J.ophthalmol.(Ukraine).2020;2:17-23.
|
http://doi.org/10.31288/oftalmolzh202021723 Received: 31 January 2020; Published on-line: 30 April 2020 Tumor-like corneal limbal lesions K.V. Sereda, Cand Sc (Med); G.I. Drozhzhina, Dr Sc (Med), Prof.; T.B. Gaidamaka, Dr Sc (Med); V.L. Ostashevskii, Cand Sc (Med); V.V. Vit, Dr Sc (Med), Prof Filatov Institute of Eye Diseases and Tissue Therapy, NAMS of Ukraine; Odesa (Ukraine) E-mail: evsereda08@gmail.com TO CITE THIS ARTICLE: Sereda KV, Drozhzhina GI, Gaidamaka TB, Ostashevskii VL, Vit VV. Tumor-like corneal limbal lesions. J.ophthalmol.(Ukraine).2020;2:17-23. http://doi.org/10.31288/oftalmolzh202021723
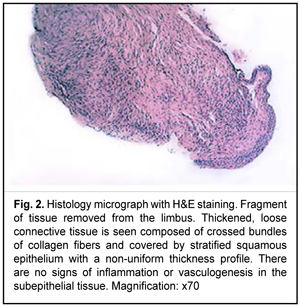
Background: Primary tumors of the cornea and sclera are extremely rare. Most tumors of this region are secondary neoplasms arising from adjacent ocular structures. Benign tumors, namely, conjunctival and/or corneal dermoid tumors and lipodermoids are most common. Purpose: To analyze three cases of tumor-like corneal limbal lesions and to assess treatment outcomes. Material and Methods: Three cases of tumor-like corneal limbal lesions were under our observation. All these were given a preliminarily diagnosis of a dermoid cyst or lipodermoid. Two patients underwent corneal lesion removal and subsequent keratoscleral plasty. In the third case, amniotic membrane was applied to the cornea after corneal lesion removal. Results: The intrasurgically removed tissue was sent for histological examination. The diagnosis of dermoid or lipodermoid was not confirmed in any case. In these three cases, histology showed thickened loose connective tissue composed of crossed bundles of collagen fibers and covered by stratified squamous epithelium with a non-uniform thickness profile, with evidence of mild acanthosis. Loose connective tissue comprised blood vessels and was mildly infiltrated with lymphocytes in one case. Conclusion: Limbal tumor-like lesions require thorough diagnostic evaluation including impression cytology is a must to differentiate benign from malignant epithelial lesions. In addition, the tissue removed during the surgical procedure must be sent to the pathological laboratory for histological verification of diagnosis. Keywords: tumor-like lesions, corneal limbal area, dermoid cyst, lipodermoid, keratoscleral plasty, amniotic membrane
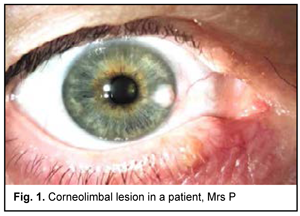
Introduction Primary tumors of the cornea and sclera are extremely rare. Most tumors of this region are secondary neoplasms arising from adjacent ocular structures. Connective tissue tumors (fibroma, proliferative fasciitis), angiomatous tumors (hemangioma), neural tissue tumors (neurofibromatosis), melanocytic tumors (melanoma) may also involve the cornea and sclera [1]. Benign tumors, namely, conjunctival and/or corneal dermoid tumors and lipodermoids are most common [2]. Dermoid cysts are the most common tumors of the orbit [3]. Some authors consider them as choristomas which are defined as the proliferation of normal tissue at an abnormal site [3, 4, 5]. Dermoid cysts are commonly located on the bulbar or tarsal conjunctival surface. Limbal dermoids usually occur at the superior temporal limbsal area, and may involve the cornea [6]. Lipodermoid cysts and solid dermoid tumors consist of adipose tissue covered by connective tissue [7]. Most newly diagnosed cases of dermoids and lipodermoid cysts are individuals aged 15 to 35 years [8]. Symptoms of dermoid cysts vary depending on patient’s age, cyst location, and clinical data, and present as ocular discomfort, foreign body sensation, tearing, redness, ptosis, diplopia, and reduced vision. Advanced cases may cause severe corneal astigmatism [9, 10, 11]. Clinical signs, however, frequently are not supported by histological evidence, which