J.ophthalmol.(Ukraine).2020;3:31-36.
|
http://doi.org/10.31288/oftalmolzh202033136 Received: 28 February 2020; Published on-line: 24 June 2020 Efficacy of radiowave surgery in the treatment of patients with iris and ciliary body melanoma A.P. Maletskiy, Dr Sc (Med); O.V. Khomiakova SI “The Filatov Institute of Eye Diseases and Tissue Therapy of the National Academy of Medical Sciences of Ukraine”; Odesa (Ukraine) E-mail: maletskiy@filatov.com.ua TO CITE THIS ARTICLE: Maletskiy A.P., Khomiakova O.V. Efficacy of radiowave surgery in the treatment of patients with iris and ciliary body melanoma. J.ophthalmol.(Ukraine).2020;3:31-36. http://doi.org/10.31288/oftalmolzh202033136 Purpose: To determine the efficacy of resecting iris and ciliary body melanoma with the use of a 3.8-4.0-Mhz radiowave surgery unit. Material and Methods: This study was conducted at Department of Eye Cancer, the Filatov Institute, from 2005 through 2018. The study group involved 45 patients with iris and ciliary body melanoma; the mean age was 56.3 ± 2.2 years, with a slight female predominance (53.3%). Sixty-seven patients who had undergone iridociliary melanoma excision using a conventional technique with cutting tools were used as retrospective controls. The eye examination included visual acuity measurement, perimetry, biomicroscopy and ophthalmoscopy. Tumor, nodus и metastasis (TNM) staging was according to the American Joint Committee on Cancer (AJCC). No metastases were seen at the time of enrollment. The mean tumor prominence at baseline was 4.0 ± 0.3 mm, with a mean base diameter of 8.3 ± 0.4 mm, corresponding to a tumor volume of 34.3 ± 0.7 mm3. All the patients of each group were divided into two subgroups based on baseline visual acuity. The study group involved subgroup 1A (n=37 patients; 82.2%) with a visual acuity of 0.1 to 0.5 and subgroup 1B (n=8 patients; 17.8%) with a visual acuity of 0.6 to 0.8, and the retrospective control group involved subgroup 2A (n=55 patients; 82.1%) with a visual acuity of 0.1 to 0.5 and subgroup 2B (n=12 patients; 17.9%) with a visual acuity of 0.6 to 0.8 (p > 0.05). The analysis was performed by analysis of variance (ANOVA) using Statistica 13.0 (Dell Statsoft Inc., Austin, TX). Results: The radiosurgical approach to treatment of iridociliary tumors in our patients allowed significantly reducing the rates of intraoperative and postoperative complications (?2=4.16; df=1; p=0.04). In addition, the rates of intraoperative and postoperative complications for the treatment of iridociliary tumors with cutting instruments were 9.1% and 10.4%, respectively. The use of a radiowave surgery unit for uveal melanoma resection allowed preserving baseline visual acuity in all patients, with a tumor recurrence rate of not more than 2.2%. Conclusion: Early (12-month) treatment outcomes (visual functions and postoperative clinical course) and late treatment outcomes (visual functions; optic media; IOP; and tumor recurrence) for iridociliary melanoma resection using a radiowave 3.8-4.0 MHz unit allow us to state that high-frequency radiowave surgery enables reducing the risk of intraoperative and postoperative complications and, consequently, preserving a good visual function. Keywords: uveal melanoma, radiowave surgery unit, treatment
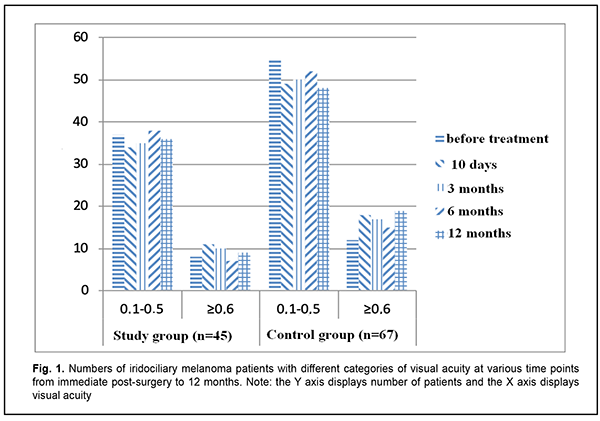
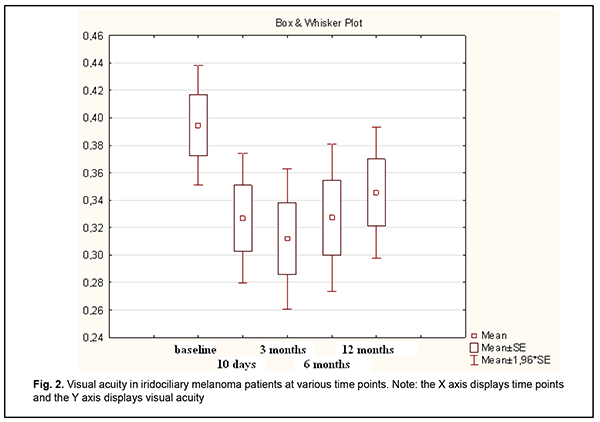
