J.ophthalmol.(Ukraine).2020;2:30-35.
|
http://doi.org/10.31288/oftalmolzh202023035 Received: 21 January 2020; Published on-line: 30 April 2020 Optimizing the treatment for dry eye syndrome in patients with allergic conjunctivitis F.A. Bakhritdinova,1 Dr Sc (Med), Prof.; S.A. Mirrakhimova,2 Dr Sc (Med), Ass. Prof.; K.I. Narzikulova,1 Dr Sc (Med), Ass. Prof.; Zh.O. Safarov, 2 Assistant; O.I. Oripov,1 Assistant 1 Ophthalmology Department, Tashkent Medical Academy; Tashkent (Uzbekistan) 2 Eye Disease Department, Samarkand State Medical Institute; Samarkand (Uzbekistan) E-mail: okil.oripov@mail.ru TO CITE THIS ARTICLE: Bakhritdinova FA, Mirrakhimova SA, Narzikulova KI, Safarov ZhO, Oripov OI. Optimizing the treatment for dry eye syndrome in patients with allergic conjunctivitis. J.ophthalmol.(Ukraine).2020;2:30-35. http://doi.org/10.31288/oftalmolzh202023035
Background: Allergic conjunctivitis is commonly complicated by secondary dry eye syndrome that substantially affects the quality of life of patients and requires a comprehensive approach to treatment. Purpose: To improve treatment of dry eye patients with allergic conjunctivitis through the use of artificial tears. Material and Methods: Fifty-six patients with acute allergic conjunctivitis complicated by secondary dry eye syndrome were included in the study. The main group, but not the control group, received artificial tears as adjunct to basic therapy. A comprehensive analysis included a study of clinical symptoms, status of the tear complex and meibomian glands. Results: In addition to improvements in scores of subjective symptom questionnaire, and Schirmer test and tear film break up time (TFBUT) measurements, more apparent improvements in signs of disease were found in patients who received artificial tears as an adjunct to basic therapy beginning from day 10. The most severe meibographic evidence of morphological defects in gland ducts was seen in the papillary and follicular forms of conjunctivitis. Conclusion: Comprehensive therapy with introduction of artificial tears as an adjunct at day 10 of basic treatment is a reasonable and pathogenetically substantiated corrective treatment for poor tear film function in the acute phase of allergic conjunctivitis. Keywords: allergic conjunctivitis, dry eye syndrome, tear substitute therapy, meibography
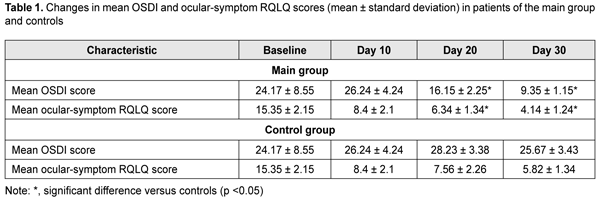
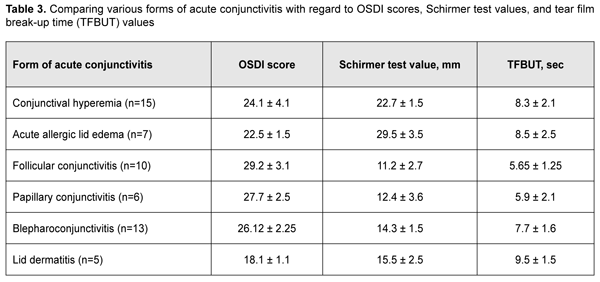
Introduction Management of allergic eye disorders is an important medical and social issue, since the rates of allergic disorders are rising, especially in the developed countries and countries with poor environmental conditions. The prevalence of allergic conjunctivitis (AK) varies worldwide, ranging 20% to 30% in general population, and approaching 40% in pediatric population [1, 2]. Abnormal tear formation in the form of tear hypersecretion or hyposecretion is a major clinical aspect of allergic conjunctivitis. The tissue edema that accompanies allergic reactions locally affects conjunctival glands and plays a key role in the pathogenesis of abnormal tear formation [3, 4, 5, 6]. Previous studies have demonstrated that innervation of the auxiliary lacrimal glands and conjunctival goblet cells takes the same route as innervation of the conjunctiva [7,8]. Qualitative and quantitative tear film abnormalities include changes in the ocular surface, main lacrimal gland, and their neuroreflexive relationships [9]. This set of abnormalities is defined by the term secondary dry eye syndrome (SDES) [10]. In this connection, management of allergic conjunctivitis is a set of measures aimed at relieving and preventing allergic inflammation and its consequences with pharmacological and non-pharmacological treatments. The