J.ophthalmol.(Ukraine).2020;2:70-78.
|
http://doi.org/10.31288/oftalmolzh202027078 Received: 05 February 2020; Published on-line: 30 April 2020 Clinical decision support system for extraocular muscle pathology M.L. Kochina1, Dr Sc (Biol), Prof.; Yu.A. Demin2, Dr Sc (Med), Prof.; O.V. Yavorsky3, Dr Sc (Med), Prof.; N. M Kovtun4, Ophthalmologist; O.G. Firsov5, Cand Sc (Techn) 1 Petro Mohyla Black Sea National University; Mykolaiv (Ukraine) 2 Kharkiv Medical Academy of Postgraduate Education; Kharkiv (Ukraine) 3 Kharkiv National Medical University; Kharkiv (Ukraine) 4 Oftalmika, International Medical Center; Kharkiv (Ukraine) 5 ASTER IT LLC; Kharkiv (Ukraine) E-mail: kochinaml@gmail.com TO CITE THIS ARTICLE: Kochina ML, Demin YuA, Yavorsky OV, Kovtun NM, Firsov OG. Clinical decision support system for extraocular muscle pathology. J.ophthalmol.(Ukraine).2020;2:70-78. http://doi.org/10.31288/oftalmolzh202027078
Background: Integration of clinical decision support systems (CDSS) into clinical practice commonly allows improvements in efficacy of diagnosis, treatment and observation of patients, particularly those with eye disease. Purpose: To substantiate and develop an automated CDSS for extraocular muscle pathology in strabismus. Material and Methods: We used polarized light to assess the parameters of interference patterns for 147 patients with strabismus due to abnormal structure and function of extraocular muscles. Results: The following informative interference pattern parameters were determined based on the results of studies and modeling of interference patterns: interference diamond diagonal segments, angles between two diagonal segments, and angles between the diagonal segment and relevant meridians. The main features of interference patterns for various types of strabismus were identified. An automated system using the above informative interference pattern parameters for clinical decision support for extraocular rectus muscle pathology in strabismus was proposed. Conclusion: Application of the proposed CDSS with enable the ophthalmologist to obtain information on the structural and functional state of the extraocular rectus muscles in 2 to 3 minutes. In addition, it will enable him/her to judge the state of the extraocular oblique muscles indirectly if the symmetrical corneal interference pattern is obtained for the strabismic eye. Keywords: strabismus, polarizing optical studies, clinical decision support system
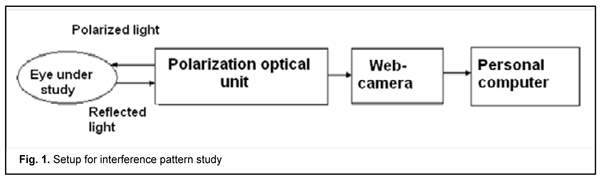
Introduction There is a current worldwide trend towards introduction of information technologies in healthcare [1]. Information systems are introduced in various medical areas to facilitate processing and systematizing of vast amounts of data, producing analytical reviews, predicting disease course and outcomes, providing clinical decision support, etc [2]. As decision making in medicine is directly related to human health and life, the results obtained with the help of information decision support systems (DSS) should be as reliable as possible [3-5]. DSS are computerized systems designed to effectively influence the processes of decision making by specialists working in various fields of medicine [3, 6]. They commonly incorporate computerized procedures for selecting, processing and analyzing medical data, developing alternative decisions and substantiating the choice of the optimum diagnostic or treatment modality [3,7]. Recently, DSS have been increasingly used in ophthalmology, which is associated with the rapid integration of advanced diagnostic and treatment technologies into clinical practice [9]. The exponential growth of the amount of data on the features and course of such socially diseases as cataract, glaucoma, diabetic retinopathy, uveitis, myopia, strabismus, etc., makes it difficult for doctors to assimilate and understand the full range of new information in real time. Given the growing demand for quality eye care services and high cost of medical errors, there is a clear need to develop intelligent DSS to assist the ophthalmologist [10-14]. In addition, with an advance of novel eye imaging techniques, the amount of digital ophthalmological data to be analyzed has considerably increased, which makes important the incorporation of computerized data processing systems and DSS to assist the physician in making an accurate clinical diagnosis and improving treatment outcomes. Clinical DSS for predicting the risk of diabetic retinopathy and assessing patients with this disease are especially popular currently [15-17]. While the existing diagnostic approach