J.ophthalmol.(Ukraine).2020;3:61-64.
|
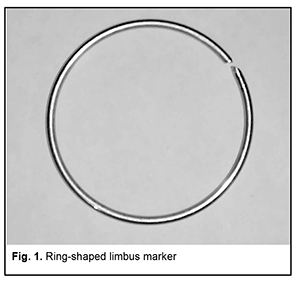
http://doi.org/10.31288/oftalmolzh202036164 Received: 26 February 2020; Published on-line: 24 June 2020 A method of marking the limbus during X-ray localization of IOFB in the presence of apparent chemosis or scleral subconjunctival hemorrhage N.V. Malachkova, I.A. Gabruk; I.I. Gabruk; O.O. Andrushkova, Pirogov Vinnytsia Regional Clinical Hospital; Vinnytsia (Ukraine) Pirogov National Medical University; Vinnytsia (Ukraine) E-mail: illyagabruk@i.ua TO CITE THIS ARTICLE: Malachkova N.V., Gabruk I.A., Gabruk I.I., Andrushkova O.O. A method of marking the limbus during X-ray localization of IOFB in the presence of apparent chemosis or scleral subconjunctival hemorrhage. J.ophthalmol.(Ukraine).2020;3:61-64. http://doi.org/10.31288/oftalmolzh202036164 The method proposed for marking the limbus during X-ray localization of IOFB in the presence of apparent chemosis or scleral subconjunctival hemorrhage is based on the use of a ring-shaped limbus marker made from 0.5-0.7-mm stainless steel wire. Rings with external diameters of 10, 11 and 12 mm are used for examining eyes of different sizes. A ring of the appropriate size is placed on the cornea against the limbus to perform X-ray examination. It is well fit in the specified position due to hypertrophy of the conjunctiva surrounding the cornea, and corresponds to the conjunctival attachment to the limbus. Orbit X-ray is performed, quality of X-ray films is assessed and IOFB position in the eye is calculated using the technique of Comberg-Baltin or Abalikhin-Pivovarov. In 12 patients, IOFB was successfully removed based on the data obtained from the use of this method. The accuracy of IOFB X-ray localization by means of the ring-shaped limbus marker was found to be the same as that by means of the Baltin’s prosthesis. Keywords: X-ray localization of intraocular foreign bodies, ring-shaped limbus marker
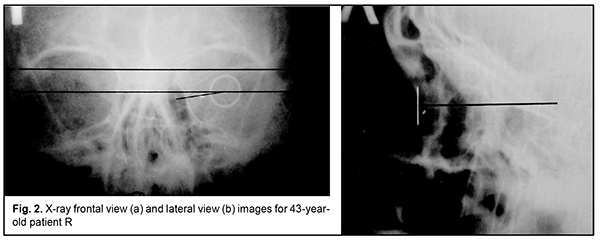
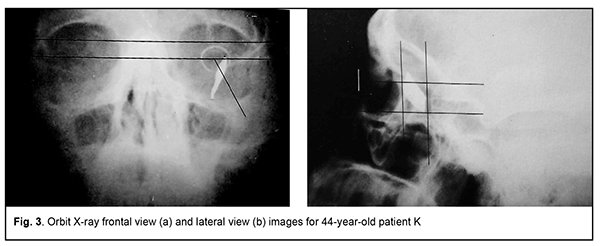
Introduction Ocular trauma is still a leading cause of loss of vision and legal blindness and vision impairment. Intraocular foreign bodies (IOFBs; such as metal, glass, rock, etc.) are seen in 15%-40% of penetrating ocular injuries [1, 2]. IOFBs sized 1-2 mm are most common and can cause early and late complications (endophthalmitis, metallosis, etc.) which are more significant in terms of their effect on health than the trauma caused by such a body itself. IOFBs sized more than 5 mm commonly cause significant damage to the eye, and may lead to loss of not only vision, but also of the whole eye. Accurate IOFB localization is essential for the success of IOFB removal. Until recently, orbit X-ray in two views using the Comberg-Baltin prosthesis was the primary imaging modality for localizing radiopaque IOFBs. Although other modalities can be used today for localizing radiopaque IOFBs, they do have certain diagnostic disadvantages. Because the X-ray method of foreign body localization is widely available, cost-effective, and offers sufficient accuracy for surgical planning, it is still relevant. It is used in combination with contemporary imaging modalities (CT, ultrasound, etc.) and, if these are unavailable, it can be used as the primary imaging modality. Although the ultrasound method is, undoubtedly, of value in localizing IOFBs, especially radiopaque ones, it cannot localize the IOFB accurately enough to remove the latter immediately. In addition, it is effective only if combined with the X-ray method. Computed tomography (CT) scan provides more differentiated images of ocular tissue and media, and can identify IOFB and precisely locate it with respect to the adjacent ocular structures in most cases. CT is the indispensable imaging examination technique in the presence of numerous IOFBs, but is not always effective in determining IOFB size and shape. In CT scans, a foreign body sized less than 3 mm appears as a regular round body, and that sized 3 to 7 mm appears