J.ophthalmol.(Ukraine).2020;2:45-49.
|
http://doi.org/10.31288/oftalmolzh202024549 Received: 24 February 2020; Published on-line: 30 April 2020 Visualization of anterior eye structures by near-infrared transillumination in patients with contusions of the globe M.B. Kogan, Ophthalmologist, Post-graduate Student SI "Filatov Institute of Eye Diseases and Tissue Therapy of the National Academy of Medical Sciences of Ukraine"; Odesa (Ukraine) E-mail: mihailkogan2@gmail.com TO CITE THIS ARTICLE: Kogan MB. Visualization of anterior eye structures by near-infrared transillumination in patients with contusions of the globe. J.ophthalmol.(Ukraine).2020;2:45-49. http://doi.org/10.31288/oftalmolzh202024549
Background: Contusion of the globe is an injury resulting from a blunt object. Despite advances in imaging techniques, the detection of the pathology in contusion of the eye is still a challenge for the ophthalmologist. Purpose: To assess visualization of anterior eye structures by near-infrared transpalpebral transillumination (NIR TPT) in patients with contusions of the globe. Material and Methods: Twenty-five patients with a moderate or severe uniocular contusion who presented 2 to 15 days after the traumatic event were under observation. The fellow eye was intact in all cases. Patients underwent visual acuity assessment; biomicroscopy; ophthalmoscopy; intraocular pressure (IOP) measurements; ultrasound scanning of the anterior eye and posterior eye; ultrasound distant perimetry; X-ray examination; color photography and NIR TPT. Results: NIR TPT enabled identifying various types of damage to the iris, lens and sclera, including subconjunctival scleral ruptures. Pars plicata width was larger in affected eyes than in intact fellow eyes. Conclusion: NIR TPT enables non-invasive visualization of various types of damage to the anterior eye like iridodialysis in the iris root area, tears of the pupillary margin, lenticular opacity, subluxated lens and subconjunctival scleral ruptures in patients with contusion of the globe. In addition, for these study patients, pars plicata width was larger in affected eyes than in intact fellow eyes. Keywords: contusion of the globe, ciliary body, near-infrared transillumination
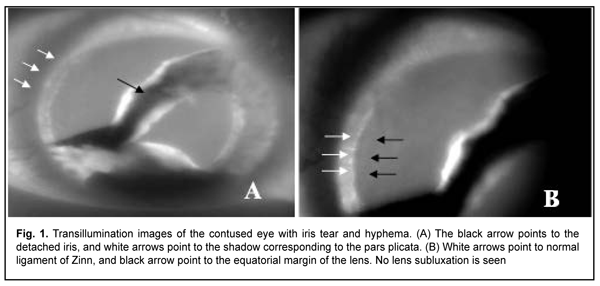
Introduction Ocular trauma is one of the commonest causes of monocular blindness [1]. Contusion of the globe is a globe injury resulting from a blunt object [2], and is seen predominantly in working-age males [3]. The diversity of post-contusion conditions can be explained by the impact force and direction, as well as by the anatomical structure of the eye [2]. Blunt ocular trauma is frequently associated with injury to the lens and anterior segment hemorrhage and inflammation, and sometimes with loss of integrity of the intraocular structures (the choroid and sclera) [1, 2]. It is noteworthy that contact imaging techniques (like ultrasonography) are not advisable in patients with suspected subconjunctival scleral rupture due to the risk of expulsive iatrogenic hemorrhages during such imaging procedures [4]. Despite advances in imaging techniques, the detection of the pathology in contusion of the eye is still a challenge for the ophthalmologist. It has been demonstrated previously that transpalpebral near-infrared transpalpebral transillumination (NIR TPT) enables visualizing, localizing and assessing the size of scleral shadows of ciliary body structures [5,6]. In addition, in patients with penetrating globe injury, the technique enables visualizing infrared shadows cast by intraocular foreign bodies (IOFB; such as metal, stone or wood) located in the scleral projection of the ciliary body structures, which improves the potential for making the preoperative diagnosis [6, 7]. As the near-infrared light penetrates human tissues better than the visible light used in biomicroscopy [8], we believe it is reasonable to use the near-infrared light for assessing changes in the