7 0⁄0000). References 1.Collier SA, Gronostaj MP, MacGurn AK, et al. Estimated burden of keratitis – United States, 2010. MMWR Morb Mortal Wkly Rep. 2014 Nov 14; 63(45): 1027–30. 2.Moshetova LK, Nesterov AP, Egorov EA, eds. [Ophthalmology. Clinical recommendations]. GEOTAR-Media: Moscow; 2016. Russian. 3.Li X, Wang L, Dustin L, Wei Q. Age distribution of various corneal diseases in China by histopathological examination of 3112 surgical specimens. Invest Ophthalmol Vis Sci. 2014 May 8;55(5):3022-8. 4.Pedrotti E, Demasi C, Bruni E, et al. Prevalence and risk factors of eye diseases in adult patients with obstructive sleep apnoea: results from the SLE.E.P.Y Cohort Study. BMJ Open. 2017; 7(10): e016142. 5.Lin Z, Chen J, Cui H. Characteristics of corneal dystrophies: a review from clinical, histological and genetic perspectives. Int J Ophthalmol. 2016; 9(6):904–13. 6.Shehadeh M, Diakonis V, Jalil S, et al. Prevalence of keratoconus among a Palestinian Tertiary student population. Open Ophthalmol J. 2015;9:172–6. 7.Qu J-H, Li L, Tian L, et al. Epithelial changes with corneal punctate epitheliopathy in type 2 diabetes mellitus and their correlation with time to healing. BMS Ophthalmology. 2018 Jan 4;18(1):1. 8.Diez–Feijoo E, Grau A, Abusleme E, Duran J. Clinical presentation and causes of recurrent corneal erosion syndrome: review of 100 patients. Cornea. 2014 Jun;33(6):571-5. 9.Dolzhich RR, Piatnitsyna VV. [A combination technique for treating recurrent corneal erosions]. Problemy oftalmologii. 2008;1:47-8. Russian. 10.Stenton G. [Medical and biological statistics]. Praktika: Moscow; 1999. Russian.
The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|