requires access to ophthalmologists and expensive equipment, the clinical DSS built by Piri and coauthors [18] only uses demographic and lab data to detect patients' susceptibility to diabetic retinopathy with a high accuracy. Hospital Eye Services (HES) in the UK face an increasing number of optometric referrals driven by progress in retinal imaging. In the study by Kern and colleagues [19], a cloud-based referral platform was implemented to improve communication between optometrists and ophthalmologists. After reviewing the patient's data in a web-based interface 54 (52%) out of 103 attending patients initially classified into the referral pathway did not need a specialist referral. This resulted in eye care cost savings to the National Health Service. Application of OphthalDSS [20], a mobile DSS for diagnosing anterior eye diseases, especially those which produce red eye, allowed reducing the load on specialists. Diagnosis and treatment of strabismus is still a challenge, since the number of strabismic patients is not decreasing [21]. An automated telemedicine system for improved diagnosis of strabismus has been built. Its principle is as follows: tele strabismus dataset is established by ophthalmologists. Then an end-to-end framework named as RF-CNN is proposed to achieve automated strabismus detection on the established tele strabismus dataset. RF-CNN first performs eye region segmentation on each individual image, and further classifies the segmented eye regions with deep neural networks. The telemedicine DSS enables making a decision on the presence or absence of strabismus in a patient, and, if required, referring this patient to a relevant specialist [22]. An innovative intelligent evaluation system of strabismus in digital videos, based on the cover test has been proposed. In particular, the video is recorded using an infrared camera, while the subject performs automated cover tests [23]. An automated system, based on eye tracking and dedicated full occlusion glasses, was developed to provide another alternative to the manual measurements of strabismus [24]. STRABO, a clinical DSS for treating strabismus, uses modeling to develop a plan for treating non-accommodative esotropia in an individualized way [25]. The DSS uses the following parameters of a patient with strabismus to determine the number of stages and amount of strabismus surgery: axial length of the eye, pupil-to-pupil distance, strabismus angle and amount of hyperopia. The system calculates the eye turn to achieve alignment of the eyes as well as the number of stages required for strabismus surgery. This DSS does not use the data on the state of extraocular muscles (EOM), but determines the total angle of deviation which can result from various combinations of structural and functional disorders of the EOM. The developers of the DSS noted that the technology can be used only for horizontal convergent strabismus (esotropia) and performing recession-resection surgery (or muscle-folding operation instead or resection), since the DSS interface provided in the paper [26] does not allow for entering additional data relevant to the patient [26]. Much more parameters should be determined and taken into account in calculations of the amount of surgery required to correct for the types of strabismus (e.g., vertical strabismus or combined horizontal and vertical strabismus) associated with oblique muscle pathology or displacement of rectus muscle insertion. A comparison clinical study [27] was conducted to assess the efficacy of the biomechanical eye model SEE-KID for determining the amount of surgery required to correct for strabismus. The success rate for strabismus surgery performed based on recommendations of the model was found to be as low as 50.9%. The authors of that study believed that the use of only one parameter (namely, total angle of deviation) was not enough for effective determination of the amount of surgery required to correct for strabismus. The model can be used as a clinical DSS, but only in combination with traditional methods for preoperative diagnosis of EOM pathology. The study by Romanenko et al [28] aimed to assess extraocular muscle motility in patients with concomitant or non-concomitant strabismus and vertical deviation through automatic analysis of 2D images of the eye moved into diagnostic gaze positions. The developed methodology is capable of objective assessment of oblique muscles in strabismus with vertical deviation and using intellectual data processing methods. In fact, those authors developed an automated DSS for determining