anterior eye structures in post-contusion conditions. The purpose of the study was to assess visualization of anterior eye structures by NIR TPT in patients with contusions of the globe. Materials and Methods This was a pilot, open-label, prospective cross-over study. The study was conducted to perform the planned research (state registration number 0119U101215), and the protocol was approved by the Bioethics Committee of the Filatov Institute. All study subjects signed informed consent. The potential of NIR TPT for identifying damage to intraocular structures in mild or severe contusion was assessed. Twenty-five patients (50 eyes; age, 30 years to 57 years) with a uniocular contusion who presented 2 to 15 days after the traumatic event were under observation. The fellow eye was intact in all cases. Patients underwent visual acuity assessment; biomicroscopy; ophthalmoscopy; intraocular pressure (IOP) measurements; ultrasound scanning of the anterior eye and posterior eye; ultrasound distant perimetry; X-ray examination; and color photography. Patients with suspected subconjunctival scleral rupture were not subject to any contact imaging procedure. In addition, all patients underwent NIR TPT. The NIR TPT system used consisted of (1) a wireless infrared light-emitting-diode light source with a dominant wavelength of 940 nm, and (2) slit-lamp attachable monochrome video camera (Blackfly®, FLIR Integrated Imaging Solutions Inc., Canada) capable of recording NIR images and video [6]. Since we used the transpalpebral illumination pathway, the study was conducted without the use of topical anesthetics. The transpalpebral illumination study was performed with the patient sitting at the slit lamp. Images of the scleral projection of the pars plicata and pars plana limited by the ora serrata were taken for both eyes. The intraocular damage found by NIR TPT was compared with that found by conventional techniques such as biomicroscopy, ophthalmoscopy, and ultrasound scanning of the anterior eye and posterior eye. The width of ciliary body structures was measured for both eyes in 23 patients (46 eyes), but not in patients with subconjunctival scleral rupture. These NIR TPT-based width measurements for ciliary body structures were made at four meridians: 12 o’clock, 6 o’clock, 3 o'clock and 9 o'clock. The widths of the shadows of ciliary body structures were measured with calipers. Epibulbar anesthesia with ophthalmic 0.5% proparacaine hydrochloride was used in both eyes for performing this procedure. Statistical analysis was performed using STATISTICA 10 software (StatSoft, Inc.). Group means and standard deviations (SD) were calculated for all variables. The level of significance p ? 0.05 was assumed. Results Incidence and types of eye damage found by conventional imaging techniques included: hyphema, tears of the pupillary margin, posttraumatic mydriasis, and iridodialysis in 1st or 2nd quadrants in 7 patients (28%), subluxated lens in 11 patients (44%), lens luxated into the vitreous in 5 patients (20%), and anterior subconjunctival scleral rupture in 2 patients (8%). In study patients with contusion of the eye, NIR TPT was performed in an easy and non-invasive way, and enabled identifying above types of damage to the iris and lens. E.g., iridodialysis in the iris root area, tears of the pupillary margin, lenticular opacity and subluxated lens were well visualized in all cases (Fig. 1).
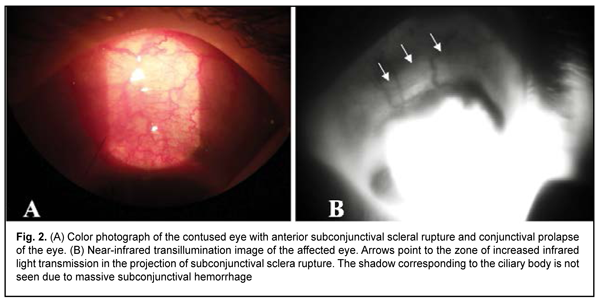
In addition, NIR TPT enabled identifying subconjunctival scleral rupture in the form of increased infrared light transmission in the projection of the rupture in two patients with contusion of the eye (Fig. 2). It is noteworthy that conventional imaging techniques showed indirect signs of anterior scleral rupture (hypotony, conjunctival chemosis, deep anterior chamber, and vitreous hemorrhage). This was followed by surgical revision of the sclera with identification and repair of the scleral rupture.