results in the need for detailed examination in cases with epibulbar neoplasms. The purpose of this study was to analyze three cases of tumor-like corneal limbal lesions and to assess treatment outcomes. Material and Methods Three cases of tumor-like corneal limbal lesions (two men of 21 and 52 years of age and a woman of 65 years) were under our observation. All these were given a preliminarily diagnosis of a dermoid cyst or lipodermoid. Two patients underwent corneal lesion removal and subsequent keratoscleral plasty. In the third case, amniotic membrane was applied to the cornea after corneal lesion removal. The removed tissue was sent for histological examination. Results Case 1 A female patient of 65 years presented to the institute with complaints of periodic redness, foreign body sensation and decreased vision in her right eye. She reported a history of discomfort and periodical redness in the eight eye for 2 months, presumably after her blood pressure rose to 180/100 mmHg. The patient was administered Indocollyre eyedrops as was recommended by her ophthalmologist, but noted no improvement with the treatment. After a two-week increase in foreign body sensation and discomfort in her right eye, the patient applied for care at our institute. At presentation at the Corneal Microsurgery Department, the patient’s uncorrected visual acuity (UCVA) was 0.6 OD and 0.85 OS. The best corrected visual acuity (BCVA) was 0.7 with +1.0 D sphere OD and 1.0 with +1.0 D sphere OS. Biomicroscopy of the right eye revealed a bright tumor-like lesion at the limbus between 3 o’clock and 4 o’clock, local conjunctival hyperemia and full-blood radiating vessels in the right eye. The anterior chamber was of moderate depth and the pupil was mobile. There was mild lens opacity. In the left eye, the cornea was clear and bright, the anterior chamber was of moderate depth, and there was mild lens opacity (Fig. 1).
A sonogram of the right eye showed moderately echogenic substrate measuring 0.75-mm height and 2.7 x 2.5-mm length in the peripheral anterior corneal surface at the 3 o’clock with extension into the limbal conjunctiva. Anterior corneal contour beneath the substrate was slightly molded. No evidence of focal space-occupying pathology was revealed in the ciliary body. Impression cytology showed epithelial hyperplasia without cell atypia. On November 20, 2019, the patient underwent removal of the tumor-like lesion, and the amniotic membrane cryopreserved at 196°С was applied to cover the corneal defect. During the surgical procedure, the tumor-like mass was completely removed intracapsularly within the corneal epithelium. Amniotic membrane was applied as a peripheral transplant and sutured to the epithelial defect margin using interrupted 10-0 nylon sutures. A soft therapeutic contact lens was placed on the corneal surface. The removed tissue was sent for histological examination (Fig. 2).
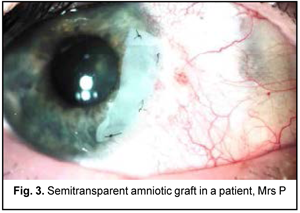
At the time of discharge: the patient’s UCVA was 0.85 OU, and the BCVA was 1.2 with +1.0 D sphere OD and 1.0 with +1.0 D sphere OS. On biomicroscopy of the right eye, the conjunctiva was pink, the soft therapeutic contact lens was seen covering the entire corneal surface and appeared correctly positioned. The peripheral amniotic graft was semitransparent, with well preserved integrity, and was adapted with nylon 10/0 interrupted corneal sutures. The rest of the cornea was transparent. The anterior chamber was of moderate depth and the pupil was mobile. There was mild lens opacity (Fig. 3).
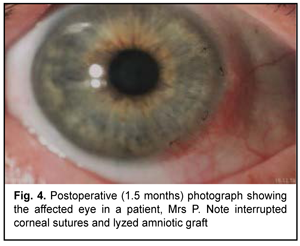
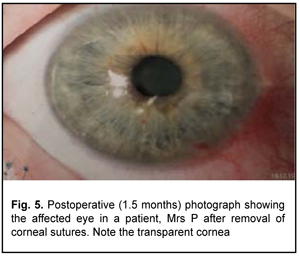
At 1.5 months after surgery, the amniotic graft appeared completely lysed, and the cornea was transparent, epithelized and did not stain with fluorescein (Figs. 4,5).