the pathology of oblique muscles which allows identifying the cause of strabismus and features of treatment for the specific patient. Therefore, integration clinicall DSS into clinical practice commonly allows improvements in efficacy of diagnosis, treatment and observation of patients, particularly those with eye disease. We used the results of studies on and modeling of the stress-strain state of the cornea for developing a clinical DSS for determining the structural and functional disorders of the EOM. Investigations of the cornea using polarized light have been conducted for more than two centuries. Brewster was the first to describe the interference pattern generated in the living cornea in 1815 [29]. Subsequently, Cogan [30], Stanworth [31] and Stanworth and Naylor [32-33] conducted further research on the polarized optics of the cornea. A study by Zandman [34] forms the basis for current views on the nature and features of optical anisotropy of the cornea. The author determined the physical nature of the interference pattern observed on the cornea, and pointed that the main contributors to this effect are EOM and intraocular pressure (IOP). The mechanical effect of these factors changes the inherent optical anisotropy of the cornea caused by the optical characteristics of corneal collagen and geometrical characteristics of the cornea. Penkov and Kochina [35] were the first to conduct studies on polarization characteristics of the cornea in strabismic eyes. Subsequent studies were conducted by Vodovozov and Kovylin [36] and Bosenko [37]. Modeling of the stress-strain state of the cornea in different states of the EOM using thin-shell theory [38,39] and the ANSYS Finite Element Analysis System [40] and fuzzy-logic based interference pattern classification [41] allowed determining the basic features and quantitative values of the parameters of polarized light interference patterns observed on the cornea in normal and pathological EOM. Findings of these studies were confirmed by results of a study on the parameters of interference patterns in patients with different types of strabismus [42,43]. All these allowed us to develop an EOM pathology classification based on corneal interference patterns, which became the foundation for developing a clinical DSS for the structural and functional pathology of the EOM. The purpose of the study was to substantiate and develop an automated clinical decision support system for extraocular muscle pathology in strabismus. Material and Methods The polarized light interference patterns observed on the cornea in normal and strabismic individuals were recorded using the setup in Fig. 1. A polarization optical unit (POU) mounted on the web-camera lens is composed of two parts, the illumination part and the polarization part. The former is designed as a ring of light-emitting diodes, and the latter as a set of two crossed polarizing filters. The light from LEDs becomes polarized after passing through the first polarizing filter, and enters the cornea which is anisotropic. The polarized light changes its polarization state while passing through the cornea, then passes to the anterior eye and is reflected from the iris. Thereafter, the light passes through the cornea another time, and passes through the second polarizing filter which is mounted directly on the web-camera lens, producing corneal interference pattern image on the camera matrix. This interference pattern image is subsequently processed by software in the computer.
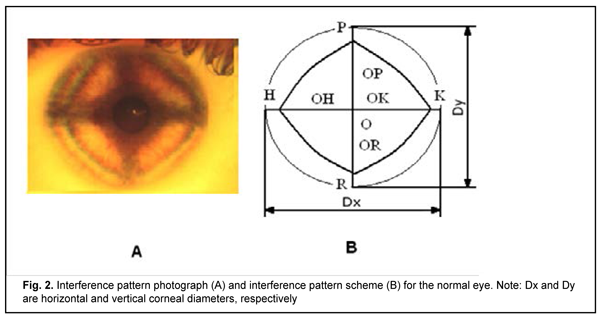
During the interference pattern recording procedure, the patient’s head should be immobilized, and the eye should be in a state of orthophoria. The first order isochromatic is the brightest in the interference pattern image and is used in all measurements of interference pattern parameters. Fig. 2 shows the interference pattern (Fig. 2A) and the first-order isochromatic scheme (Fig. 2B) for the normal eye. The scheme presents informative indicators for assessing the state of EOM, namely, segments of the diagonals in the interference diamond (OK, OH, OP, and OR) and angles between these segments (?KOP,?POH,?HOR, and ?ROK) [41]. In all images and schemes, OK, OH, OP, and OR segments correspond to the internal rectus muscle, external rectus muscle, superior rectus muscle, and inferior rectus muscle, respectively. The effect of interference pattern image scale on study results was excluded by normalizing measurements of linear parameters of interference patterns to the measurement of mean corneal diameter calculated as (Dx+Dy)/2.