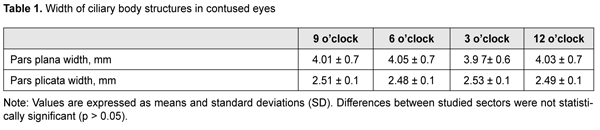
The axial length ranged from 23 mm to 24.7 mm. Mean width of the pars plicata was significantly wider in affected eyes than in intact fellow eyes (2.5 ± 0.1 mm vs 0.5 ± 0.1 mm, p = 0.01). There was no significant difference in size of ciliary body structures between the zones of the ciliary body. Table 1 presents the width of ciliary body structures in study zones.
Discussion Applications of visible light transillumination for identifying ciliary body outline or anterior ocular tumors have been known for years. This approach has been also used for accurate placement of radioactive plaques in brachytherapy of choroidal melanoma [9, 10]. A traumatic transcorneal or transscleral illumination pathway should be used to perform visible-light transillumination of the globe. A number of authors pointed to the advantages of using the infrared light for transillumination [8, 11, 12]. For example, the near-infrared light is known to penetrate human tissues better than the visible light. The use of near-infrared LED illumination in NIR TPT enables transillumination not only through the cornea and sclera, but even through the patient’s lid, which provides a number of advantages. Compared to ultrasound, NIR TPT is more comfortable and safe for the patient, and requires no use of topical anesthesia. With the use of near-infrared light for globe transillumination, there is no glare from bright visible light, because the near infrared light is invisible for the human eye; this makes the conduct of NIR TPT studies in patients with posttraumatic eye disorders easier. In addition, absence of physical contact between LED light source and the cornea and sclera allows excluding complications and trauma of these ocular structures, which is especially important in traumatic eye injuries. We managed to conduct NIR TPT diagnostic procedures quickly and safely with as little pain and discomfort to the patient as possible in all cases of the study [6, 13]. Subconjunctival scleral rupture is a globe pathology that is difficult to diagnose. The major signs of this disorder are low IOP, conjunctival chemosis, deep anterior chamber, and vitreous hemorrhage, which might not be apparent early after the traumatic event [4, 14, 15]. Surgical revision of the sclera for identification of the scleral rupture (if any) is recommended in eyes suspected for this pathology [2]. It should be noted that, in patients with scleral rupture, contact imaging studies are associated with the risk of prolapse of the retina, choroid and vitreous resulting from probe contact with the globe [4]. In the current study, using NIR TPT, we managed to detect various types of posttraumatic damage in the anterior eye in all patients with contusion of the globe. In particular, we managed to identify subconjunctival scleral rupture due to increased infrared light transmission in the projection of the rupture. Using NIR TPT, we identified not only the types of lens or iris damage easily detectable with the slit lamp, but also those that are difficult to diagnose. For example, we managed to visualize damage to anterior eye structures in eyes with opaque optic media (e.g., corneal clouding). This can be explained by the fact that the infrared light has better penetration compared to the visible light. It should be noted that, in patients with subconjunctival hemorrhage, a thin blood layer did not prevent near-infrared visualization of the intraocular structures. A massive subconjunctival hemorrhage, however, can hamper visualization of these structures. Thus, in the current study, we failed to visualize the shadow of pars plicata and pars plana in any quadrants in two patients due to a shielding effect of blood with respect to the near-infrared light. Morphometric characteristics of the choroid are known to depend on the size of the eye. Thus, OCT-measured subfoveal choroidal thickness has been found to decrease with an increase in axial length [16]. A relationship between dimensions of ciliary body structures and axial length has been also reported [5, 17, 18]. The results of measurements of ciliary body structures in intact fellow eyes in this study are in agreement with the previous findings, taking into account axial length values [5]. In the present study, width of the pars plicata was wider in affected eyes than in intact fellow eyes for all patients, which we believe could be explained by the presence of contusion-induced traumatic ciliary edema. Conclusion In patients with contusion of the globe, NIR TPT enables non-invasive visualization of various types of damage to the anterior eye (like iridodialysis in the iris root area, tears of the pupillary margin, lenticular opacity, subluxated lens and subconjunctival scleral rupture) due to variations in absorption and transmission of the near-infrared light by these structures. Pars plicata width was larger in affected eyes than in intact fellow eyes for all study patients with contusion of the globe, which could be explained by the presence of contusion-induced traumatic ciliary edema.