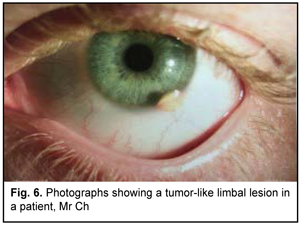
Case 2 A male patient of 21 years presented to the institute with complaints of a 4-month history of a lesion in his left eye. He reported no trauma of the head or the left eye. At presentation, UCVA was 1.0 OU. Biomicroscopy of the left eye revealed a yellowish lesion at the limbus at 5 o'clock position with associated corneal involvement. The rest of the cornea was transparent. The anterior chamber was of moderate depth and the pupil was mobile (Figs. 6).
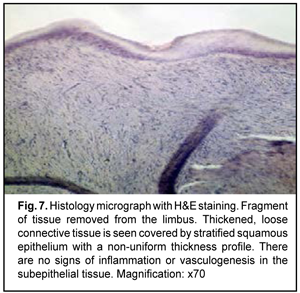
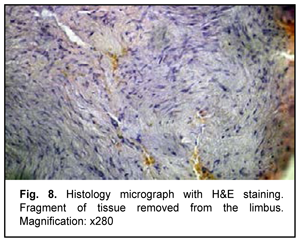
The clinical diagnosis was a limbal neoplasm with partial peripheral corneal involvement. The patient was suspected of having either dermoid, lipodermoid or lipoma. Impression cytology showed transitional and epidermal epithelial layers without cell atypia or polymorphism. This patter is characteristic of benign epithelial hyperplasia. On April 3, 2018, the patient underwent removal of the limbal and corneal lesion and subsequent keratoscleral plasty. The removed tissue was sent for histological examination (Figs. 7,8).
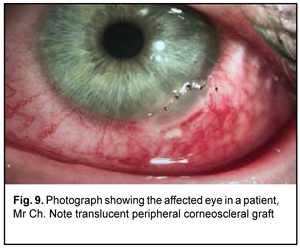
At the time of discharge: UCVA was 1.0 OD and 0.5 OS and the pin-hole visual acuity was 1.0 OS. On biomicroscopy of the left eye, the conjunctiva was pink. The lamellar graft was seen at the limbus at the 5 o’clock position and was transparent, adapted with interrupted sutures, and did not stain with fluorescein. The rest of the cornea was transparent. The anterior chamber was of moderate depth and the pupil was mobile (Fig. 9).
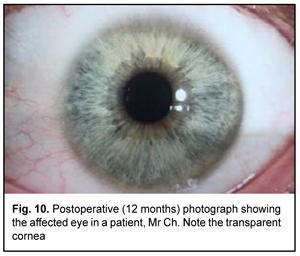
At 12 months after surgery, the cornea was transparent and epithelized (Fig. 10). UCVA was 1.0 OU.
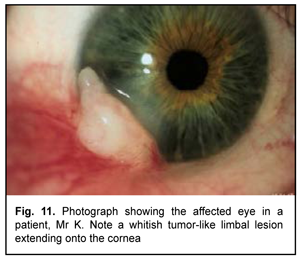
Case 3 A male patient of 52 years presented to us with a 4-month history of a gradually increasing white lesion in his right eye. He complained of redness, itching and foreign body sensation in this eye. In addition, he had a history of pterygium surgery in his right eye 7 months before. At presentation, UCVA was 0.6 OD and 1.0 OS. Biomicroscopy of the right eye revealed a white lesion at the limbus between 7 and 8 o’clock. The rest of the cornea was transparent. The anterior chamber was of moderate depth and the pupil was mobile (Fig. 11).
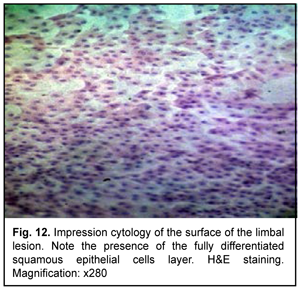
Clinically, a recurrent lesion was suspected to be dermoid or fibroma. Impression cytology showed a well differentiated epithelial tissue pattern (Fig. 12).