as an irregularly round or oval-shaped body, although the actual size and shape may differ from those seen in the CT. CT images of metal IOFBs often suffer from bright and dark streak artifacts that radiate from the shadow of metal IOFB. If there is any possibility that the foreign body may be metallic, magnetic resonance imaging (MRI) should not be performed because of possible movement of the object and consequent damage to intraocular structures. Scleral subconjunctival hemorrhage is more commonly caused by larger IOFBs. In addition, hypertrophy of the scleral conjunctiva surrounding the limbus may arise from other causes such as allergic response, burns, consequences of severe concussion, etc. Marking the position at the limbus presents some difficulties in the presence of apparent chemosis or scleral subconjunctival hemorrhage. As it is difficult or impossible to make the Baltin prosthesis adjacent to the limbus under these circumstances, other methods have been proposed for marking the position at the limbus. Baltin [3] proposed to apply bismuth pulp to mark the limbus at 6 and 12 o’clock axes with a (preferably plastic) probe when the lids are separated with eye speculum. Bismuth pulp spreads over the eye and is washed away by tears rather frequently. In addition, the eye must be kept immobile during examination, which is almost impossible. Vodovozov [4] proposed to mix bismuth or barium sulfate with nitro-glue or collodion, make small silver-paper half-discs and soak them in this mixture, and use them to mark the limbus. These adhere well to the limbus, are not washed away by tears, and exhibit no displacement during movements of the eye. Poliak [5-6] proposed to introduce T-shaped studs beneath the conjunctiva at the limbus at 3 and 9 o’clock axes. Adhering, suturing or fastening various radiopaque markers at the limbus causes incongruous shadows on X-ray films, and can result in increased damage to the eye. Because radiopaque objects are placed by sight and hands and in one plane, approximately at certain meridians, location of the IOFB in the eye is estimated with a significant error. Marking the center of the cornea with a probe, dressing forceps, or other methods (Plittas, 1941; Bogatin, 1949; Madroszkiewiz, 1954, etc) have not been widely implemented due to their small effect [7]. A limbal ring (internal diameter, 12 mm) made of 1-mm thick wire, which is sutured or adhered to the conjunctival sclera, cannot mark the limbus in cases of hypertrophy of the scleral conjunctiva, and it is difficult or impossible to make the ring adjacent to the limbus. In addition, it should not be used in the presence of fresh, gaping wound [8-10]. Gardona and Trokel [11] used a soft vacuum lens for X-ray localization of foreign bodies in eyes with maintained corneal sphericity. Such a lens remains well secured and does not change its position over the cornea, which facilitates adequate localization of the IOFB. Taking into account the relevance of the problem, we have been looking for a new way to solve it. We made a corneal prosthesis (limbus marker; Innovation Proposal No. 556/54 dated 12.07.1989), which is a rigid corneal contact lens (optical power, 0D; diameter, 11 mm; thickness, 0.3-0.35) made of polymethylmethacrylate. The lens has 0.5-mm lead marks in four quadrants (3, 6, 9 and 12 o’clock); lead mark edges and lens edges coincide with each other. The distance between external contours of adjacent marks is 11 mm, and the distance between internal contours is 10 mm. The prosthesis is well fit in the specified position over the cornea during X-ray examination. It can be used if the conjunctiva and lens are abnormally spherical in shape (chemosis and/or subconjunctival hemorrhage) and in the presence of a fresh scleral wound. The purpose of the study was to improve the accuracy of X-ray localization of foreign bodies in the presence of apparent chemosis or scleral subconjunctival hemorrhage through the use of the ring-shaped limbus marker. Material and Methods