Introduction Uveal melanoma is a highly malignant tumor of the eye with a global annual incidence of more than 7,000 cases, and mean age-adjusted incidence of 4.3 per million [1, 2]. There is a nearly equal distribution of primary uveal melanoma by gender [2]. Caucasians and Hispanic Americans represent 98% and 1%, respectively, of cases in the US, and the rest (<1%) is attributed to American Asians, Africans and Native Americans. The disease is most commonly diagnosed in individuals aged 50-60 years (mean age, 55 years) [1, 2]. The age-adjusted incidence increases with increasing age until about age 70-75, then plateaus [1]. Approximately 90% of uveal melanomas arise in the choroid, 6% in the ciliary body, and the remaining 4% in the iris [2]. Therapy for uveal melanoma depends on the site and size of the tumor, course of the disease, fellow eye status, and patient’s systemic status. In addition, the therapeutic approach is tailored to the needs of the individual. Management options include transpupillary thermotherapy, brachytherapy, stereotactic radiotherapy, limited surgical resection, enucleation and orbital exenteration [3]. Surgical removal of pre-equatorial tumors may be associated with peri-operative complications (like expulsive hemorrhage, partial vitreous hemorrhage, and retinal detachment) and post-operative complications (cataract, ocular subatrophy, etc.) [3, 4]. On the basis of analysis of complications in surgical removal of pre-equatorial tumors, we concluded that they are caused by the surgical technique itself. First, tumor resection using cutting tools may be associated with hemorrhage which is difficult to control. Second, combining tumor removal with simultaneous local brachytherapy increases a therapeutic load on the eye, leading to ocular hypotony and subsequently to ocular subatrophy [4]. Given the above, it appears that the rate of these complications may be reduced if tumor resection is combined with simultaneous vessel coagulation with a radiowave surgery unit [5]. This will allow not only reducing the traumatic effect on the eye but also meeting the principles of ablastics (prevention of intraoperative dissemination of tumor cells) and reducing the risk of intraoperative hemorrhage. While implementing the outlined technology for organ-preserving management of iridociliary melanoma, we encountered some issues for which we have failed to find appropriate solutions in the literature. In addition, the literature is scant on the use of RF surgery in uveal melanoma, and there is no data on appropriate modes for a RF surgery unit in manipulation of the sclera, iris, ciliary body and choroid. Findings of our previous experimental study [6] have demonstrated that this approach is promising for the treatment of uveal melanoma, and encouraged us for further research. The purpose of the study was to determine the efficacy of resecting iris and/or ciliary body melanoma with the use of a 3.8-4.0-Mhz radiowave surgery unit. Material and Methods This study was conducted at Department of Eye Cancer, the Filatov Institute, from 2005 through 2018. The study group involved 45 patients with iris and ciliary body melanoma; the mean age was 56.3 ± 2.2 years, with a slight female predominance (53.3%). Sixty-seven patients who had undergone iridociliary melanoma excision using a conventional technique with cutting tools were used as retrospective controls. There was no significant difference in age, male/female percentage, visual acuity, or intraocular pressure (IOP). The set of diagnostic procedures adhered to the clinical guidelines from the Ministry of Health Order “On Approval of Protocols for Provision of Medical Care to Patients with Eye Disease” [7]. The eye examination included visual acuity assessment measurement, perimetry, biomicroscopy and ophthalmoscopy. Tumor, nodus и metastasis (TNM) staging was according to the American Joint Committee on Cancer (AJCC) [3]. No metastases were seen at the time of enrollment. The mean tumor prominence at baseline was 4.0 ± 0.3 mm, with a mean base diameter of 8.3 ± 0.4 mm, corresponding to a tumor volume of 34.3 ± 0.7 mm3. Operation technique Eye speculum was placed in the eye after