use of any agents should, however, be justified, since only a comprehensive approach to management of patients with allergic diseases will provide the best therapeutic effect. The purpose of the study was to improve treatment of dry eye patients with allergic conjunctivitis through the use of artificial tears. Material and Methods Fifty-six patients (112 eyes; 26 men and 32 women; age, 18 years to 60 years) with acute allergic conjunctivitis were included in the study. Patients were divided into the following groups based on the clinical form of the allergic lesion and using the Maichuk’s classification scheme [5]: conjunctival hyperemia (15 patients), acute allergic lid edema (7 patients), follicular conjunctivitis (10 patients), papillary conjunctivitis (6 patients), blepharoconjunctivitis (13 patients), and lid dermatitis (5 patients). All patients received topical desensitizing therapy including Kromoviz, 4% ocular sodium cromoglycate (ASEPTICA Ltd, Tashkent, Uzbekistan), 2 drops four times daily for 4 weeks. This treatment resulted in some decrease in clinical signs and subjective symptoms of the disease. Beginning from day 10 of this treatment, patients were divided into two clinically homogeneous groups (the main group and the control group) of 28 patients each to receive either Ophthalron, sodium hyaluronate (ASEPTICA Ltd), 2 drops three times daily for 20 days as an adjunct to topical Kromoviz therapy, or topical Kromoviz therapy only using the initial therapeutic regimen, respectively. At baseline and at each 10-day interval, patients were asked to complete questionnaires to identify subjective symptoms of AK and SDES. The second category of the modified Rhinoconjunctivitis Quality of Life Questionnaire [11, 12] aims to assessing the intensity of ocular symptoms (eye itching, tearing, irritation and fatigue); the responders rated each item of this category using a 5-point Likert scale, and these ratings were used to subjectively assess symptoms of AK. The diagnosis of dry eye syndrome was based on responders’ answers to questions of the Ocular Surface Disease Index (OSDI) questionnaire [6] that was adapted and translated into Uzbek language by the authors of the current study. Patients underwent a comprehensive eye examination including Schirmer test and tear film break up time (TFBUT) measurements. The automatic refractor/ keratometer HRK-9000A (Huvitz, South Korea) was used to perform TFBUT measurements and meibography. Fluorescein Sodium Ophthalmic Strips (Fluoro Touch; Madhu Instruments, India) were also utilized in TFBUT measurements. Microsoft Excel software was used for statistical analysis, and mean values, standard deviations, and standard errors of the mean were calculated. The Student test was used to assess significance. Differences in mean values for independent variables or related paired series were considered significant at 95% confidence intervals. Results At baseline, mean OSDI and mean ocular-symptom RQLQ scores of study patients were 24.17 ± 8.55 and 15.35 ± 2.15, respectively, and corresponded to moderate disease. At day 10 of Kromoviz monotherapy, mean ocular-symptom RQLQ score decreased to 8.4±2.1, and mean OSDI score was 26.24±4.24 for 56 patients. At later time points, statistics were calculated separately for the groups. At days 20 and 30, mean RQLQ score for the control group decreased to 7.56 ± 2.26 and 5.82 ± 1.34, respectively. In addition, mean OSDI score for the control group was maximum (28.23±3.38) at day 20 and 25.67±3.43 at day 30. Mean RQLQ score for the main group decreased to 6.34 ± 1.34 and 4.14 ± 1.24 at days 20 and 30, respectively. Mean OSDI score for the main group decreased to 16.15±2.25 at day 20 and 9.35±1.15 at day 30 (Table 1).