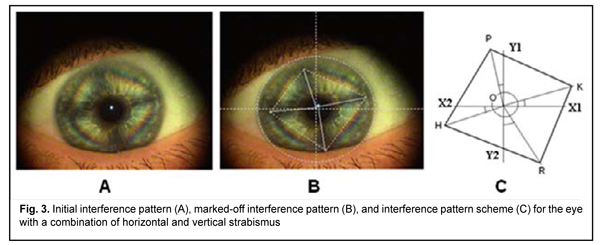
To develop an EOM pathology classification based on corneal interference patterns, we used (1) parameters of interference patterns for 147 strabismic patients in whom the presence of pathology of specific EOM was confirmed, and (2) parameters of calculated isochromes produced by modeling of the stress-strain state of the cornea in various structural and functional states of the EOM [38-40]. While determining the geometric parameters of interference patterns, we singled out cases involving the displacement of interference diamond angles from respective meridians (Fig. 3A). In such cases we proposed to determine complementary angles (?KOX1,?POY1,?HOX2, and ?ROY2) formed between interference diamond diagonal segments and relevant meridians (Fig. 3B). Fig. 3C shows the interference pattern scheme for the case involving the displacement of interference diamond angles from respective meridians.
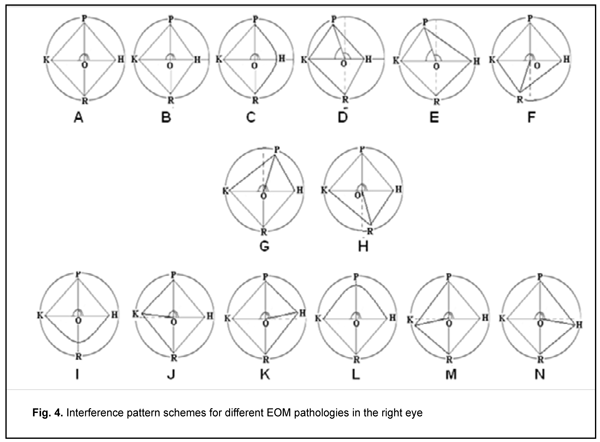
We have demonstrated previously that the shift of interference diamond angles from respective meridians indicated dislocation of the site of attachment of the relevant muscle. In addition, modeling of the stress-strain state of the cornea in various EOM attachment sites and the plotting of calculated isochromates [38-40] allowed finding that insubstantial (2 to 4 degrees) shifts of diamond angles from respective meridians could result from superposition of stresses from all extraocular recti muscles. Commonly, the largest angles between the meridian and interference diamond diagonal segment are found close to the muscles which sites of attachment are dislocated in the direction in which interference diamond angle is shifted. Results and Discussion Studies of interference patterns of strabismic patients were conducted and modeling of the stress-strain state of the cornea in various EOM attachment sites was performed, and main features and geometric parameters of these interference patterns were determined (Fig. 4). The schemes in Fig. 4 correspond to convergent strabismus (esotropia; A-F), divergent strabismus (exotropia; G-H), vertical strabismus with upward deviation (I-K) and vertical strabismus with downward deviation of the eye (L-N).