preoperative showering with chlorhexidine. The scleral conjunctival incision was made 2-4-mm (depending on exact tumor location) outside the limbus at the tumor site, and the scleral conjunctiva was separated. Scleral projection of the tumor was clarified based on the data obtained from near-infrared transillumination, and the sector of exact tumor location was marked. Scleral incision was performed in a layer-by-layer fashion. A 3.8-Mhz radiowave surgery unit (Surgitron, Ellman International) was used to remove the tumor with 2-3-mm normal adjacent tissue margins in patients of the study group. The unit was set to 35 W in the coagulation mode and to 70-90 W in the cut mode to perform vessel coagulation and tissue dissection, respectively. Interrupted sutures were used to close the scleral incision, the anterior chamber was washed with Ringer solution, and the conjunctiva was closed using uninterrupted silk suture. Patients received disinfectant eye drops, parabulbar antibiotic and steroid injections and aseptic dressing. Antibacterial and anti-inflammatory therapy was used postoperatively. Prospective follow-up duration was from 12 months to 13 years (median value, 3.5 years). All the patients of each group were divided into two subgroups based on baseline visual acuity. The study group involved subgroup 1A (n=37 patients; 82.2%) with a visual acuity of 0.1 to 0.5 and subgroup 1B (n=8 patients; 17.8%) with a visual acuity of 0.6 to 0.8. The retrospective control group involved subgroup 2A (n=55 patients; 82.1%) with a visual acuity of 0.1 to 0.5 and subgroup 2B (n=12 patients; 17.9%) with a visual acuity of 0.6 to 0.8. The analysis was performed by analysis of variance (ANOVA) using Statistica 13.0 (Dell Statsoft Inc., Austin, TX) [8]. The tumor volume was calculated using the formula for rotation ellipsoid: V=4?ab2/3, where a is the tumor prominence, and b is half of tumor base diameter. Mean (M), median (Me), quartile (q1, q3), mean root square deviation (?) and standard error of mean (m) values were calculated. Non-parametric methods were used for group comparisons. The level of significance p ? 0.05 was assumed. Results No intraoperative complications were observed in the study group. In the early postoperative period (24 hours), one patient (1.4%) of this group exhibited local retinal detachment that was absent at the 4-month follow-up. In addition, two patients were diagnosed with hyphema. The condition was subject to routine treatment, and the two patients demonstrated no sequelae of this complication at the last follow-up visit. With regard to the control group, vitreous hemorrhage was the most common postoperative complication (7 patients; 10.5%), followed by retinal detachment (4 patients; 5.7%) and epiretinal fibrosis (1 patient; 1.5%). Therefore, the use of a radiowave surgery unit for melanoma resection in the study group allowed a significant decrease in the risk of postoperative complications compared with retrospective controls (?2=4.46, df=1, p < 0.05). With regard to the study group, mixed melanoma was the most common histological tumor type (23 patients; 51.1%), followed by spindle cell A melanoma (7 patients; 15.5%), spindle cell A-B (6 patients; 13.3%), spindle cell B melanoma (5 patients; 11.1%), and epithelioid cell melanoma (4 patients; 8.9%). This is in agreement with findings reported by others [3]. No significant decrease in vision was found in both groups within a year after surgery (Fig. 1). Although there was some decrease in visual acuity at 10-day, 3-, 6- and 12-month follow up visits, no critical decrease in visual acuity was observed in any case. Mean visual acuity in the study group was 0.32 ± 0.02 at 10 days, 0.31 ± 0.03 at 3 months, 0.32 ± 0.02 at 6 months and 0.34 ± 0.03 at 12 months (Fig. 2).