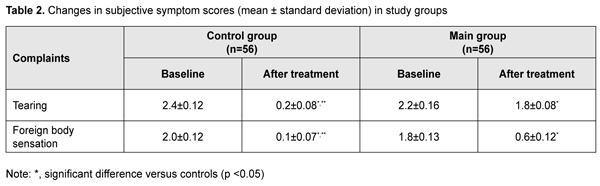
By day 10 of Kromoviz therapy, such symptoms as eye itching, hyperemia and burning sensation, and mucous discharge relieved completely, and allergic inflammation score was as low as 0. By that time, however, there was still some tearing and some foreign body sensation in the eyes. Before administration of tear substitutе therapy, mean tearing score and mean foreign body sensation score for the groups were 2.3±0.14 and 1.9±0.11, respectively. We found decreased tearing in eyes receiving tear substitutе therapy as early as day 3 of treatment, with a mean tearing score of 1.9 ± 0.06 (p < 0.05), which was 1.2-fold lower than baseline. At day 10, tearing relieved in almost all patients, with a mean tearing score of 0.2 ± 0.08 (p < 0.05). In the group of patients not treated with tear substitutе therapy, however, a decrease in tearing was observed only at day 10, with a mean tearing score of 1.8 ± 0.08, which was significantly (p < 0.05) lower than baseline. In the main group, a decrease in foreign body sensation was observed at day 2 or day 3 of tear substitutе therapy, with a mean foreign body sensation score of 1.2 ± 0.04 (p < 0.05). By day 10, patients of this group reported a substantial improvement in their eye conditions, with a mean foreign body sensation score of 0.1 ± 0.07 (p < 0.05), whereas patients of the control group still reported foreign body sensation, although the mean score decreased to 0.6±0.12 (Table 2).
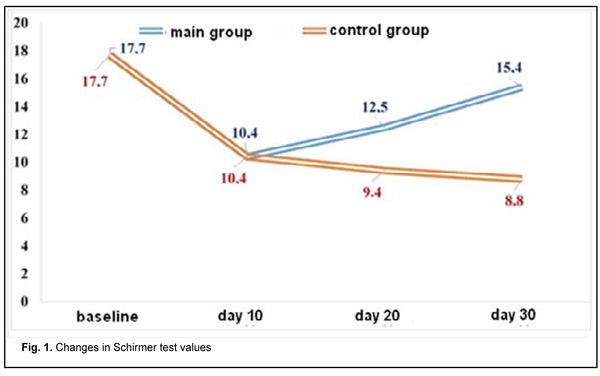
Therefore, inclusion of tear substitutе therapy into the comprehensive treatment of allergic eye produced an almost two-fold decrease in the time to dry eye symptom relief, resulting in faster recovery. The results of the Schirmer test showed that tear hypersecretion was common for patients with acute conjunctivitis. Mean Schirmer test value for all 56 patients decreased from 17.7±2.3 mm at baseline to 10.4±1.4 mm by day 10. By day 30, mean Schirmer test value for the control group decreased to 8.8±1.6 mm, and for the main group, to 15.4±1.6 mm (Fig. 1).
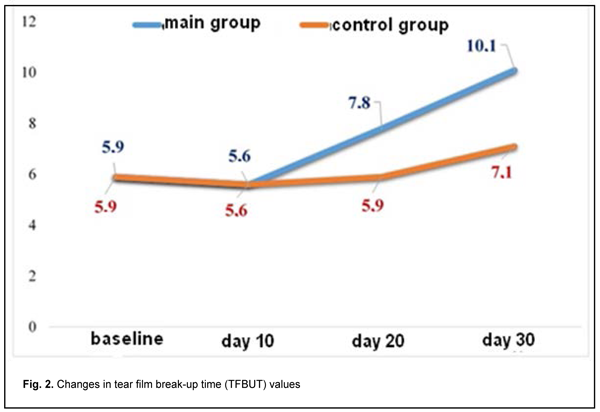
In addition, mean TFBUT test value for all 56 patients decreased from 5.9±2.1 s at baseline to 5.6±1.1 s by day 10. Subsequently, inclusion of artificial tears into the comprehensive topical treatment of patients of the main group resulted in tear film stabilization and increases in mean TFBUT test value to 7.8±2.3 s and 10.1±1.7 s at days 20 and 30, respectively. In the control group, mean TFBUT test value at the end of the study was 7.1 ± 2.5 s, which was lower than the norm, and indicated impaired tear film stability (Fig. 2).