We proposed a method for marking the limbus during X-ray localization of foreign bodies in the presence of apparent chemosis or scleral subconjunctival hemorrhage through the use of the ring-shaped limbus marker (Patent of Ukraine No. 12,015 issued 25.10.2017; Bulletin No. 20). The ring is made from 0.5-0.7-mm stainless steel wire. Rings with external diameters of 10, 11 and 12 mm were made for examining eyes of different sizes. The examination procedure was as follows. After epibulbar anesthesia, a sterile ring-shaped limbus marker of the appropriate size was placed on the cornea against the limbus. It was well fit in the specified position due to hypertrophy of the conjunctiva surrounding the cornea, and corresponded to the conjunctival attachment to the limbus. The posterior-to-anterior (frontal view) orbit X-ray was taken as per the technique described by Itsykson (using the grating), which allowed for control of the eye and limbus marker for correct position during roentgenography. In lateral or axial view, the shadow of ring-shaped limbus marker appeared as a straight line, and in a PA view, it appeared as a ring. Orbit X-ray was performed, quality of X-ray films was assessed and IOFB position in the eye was calculated using the technique of Comberg-Baltin or Abalikhin-Pivovarov. In order to determine the projection of the anteroposterior axis of the eye, the measurement scheme was put on the PA X-ray film so to get the limbus marker shadow inside the relevant circle of the scheme. Thereafter, the needle was used to puncture the PA X-ray film through the measurement scheme and at the intersection of horizontal and vertical meridians. This puncture point at the X-ray film corresponded to the projection of the antero-posterior axis of the eye. Ring-shaped limbus markers with external diameters of 11 and 12 mm were utilized in 10 cases and 2 cases, respectively, in the presence of limbal conjunctival hypertrophy. Results In 12 patients, IOFB was successfully removed based on the data obtained from X-ray localization by means of the ring-shaped limbus marker. In two patients without limbal conjunctival hypertrophy, foreign body X-ray (PA view and lateral view) localization was performed by means of the Baltin’s prosthesis. Thereafter, these two received a paralimbal subconjunctival injection of 0.9% NaCl, and foreign body X-ray localization was performed by means of the ring-shaped limbus marker. Calculations for X-ray (PA view) localization by means of the Baltin’s prosthesis were in agreement with those for X-ray (PA view) localization by means of the ring-shaped limbus marker. In addition, with regard to the X-ray lateral view and X-ray axial view, the position of the IOFB relative to the ring-shaped limbus marker was 1 mm deeper than that relative to the Baltin’s prosthesis due to the location of the limbal circle in the eye. Figs 2 and 3 present X-ray films (frontal projection, a; and lateral projection, b) of the orbit and ring-shaped limbus marker taken on two patients. Example Case 1 A 43-year-old man sustained injuries from a battery explosion. At admission to the trauma centre, he was diagnosed with Poliak grade 1-2 chemical (battery acid) burn to face, conjunctiva and cornea, and a suspected foreign body in the left eye. OD: His right eye was normal. OS: His uncorrected visual acuity in the left eye was 0.1. There was photophobia and subconjunctival hemorrhage, and the bulbar conjunctivae showed a marked collar of edema at the limbus. A 2-3-mm conjunctival wound was found 5 mm from the limbus at the 8 o’clock meridian. The left eye showed subtotal corneal erosion and edema. The left anterior chamber was of moderate depth. The pupil was round and reactive to light. A pink fundus reflex was observed. Fundus structures were poorly seen. The intraocular pressure (IOP) was normal. A shadow of metal IOFB measuring 1х1х2 mm was seen in X-ray films (frontal projection and lateral projection) of the orbit and limbal circle. In the frontal view of orbital