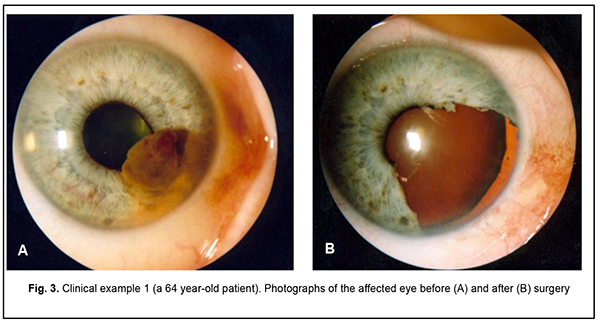
The use of a radiowave surgery unit allowed preserving baseline visual acuity over a year after surgery. With regard to the retrospective data for controls, only visual acuity data for the hospital stay period were available, and mean visual acuity at discharge was 0.33±0.03, which was comparable with the results for the study group. Of the nine study group patients with poor IOP control at baseline, only one (11.1%) showed high IOP at 12 months. Therefore, the use of a radiowave surgery unit for uveal melanoma resection allowed normalizing IOP in 88.9% of cases. All patients of the study group were still alive at 5 years, whereas of the 67 retrospective controls, 16 (23.9%) were found legally dead, and survival status was not available in 12 (17.9%) at 5 years. We believe that this difference may be explained by decreased dissemination of tumor cells in patients who underwent uveal melanoma resection using a radiowave surgery unit. As it has been reported that the five-year survival rate for patients with metastasis-free uveal melanoma was approximately 75% [1, 2], the rate for our patients with uveal melanoma may be considered satisfactory. Below we present representative clinical examples of iridociliary melanoma treated using a radiowave surgery unit. Clinical example 1 (patient Mr. U-ts, 64 years old, medical record No. 345672) The diagnosis was an iridociliary melanoma OD, and the tumor was classified as a T1 N0 M0. Clinical description: OD: A pigmented iris lesion involving the ciliary body extended from 3 to 5 o’clock. The tumor base and thickness measured 5.6 х 6.0 mm and 4.1 mm, respectively, by ultrasonography. Preoperative visual acuity was 0.8 (Fig. 3a). The patient had iridocyclectomy with the use of a Surgitron radiowave unit. Histopathologic examination revealed a spindle A-B cell iris melanoma with involvement of the ciliary body. No complications were observed within the course of treatment. Postoperative visual visual acuity was 0.8 (Fig. 3b). No recurrence was observed during a follow-up of 7 years and 8 months.
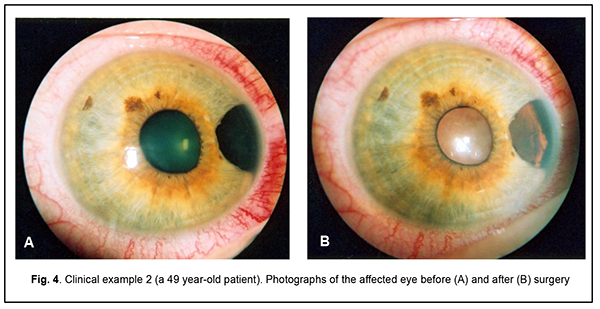
Clinical example 2 (patient Mr. M-r, 49 years old, medical record No. 352632) The diagnosis was an iridociliary melanoma OD, and the tumor was classified as a T1 N0 M0. Clinical description: OS: A pigmented iris lesion involving the ciliary body extended from 3 to 5 o’clock. The tumor base and thickness measured 3.5 х 4.0 mm and 2.1 mm, respectively, by ultrasonography. Preoperative visual acuity was 1.0 (Fig. 4a). The patient had iridocyclectomy with the use of a Surgitron radiowave unit. Histopathologic examination revealed a spindle A-B cell iris melanoma with involvement of the ciliary body. No complications were observed within the course of treatment. Postoperative visual visual acuity was 1.0 (Fig. 3b). No recurrence was observed during a follow-up of 6 years and 5 months.