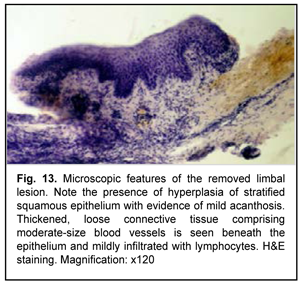
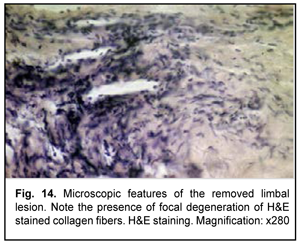
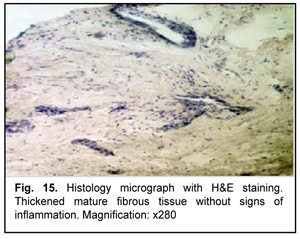
A B-scan ultrasound image of the right eye showed moderately echogenic substrate measuring 2.5-mm thickness and 8.4 х 7.2-mm lengths at the limbus from 7 to 9 o’clock. The corneal thickness beneath the substrate was 0.25-0.35 mm. On January 19, 2017, the patient underwent removal of the limbal and corneal lesion and subsequent keratoscleral plasty in the right eye. The removed tissue was sent for histological examination (Figs. 13-15).
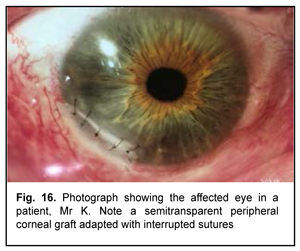
At the time of discharge: UCVA was 0.6 OD and 1.0 OS. On biomicroscopy of the right eye, the conjunctiva was pink; the corneoscleral graft in the external inferior quadrant of the cornea was transparent, adapted with interrupted sutures, and did not stain with fluorescein. The limbus was well vascularized. The rest of the cornea was transparent (Fig. 16).
At 7 months after surgery, the peripheral corneal graft was transparent (Fig. 17) and UCVA was 1.0 OU.
Discussion The final diagnosis in patients with tumor-like corneal and limbal lesions requires a detailed and thorough examination. Limbal tumor-like lesions require thorough diagnostic evaluation including impression cytology is a must to differentiate benign from malignant epithelial lesions. Since dermoid cysts may occur in various sites it is important to establish whether the cyst is superficial or deep in order to perform the appropriate surgery [12]. For relatively superficial dermoids, amniotic membrane transplantation may help with the healing process after removal of cysts. The amniotic membrane has proven useful in ocular surface lesions as an alternative treatment in various pathologies of the cornea, conjunctiva, sclera and eyelid [13, 14, 15]. The amniotic membrane facilitates healing with minimal inflammation and scarring by combining its mechanical action with biological factors. In addition, it promotes cell migration, facilitates cell adhesion, cell differentiation and other factors that make it useful in the management of injuries of the ocular surface [16, 17, 18]. Lamellar keratoplasty or keratoscleral plasty is recommended for deep corneal lesions [19, 20]. Final diagnosis requires histological examination of the tissue removed at operation. The cases reported are interesting in that the clinical picture was not supported by histological evidence. The initial diagnosis of dermoid or lipodermoid was based on biomicroscopic findings in all the three cases, but pathomorphological and cytological studies revealed benign epithelial hyperplasia. Neoplasms were removed intracapsularly in all the three cases, with immediate amniotic membrane transplantation in a patient with a superficial corneal defect, and immediate keratoscleral plasty in two patients with deep corneoscleral defects. Histological examination of intraoperatively removed tissues revealed fibrous tissue displaying different levels of maturity with evidence of residual inflammation (in one case) or vascularization (in another case). The diagnosis of dermoid or lipodermoid was not confirmed in any case. It appears that in all the three cases the tumor-like lesion was of traumatic origin or was caused by persistent limbal inflammation resulting in partial limbal stem cell loss and connective tissue migration to the corneal surface. Conclusion Although the clinical picture appeared typical of dermoid, tumor-like lesions require thorough diagnostic evaluation including impression cytology to differentiate benign from malignant epithelial lesions. In addition, the tissue removed during the surgical procedure must be sent to the pathological laboratory for histological verification of diagnosis. The surgical option for a limbal tumor-like lesion may be keratoscleral plasty or amniotic membrane transplantation depending of invasion depth and lesion extension.