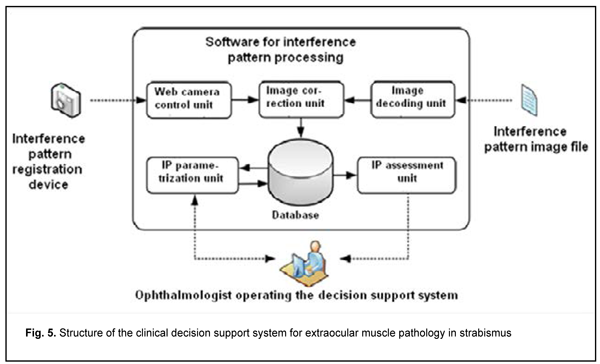
A symmetric interference pattern (Fig. 4 A) in the presence of deviation is a sign of purely functional EOM impairment that does not requires extraocular rectus muscle surgery. An increased length of interference diamond diagonal segment is seen at the side of action of a more powerful muscle (Fig. 4 B). The interference diamond is asymmetric if the antagonist muscle functions normally. The relevant diamond angle is rounded if there is underaction of the antagonist muscle (Fig. 4 C). We found dislocation of the site of attachment of a vertical EOM to be a common cause of horizontal strabismus (Fig. 4D, E, F). The interference pattern in Fig. 4D corresponds to combination of superior rectus displacement in the direction of the medial rectus and weak action of the lateral rectus; the interference pattern in Fig. 4E corresponds to superior rectus dislocation in the presence of horizontal muscle balance. The interference pattern in Fig. 4F corresponds to inferior rectus displacement in the direction of the medial rectus. Interference patterns in Fig. 4F and 4G correspond to divergent strabismus (exotropia) which either results from vertical muscle insertion displacement from the respective meridian, or is observed when vertical muscle insertion is parallel to the limbus [37]. Vertical deviations of the eye can result from imbalanced action of vertical rectus muscles (overaction, underaction, or vertical muscle insertion displacement along the action path either in the direction or opposite to the direction of the limbus) (Fig. 4G and 4L). In addition, vertical deviations of the eye can result from horizontal muscle insertion displacement from the horizontal meridian (Fig 4 J,K and Fig. 4M,N). If vertical deviation of the eye is present in the absence of loss of interference pattern shape, one of the possible causes is oblique muscle pathology. Biomechanically, the action of oblique muscles has no effect on internal stress distribution in the cornea, which was confirmed by clinical observation. Mean values and ranges of interference pattern parameters (length of diagonal segments and angles between these segments) were determined for all cases presented in Fig. 4. Mean values and ranges of complementary angles were additionally determined for the cases of shifts of diamond angles from respective meridians. Our studies demonstrated that parameters of polarized-light interference patterns observed on the cornea can be used as criteria for the assessment of structural and functional states of the EOM. Using the data for patients with extraocular muscle pathology, we developed fuzzy models which enable classification of polarized-light interference patterns observed on the cornea based on values of pattern parameters and determination of a possible cause of deviation of the eye for each specific case [41]. We developed a clinical DSS with software for determining structural and functional states of the EOM in order to transfer study results into clinical practice. The structure of the clinical DSS is presented in Fig. 5.
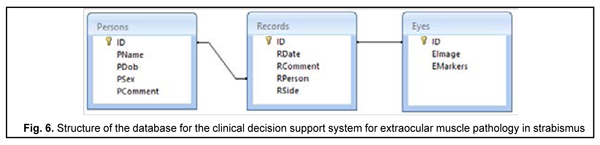
The DSS can be provided with an interference pattern image in either of the two following ways. The image can be recorded directly by means of a web-camera-based device (through the Web Camera Control Module) or loaded into the DSS through the Image Decoding Module as a previously obtained file. The Image Correction Module improves quality of interference pattern image, and the latter is saved in the data base, and processed by the IP Parametrization Module to determine interference pattern image parameters [44]. Thereafter, fuzzy-logic based interference pattern image classification is performed, which allows identifying the EOM pathology. A physician operating the DSS can either obtain the results of IP parametrization manually and make a conclusion regarding the pathology, or analyze the results of classification. The database of examined patients, interference pattern images and interference pattern parameters consists of the three interrelated tables, Persons, Records, and Eyes. The structure of inter-table relationships is presented in Fig. 6. Persons and Records tables contain basic information about examined individuals and patient eye examination results, respectively, whereas the Eyes table contains interference pattern images and parameters.