Secondary dry eye syndrome as assessed by OSDI, Schirmer test and TFBUT test was more severe in follicular conjunctivitis, papillary conjunctivitis, and blepharoconjunctivitis, compared to acute edema, lid dermatitis and conjunctival hyperemia (Table 3).
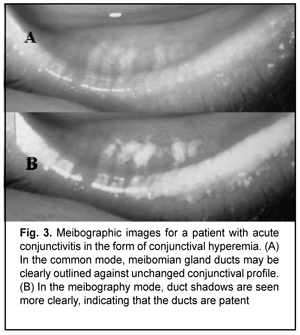
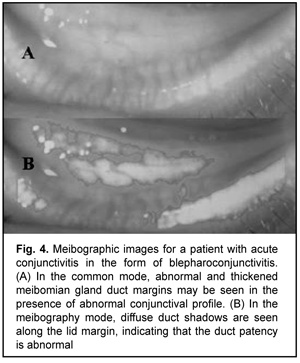
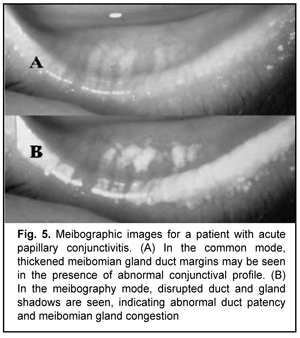
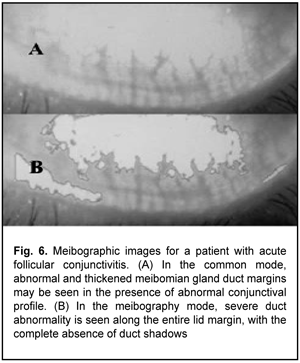
Meibography showed (Figs. 3-6) most severe changes in meibomian gland ducts in patients with follicular allergic conjunctivitis or allergic blepharoconjunctivitis. In eyes with follicular allergic conjunctivitis, meibography showed obliteration of almost all meibomian gland ducts, which resulted in severely impaired tear film stability as assessed by the TFBUT test and more severe symptoms as assessed by the OSDI. There was no apparent meibographic evidence of conjunctival defects in meibomian gland ducts in mild allergic conjunctivitis in the form of conjunctival hyperemia.
Discussion In the current study, the analysis of the obtained data provided evidence that the severity of subjective symptoms of allergic conjunctivitis reflected a decrease in major disease manifestations during the course of topical basic therapy with the mast cell membrane stabilizer. The mean ocular-symptom RQLQ score at baseline corresponded to moderate allergic conjunctivitis. As early as 10 days of treatment, the score decreased almost 50%, providing evidence of a prompt increase in effect of pathogenetic therapy for the disease. In addition, the results of OSDI and objective Schirmer test and TFBUT test measurements demonstrated that signs of secondary dry eye syndrome were observed also in the acute stage of conjunctivitis, providing evidence of long-term abnormalities. The analysis of tear secretion in the course of treatment showed that cycles in changes of tear secretion were common in the acute stage of conjunctivitis. Hypersecretion was common at baseline, and was subsequently changed by hyposecretion associated with decreased function of tear glands and effect of desensitizing medication. The subsequent use of artificial tears in the comprehensive treatment allowed for normalizing tear secretion, which was associated with restoration of tear film stability in patients of the main group. The comparative analysis of manifestations of secondary dry eye syndrome in various forms of acute conjunctivitis demonstrated that the syndrome was most severe in allergic blepharoconjunctivitis, follicular conjunctivitis and papillary conjunctivitis, which is explained by the developing morphological changes in the conjunctiva and meibomian glands [13, 14, 15]. The results of meibography confirmed that, in severe forms of allergic conjunctivitis (blepharoconjunctivitis, follicular and papillary conjunctivitis), severe morphological abnormalities develop, leading to poor lipid outflow from the meibomian glands and obliteration of meibomian gland ducts [15]. TFBUT data and intensity of subjective symptoms were in concordance with the results of meibography, which indicated that decreased lipid secretion substantially affects the development of tear film dysfunction and secondary dry eye syndrome in allergic conjunctivitis. Conclusion First, clinical manifestations of secondary dry eye syndrome were found to be concomitant with major symptoms of allergic conjunctivitis and aggravate its course, which was confirmed by the results of meibography, TFBUT, OSDI and RQLQ data. Second, comprehensive therapy with introduction of artificial tears as an adjunct at day 10 of basic treatment is a reasonable and pathogenetically substantiated corrective treatment for poor tear film function in the acute phase of allergic conjunctivitis. Finally, the most severe symptoms of secondary dry eye syndrome were observed in allergic blepharoconjunctivitis, allergic follicular conjunctivitis and allergic papillary conjunctivitis, in which severe morphofunctional abnormalities of meibomian gland ducts developed, contributing to progression of secondary dry eye syndrome.