The recurrence rate was 13.4% (9) in the control group and 2.2% (1) in the study group (?2=4.16; df=1; p=0.04). Discussion In the current study, the radiosurgical approach to treatment of iridociliary tumors in our patients allowed significantly reducing the rates of intraoperative and postoperative complications (?2=4.16; df=1; p=0.04). In addition, the rates of intraoperative and postoperative complications for the treatment of iridociliary tumors with cutting instruments were 9.1% and 10.4% [8], respectively, versus 3.6% and 7.5%, respectively, reported by others [1, 9]. Moreover, the use of a radiowave surgery unit for uveal melanoma resection allowed preserving visual acuity outcomes over a year after surgery in all patients. The tumor recurrence rate in the study group was 2.2%, which was significantly (p < 0.05) lower than in the control group. Early (12-month) treatment outcomes (visual functions and postoperative clinical course) and late treatment outcomes (visual functions; optic media; IOP; and tumor recurrence) for iridociliary melanoma resection using a radiowave 3.8-4.0 MHz unit allow us to state that high-frequency radiowave surgery enables reducing the risk of intraoperative and postoperative complications and, consequently, preserving a good visual function. Conclusion First, the use of a radiowave surgery unit for uveal melanoma resection allowed preserving baseline visual acuity in all patients. Second, the 24-month tumor recurrence rate was not more than 2.2% in the group of patients treated with the use of a radiowave surgery unit. Third, with regard to patients treated with the use of a radiowave surgery unit, the rate of postoperative complications was not more than 4.4%, and no intraoperative complications were observed. Fourth, iridociliary melanoma resection using a radiowave surgery unit allowed normalizing IOP in 88.9% of patients with manifestations of secondary glaucoma. Fifth, low complication and recurrence rates and improved 5-year survival rate allow us to recommend radiowave surgery as a surgical part of management of uveal melanoma. Finally, since patients who underwent uveal melanoma resection using a radiowave surgery unit exhibited a 100% survival rate at follow-up ranging to 13 years, it is likely that this approach prevents intraoperative dissemination of tumor cells. References 1.Aronow ME, Topham AK, Singh AD. Uveal Melanoma: 5-Year Update on Incidence, Treatment, and Survival (SEER 1973-2013). Ocul Oncol Pathol. 2018 Apr;4(3):145-151. 2.Papastefanou VP, Cohen VM. Uveal Melanoma. J Skin Cancer. 2011;2011:1–13. 3.Shields CL, Kaliki S, Furuta M, et al. American Joint Committee on Cancer Classification of Uveal Melanoma (Anatomic Stage) Predicts Prognosis in 7,731 Patients: The 2013 Zimmerman Lecture. Ophthalmology. 2015 Jun;122(6):1180-6. C 4.Kim JH, Shin SJ, Heo SJ, et al. Prognoses and Clinical Outcomes of Primary and Recurrent Uveal Melanoma. Cancer Res Treat. 2017 Dec 28. doi: 10.4143/crt.2017.534. 5.Chua V, Aplin AE. Novel therapeutic strategies and targets in advanced uveal melanoma. Curr Opin Oncol. 2018 Mar;30(2):134-41. 6.Khomiakova OV, Vit VV, Maletskyi AP. [Comparing structural changes in the rabbit’s uveal tract after the use of a radiowave surgery unit versus a cutting tool]. J Ophthalmol (Ukraine). 2019;4:43-48. Ukrainian. 7.Ministry of Health of Ukraine. [Order of Ministry of Health of Ukraine No. 117 “On Approval of Protocols for Provision of Medical Care to Patients with Eye Disease”]. Kyiv, Ukraine; 15 March 2007. https://zakononline.com.ua/documents/show/107241___107241 8.Rebrova OIu. [Statistical analysis of medical data. Application of STATISTICA software package]. Moscow: MediaSfera. 2002. Russian. 9.Smoliakova GP, Pikhovskaia IG, Luz’ianina IG, Sorokin EL. [Method for radiosurgical treatment of uveal melanoblastoma]. Patent of Russian Federation RU No. 2265423 A61F dated 10.09.2006. Patent owner: Far East State Medical University. Application filed on 20.02.2005. Information Bulletin No. 34 issued 10.12.2005. 10.Yang J, Manson DK, Marr BP, Carvajal RD. Treatment of uveal melanoma: where are we now? Ther Adv Med Oncol. 2018 Feb 21;10:1758834018757175. 11.Uveal Melanoma. Available at: https://eyewiki.aao.org/Uveal_Melanoma#targetText=Associated%20with%20th.... The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|