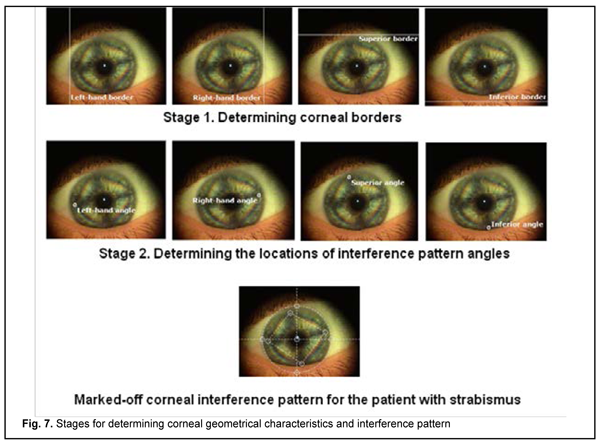
Interference pattern processing software was developed in Microsoft. Net Framework which is equipped with advanced tools for developing the Graphic User Interface (GUI) and data access, processing and visualization. Microsoft. Net Framework Windows Forms enable easy access to Microsoft Windows GUI elements. The applications which are developed by using Windows Forms provide for a homogeneous software model and reduced number of mistakes and conflicts in the developed Windows-style GUI, and can be run on obsolete computer equipment. The user of the developed software may create new database files, perform operations with the data of previously saved files, save basic information about examined individuals in the database, and, if required, edit or remove data from the database. Examination result data is stored in the database as records including the date of examination and description text. Each record is connected with the corneal interference pattern image. The image may undergo parametrization any time in order to determine lengths of diagonal segments and relevant angles for the interference pattern under study. Fig. 7 presents an example of processing the corneal interference pattern image for a strabismic patient. In the first stage of image processing, vertical and horizontal corneal diameters are determined with the help of vertical and horizontal lines. In the second stage, angles of the interference diamond are marked using the ring-shaped interactive marks.
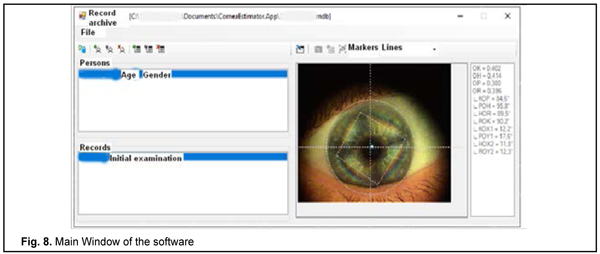
Fig. 8 presents the Main Window of the software. The determined normalized parameters of corneal interference pattern image for a strabismic patient are presented in the right-hand panel of Fig. 8. The values of diagonal segment length ratios (OK/OH = 0.97; OP/OR = 0.96) in the interference diamond indicate a symmetrical action of horizontal and vertical muscles. On the other hand, the values of angles (?KOX1,?POY1,?HOX2,?ROY2) between interference diamond diagonal segments and relevant meridians indicate significant deviations of the line along which the effort of the rectus muscles is directed from the relevant meridian. In this case, deviation of the eye is determined by a superposition of effects from a number of factors like displacement of the insertions of all the four rectus muscles to the sclera, visual function of both eyes, and central visual perception mechanisms.