References 1.Brzheskiy VV. [On the prevalence of vernal keratoconjunctivitis and current possibilities of treatment]. Russian Ophthalmological Journal. 2017;10(4):74–81. Russian. 2.Brzheskiy VV. [Allergic conjunctivitis: a guide for an outpatient ophthalmologist]. Meditsinskoie oboztrniie. 2018;1(2):74–9. Russian. 3.Majchuk DIu., Chilingarian LB. [Tear replacement therapy for allergic eye conditions]. Oftal'mologiia. 2012; 2:72–6. Russian. 4.Zabegailo AO, Safonova TN, Makarov IA. [A new method to determine the severity of the blepharoconjunctival form of the dry eye syndrome]. Kataraktal'naia i refraktcionnaia khirurgiia. 2013;13(1):35–8. Russian. 5.Maichuk IuF, Mironkova EA. [Classification of meibomian gland dysfunction combined with dry eye syndrome and pathogenetic approaches to complex therapy]. Klinicheskaia oftal'mologiia. 2007;8(4):169–72. Russian. 6.Nebbioso M, Fameli V, Gharbiya M, Sacchetti M, Zicari AM, Lambiase A. Investigational drugs in dry eye disease. Expert Opin Investig Drugs. 2016;25(12): 1437–46. 7.Trubilin VN, Polunina EG, Markova EIu, Andzhelova DV, Kurenkova SV. [Methods of screening diagnosis of meibomian gland dysfunction]. Oftal'mologiia. 2016;13(4):235–40. Russian. 8.Fogt JS, Kowalski MJ, King-Smith PE, et al. Tear lipid layer thickness with eye drops in meibomian gland dysfunction. Clin Ophthalmol. 2016 Nov7;10:2237–43. 9.Tomlinson A, Bron AJ, Korb DR, et al. The international workshop on meibomian gland dysfunction: report of the diagnosis subcommittee. Invest Ophthalmol Vis Sci. 2011 Mar 30;52(4):1994-2005. 10.Zhao Y, Veerappan A, Yeo S, et al. Clinical Trial of Thermal Pulsation (LipiFlow) in Meibomian Gland Dysfunction With Preteatment Meibography. Eye Contact Lens. 2016 Nov;42(6):339–46. 11.R?tzer V, Egu D, Waschke J. Meibomian gland cells display a differentiation-dependent composition of desmosomes. Histochem Cell Biol. 2016 Dec;146(6):685-694. 12.Hom MM, Nguyen AL, Bielory L. Allergic conjunctivitis and dry eye syndrome. Ann Allergy Asthma Immunol. 2012 Mar;108(3):163-6. 13.Nichols KK, Foulks GN, Bron AJ, et al. The International Workshop on Meibomian Gland Dysfunction: Executive Summary. Invest Ophthalmol Vis Sci. 2011 Mar 30;52(4):1922-9. 14.Pult H, Nichols JJ. A Review of Meibography. Optom Vis Sci. 2012 May;89(5):E760-9. 15.Pult H, Riede Pult B.H. Non-contact meibography: keep it simple but effective. Cont Lens Anterior Eye. 2012 Apr;35(2):77-80.
The authors declare no conflict of interest.
|