X-ray with the ring-shaped limbus marker, the IOFB was seen along the 8:40 o’clock meridian, 9-11 cm from the sagittal axis of the eye, and 1.5-3 mm beneath the horizontal meridian of the eye. In the lateral view of orbital X-ray with the ring-shaped limbus marker, the IOFB was seen 1.5-4 mm posterior to the conjunctival attachment to the limbus, and 1.5-3 mm beneath the horizontal meridian of the eye. The sagittal axis of the eye was 24 mm long. That is, the IOFB was along the 8:40 o’clock meridian, 1.5-4 mm posterior to the conjunctival attachment to the limbus, and 9-11 mm from the sagittal axis of the eye, i.e., within the scleral subconjunctival hemorrhage region. Example Case 2 A 44-year-old man sustained a left-eye injury due to a power lawnmower. At admission, he was diagnosed with the penetrating sclera wound, vitreous hemorrhage and IOFB in the left eye. OD: His right eye was normal. OS: Visual acuity was light perception with inaccurate projection of rays OS. The corneal and sclera wound was linear and vertical, 9-10 mm in length at 2 mm from the limbus at the 3 o’clock meridian; it was seen between 4-5 mm above and 4-5 mm beneath the horizontal meridian. There was scleral subconjunctival hemorrhage around the limbus. The anterior chamber was filled with blood. The IOP estimated by palpation was significantly decreased. In the frontal view and lateral view of orbital X-ray with the ring-shaped limbus marker, the shadow of IOFB measuring 4х7.5х21 mm was seen in the inferior lateral quadrant of the orbit, 3-20 mm from the sagittal axis of the eye, and 20-30 mm posterior to the conjunctival attachment to the limbus, i.e., within the posterior pole wound. In addition, a 2-3-mm portion of the IOFB was situated in the vitreous, and the rest portion extended beyond the eye to the orbit.
Conclusion The ring-shaped limbus marker provides adequate marking of the limbus in frontal, lateral and axial views for X-ray localization of foreign bodies in the presence of apparent chemosis or scleral subconjunctival hemorrhage around the limbus. The marker of the appropriate size adheres well to the eye and remains well fit in the specified position. In addition, it creates a shadow in the lateral and axial view X-ray films which corresponds to the conjunctival attachment to the limbus. Moreover, the distance between the marker shadow and the IOFB shadow can be considered equal to that between the conjunctival attachment to the limbus and the IOFB. Quality of X-ray films was assessed and IOFB position in the eye was calculated using the technique of Comberg-Baltin or Abalikhin-Pivovarov. The ring-shaped limbus marker can be employed during X-ray examination of the orbit in eyes of different sizes and in eye wounds without causing the ocular coats to drop out of the eye along the limbus. References 1.Gundorova RA, Stepanov AV, Kurbanova NF. [Contemporaty ocular traumatology]. Moscow: Meditsina; 2007. Russian. 2.Gundorova RA, Neroev VV, Kashnikov VV, editors. [Ocular injuries]. Moscow: GEOTAR-Media; 2009. p. 90-91. Russian. 3.Baltin MM. [X-ray diagnostics and therapy in ophthalmology]. Moscow: Medgiz; 1951. Russian. 4.Vainstein ES. [Basic X-ray diagnostics in ophthalmology]. Moscow: Meditsina; 1967. Russian. 5.Poliak BL. [Military field ophthalmology: A tutorial for ophthalmologists]. Leningrad: Medgiz; 1957. Russian. 6.Poliak BL. [Injuries to the eye]. Moscow: Meditsina; 1972. Russian. 7.Danilichev VF, editor. [Contemporaty ophthalmology]. St Petersburg: Piter; 2000. Russian. 8.Belkin M. А retention modification for the limbal ring method of foreign body localization. Am J Ophthalmol. 1979 Jul;88(1):124-5. 9.Ross JA. Use of a fine metal ring in the localisation of intra-ocular foreign bodies. Br J Ophthlmol. 1945 Oct;29(10):545. 10.Stallard HB. War Surgery of the Eye. Br Med J. 1942 Nov 28;2(4273):629-31. 11.Gardona H, Trokel SL. Soft vacuum lens for foreign body localization. Am J Ophthalmol. 1972 Aug; 74(2):296-8.
The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|