The above example case demonstrates that in some cases determining the cause of strabismus can be challenging. The presence of complex relationships in the EOM system may explain failures of surgery in cases when correction for deviation of the eye was performed using a traditional methodology without elucidating the actual cause of strabismus which may be associated with muscle insertion displacement from the relevant meridians. Conclusion First, polarizing optical studies of the stress-strain state of the cornea is a promising approach to determining the structural and functional pathology of the EOM, and automatization of this approach will allow obtaining additional information for optimal choice of treatment strategy for strabismus. Second, interference diamond diagonal segments, angles between two diagonal segments, and angles between the diagonal segment and relevant meridians have high information value for determining the state of the extraocular muscles. Finally, application of the proposed clinical DSS with enable the ophthalmologist to obtain information on the structural and functional state of the extraocular rectus muscles in 2 to 3 minutes. In addition, it will enable him/her to judge the state of the extraocular oblique muscles indirectly if the symmetrical corneal interference pattern is obtained for the strabismic eye.
References 1.Clinical Decision Support (CDS). Office of the National Coordinator for Health Information Technology. 2013 [cited 31 August 2017]. Available from: https://www.healthit.gov/policy-researchers-implementers/clinicaldecisio.... 2.Miller RA. Medical diagnostic decision support systems – past, present, and future: a threaded bibliography and brief commentary. J Am Med Inform Assoc. 1994 Jan-Feb;1(1):8–27. 3.Kobrinsky BA. [Decision Support Systems in Public Health Services and Training]. Vrach i informatsionnyie tekhnologii. 2010;2:39-45. 4.Yao W, Kumar A. CONFlexFlow: integrating flexible clinical pathways into clinical decision support systems using context and rules. Decis Support Syst. 2013;55(2):499–515. 5.Castaneda C, Nalley K, Mannion C, Bhattacharyya P, Blake P, Pecora A, Suh KS. Clinical decision support systems for improving diagnostic accuracy and achieving precision medicine. J Clin Bioinforma. 2015 Mar 26;5:4. 6.Litvin AA, Litvin VA. [Clinical decision support systems for surgery]. Novosti khirurgii. 2014;22(1):96-100. 7.Liberati EG, Ruggiero F, Galuppo L, Gorli M, Gonzalez-Lorenzo M, Maraldi M, et al. What hinders the uptake of computerized decision support systems in hospitals? A qualitative study and framework for implementation. Implement Sci. 2017 Sep 15;12(1):113. 8.Paunksnis A, Barzdziukas V, Jegelevicius D, Kurapkiene S, Dzemyda G. The use of information technologies for diagnosis in ophthalmology. J Telemed Telecare. 2006;12 Suppl 1:37-40. 9.Sumeet D, Mohit J. Computational Decision Support Systems and Diagnostic Tools in Ophthalmology: A Schematic Survey. In: Computational Analysis of the Human Eye with Applications. World Scientific Publishing. 2015. 10.Trikha S. AI decision support systems for Ophthalmic care - the competitive advantage? Dec 30, 2017, 08.05 AM IST. Available from: https://health.economictimes.indiatimes.com /health-files/ai-decision-support-systems-for-ophthalmic-care-the-competitive-advantage/2781 11.Kahai P, Namuduri KR, Thompson H. A decision support framework for automated screening of diabetic retinopathy. Int J Biomed Imaging. 2006;2006:45806. 12.Noronha K, Acharya U, Nayak K, Kamath S, Bhandary S. Decision support systemfor diabetes retinopathy using discrete wavelet transform. Proc Inst Mech Eng H. J Eng Med. 2013: 227(3):251-61. 