References 1.Erikitola OO, Shahid SM, Waqar S, Hewick SA. Ocular trauma: classification, management and prognosis. Brit J Hosp Med. 2013;74:108-11. 2.Yucel O, Demir S, Niyaz L. Clinical characteristics and prognostic factors of scleral rupture due to blunt ocular trauma. Eye. 2016;30:1606–13. 3.Maiya AS, Dharmesh AM, Jayaram RJ. Clinical profile of ocular blunt trauma in a rural hospital. Clin Ophthalmol Res. 2018;6:3-7. 4.Navon SE. Management of the ruptured globe. Int Ophthalmol Clin. 1995;35:71-91. 5.Zadorozhnyy O, Alibet Yassine, Kryvoruchko A, Levytska G, Pasyechnikova N. Dimensions of ciliary body structures in various axial lengths in patients with rhegmatogenous retinal detachment. J Ophthalmol (Ukraine). 2017;6:32-6. 6.Kogan MB, Zadorozhnyy OS, Petretska OS, Krasnovid TA, Korol AR, Pasyechnikova NV. Visualization of intraocular foreign bodies in the projection of the ciliary body by transpalpebral near-infrared transillumination. J Ophthalmol (Ukraine). 2019;4:23-27. 7.Pasyechnikova N, Naumenko V, Korol A, Zadorozhnyy O. Digital imaging of the fundus with long-wave illumination. Klinika oczna. 2009;111(1-3):18-20. 8.Krohn J, Ulltang E, Kjersem B. Near-infrared transillumination photography of intraocular tumours. Br J Ophthalmol. 2013;97:1244-6. 9.Krohn J, Seland JH, Monge OR. Transillumination for accurate placement of radioactive plaques in brachytherapy of choroidal melanoma. Am J Ophthalmol. 2001;132:418-9. 10.Thomson ES. The Sachs lamp for transillumination of the eye. Trans Am Ophthalmol Soc. 1905;10:456–60. 11.Saari M, Nieminen H. Fluorescein angiography and infra-red transilluminationstereo technique for studying the ciliary body and iris.In: Proceedings of the 5th Congress of the European Society of Ophthalmology; April 5–9, 1976; Hamburg, Germany. 12.Saari M, Vuorre I, Nieminen H. Infrared transillumination stereophotography of normal iris. Can J Ophthalmol. 1977;12:308–11. 13.Zadorozhnyy O, Korol A, Nevska A, Kustryn T, Pasyechnikova N. Ciliary body imaging with transpalpebral near-infrared transillumination – a pilot study. Klin oczna. 2016;3:184-6. 14.Cherry PM. Indirect traumatic rupture of the globe. Arch Ophthalmol. 1978;96:252-6. 15.Weissman JL, Beatty RL, Hirsch WL, Curtin HD. Enlarged anterior chamber: CT finding of a ruptured globe. AJNR Am J Neuroradiol. 1995;16(4):936-8. 16.Wei WB, Xu L, Jonas JB, et al. Subfoveal choroidal thickness: the Beijing Eye Study. Ophthalmology. 2013;120:175–80. 17.Hairston RJ, Maguire AM, Vitale S. Morphometric analysis of pars plana development in humans. Retina. 1997;17(2):135-8. 18.Oliveira C, Tello C, Liebmann JM. Ciliary body thickness increases with increasing axial myopia. Am J Ophthalmol. 2005;140(2):324-5.
The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|