References 1.Vit VV. [Pathology of the eye, ocular adnexa and orbit]. Vol. 1. Odesa:Astroprint; 2019. Russian. 2.Saakyan SV, Tatskov RA, Ivanova OA, Tsygankov AY, Maybogin AM. [Surgical Treatment of Epibulbar Malformations]. Ophthalmology in Russia. 2019;16(3):289-95. Russian. 3.Elsas FJ, Green WR. Epibulbar tumors in childhood. Am J Ophthalmol. 1975 Jun;79(6):1001–7. 4.Boynton JR, Searl SS, Ferry AP, Kaltreider SA, Rodenhouse TG. Primary nonkeratinized epithelial (‘conjunctival’) orbital cysts. Arch Ophthalmol. 1992; 110:1238–42. 5.Sathananthan N, Moseley IF, Rose GE, Wright JE. The frequency and clinical significance of bone involvement in outer canthus dermoid cysts. Br J Ophthalmol. 1993 Dec;77(12):789-94. 6.Karatza EC, Shields CL, Shields JA, Eagle JRC. Calcified orbital cyst simulating a malignant lacrimal gland tumor in an adult. Ophthal Plast Reconstr Surg. 2004 Sep;20(5):397–9. 7.Rajabi MT, Ramezani K. Lipodermoid Cyst: A Report of a Rare Caruncular Case. Middle East Afr J Ophthalmol. 2015 Oct-Dec;22(4):528-30. 8.Fasina O, Ogun OG. Giant deep orbital dermoid cyst presenting early in infancy in a Nigerian child: a case report and review of the literature. J Med Case Rep. 2012;6:320. 9.Robb RM. Astigmatic refractive errors associated with limbal dermoids. J Pediatr Ophthalmol Strabismus. 1996 Jul-Aug;33(4):241-3. 10.Scott JA, Tan DT. Therapeutic lamellar keratoplasty for limbal dermoids. Ophthalmology. 2001 Oct;108(10):1858-67. 11.Watts P, Michaeli-Cohen A, Abdolell M, Rootman D. Outcome of lamellar keratoplasty for limbal dermoids in children. J AAPOS. 2002 Aug;6(4): 209–15. 12.Villal?n ML, Leal ML?, Chavez JR, et al. Recurrent epibulbar dermoid cyst treated with amniotic membrane implant a case report. BMC Surg. 2018 Nov 14;18(1):98. 13.Kruse FE, Joussen AM, Rohrschneider K, You L, Sinn B, Baumann J, et al. Cryopreserved human amniotic membrane for ocular surface reconstruction. Graefes Arch Clin Exp Ophthalmol. 2000 Jan;238(1):68–75. 14.Malhotra C, Jain AK. Human amniotic membrane transplantation: Different modalities of its use in ophthalmology. World J Transpl. 2014 Jun 24;4(2):111-21. 15.Gheorghe A, Pop M, Burcea M, Serban M. New clinical application of amniotic membrane transplant for ocular surface disease. J MedLife. 2016 Apr-Jun;9(2):177-9. 16.Li DQ, Tseng SC. Three patterns of cytokine expression potentially involved in epithelial-fibroblast interactions of human ocular surface. J Cell Physiol. 1995 Apr;163(1):61-79. 17.Hao Y, Ma DH, Hwang DG, Kim WS, Zhang F. Identification of antiangiogenic and antiinflammatory proteins in human amniotic membrane. Cornea. 2000 May;19(3):348-52. 18.Zhang S, Zhu YT, Chen SY, He H, Tseng SC. Constitutive expression of pentraxin 3 (PTX3) protein by human amniotic membrane cells leads to formation of the heavy chain (HC)-hyaluron an (HA)-PTX3 complex. J Biol Chem. 2014 May 9;289(19):13531-42. 19.Watts P, Michaeli-Cohen A, Abdolell M, et al. Outcome of lamellar keratoplasty for limbal dermoids in children. J AAPOS. 2002 Aug;6(4):209-15. 20.Zhong J, Deng Y, Zhang P, et al. New Grading System for Limbal Dermoid: A Retrospective Analysis of 261 Cases Over a 10-Year Period. Cornea. 2018 Jan;37(1):66-71.
The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|