13.Kumar SJJ, Madheswaran M. An improved medical decision support system to identify the diabetic retinopathy using fundus images. J Med Syst. 2012 Dec;36(6):3573-81. 14.Xiao D, Vignarajan J, Lock J, Frost S, Tay-Kearney M-L, Kanagasingam Y. Retinal image registration and comparison for clinical decision support. Australas Med J. 2012;5(9):507–12. 15.Li Zhang. An intelligent mobile based decision support system for retinal disease diagnosis. J Health Med Informat. 2014;59:341-50. 16.Prasanna P, Jain S, Bhagat N, Madabhushi A. Decision support system for detection of diabetic retinopathy using smartphones. In: Pervasive Computing Technologies for Healthcare (Pervasive Health). 2013; 7th International Conference on 2013, pp. 176–179. 17.Bourouis A, Feham M, Hossain MA, Zhang L. An intelligent mobile based decision support system for retinal disease diagnosis. Decis Support Syst. 2014;59:341–50. 18.Piri S, Delen D, Tieming LT, Zolbanin HM . A data analytics approach to building a clinical decision support systemfor diabetic retinopathy: Developing and deploying a model ensemble. Decis Support Syst. 2017 September; 19.Kern C, Fu DJ, Kortuem K, Huemer J, Davis A, Balaskas K, et al. Implementation of a cloud-based referral platform in ophthalmology: making telemedicine services a reality in eye care. Br J Ophthalmol. 2019. doi:10.1136/ bjophthalmol-2019-314161. 20.L?pez MM, L?pez MM, de la Torre D?ez I, Jimeno JC, L?pez-Coronado M. A mobile decision support system for red eye diseases diagnosis: experience with medical students. J Med Syst. 2016 Jun;40(6):151. 21.Vitovska OP, Savina OM. [The structure and sickness rate of eye and adnexa diseases in children in Ukraine]. Medicni perspektivi. 2015; .XX (3): 133-8. Ukrainian. 22.Lu J, Feng J, Fan Z, Huang L. Automated Strabismus Detection based on Deep neural networks for Telemedicine Applications. Available from:https://www.researchgate.net/profile/Jiewei_Lu 23.Yang Z, Fu H, Li R, Lo W-L. Intelligent Evaluation of Strabismus in Videos Based on an Automated Cover Test. Appl Sci. 2019;9:731-47. 24.Yehezkel O, Belkin M, Wygnanski–Jaffe T. Automated Diagnosis and Measurement of Strabismus in Children. Am J Ophthalmol. 2019 Dec 27. pii: S0002-9394(19)30619-1. 25.Strabo care system. Available from: https://strabo-care.com. Russian. 26.Aznauryan IE, Balasanyan VO, Kudryashova EA, Uzuev MI. [StraboCare technology for dosing friendly strabismus surgery]. In: Proceedings of the 1st Intenational conference for ophthalmologists and strabismologists. STRABO 2019. New technologies in the diagnosis and treatment of ocular motility pathology. Moscow, 2019. p.7. Russian. 27.Bushueva NN, Romanenko DV, Tarnopolska IN. [Results of the surgical treatment of associated squint with preliminary modeling of operations by using three-dimensional biomechanical model of the eye]. Oftalmol Zh. 2014;1:18-23. Russian. 28.Romanenko DV, Bushuyeva NN, Dukhayer S, Pelypenko OV. [Assessment of extraocular muscle motility in patients with concomitant and non-concomitant strabismus with vertical component using automated analysis of two-dimensional eye globe pictures in diagnostic gaze positions]. Oftalmol Zh. 2014;5:15-9. Russian. 29.Brewster D. Experiments on the depolarization of light as exhibited by various mineral, animal and vegetable bodies with a reference of the phenomena to the general principles of polarization. Phil Trans Roy Soc Lond. 1815;1:21–53. 30.Cogan DC. Some ocular phenomena produced with polarized light. Arch Ophthalmol. 1941;25(3):391–400. 31.Stanworth A. Polarized light studies of the cornea II. The effect of intraocular pressure. J Exp Biol. 1953;30(2):164–9. 32.Stanworth A, Naylor EJ. The polarization optics of the isolated cornea. Br J Ophthalmol. 1950;34(4):201–11. 33.Stanworth A, Naylor E J. Polarized light studies of the cornea I. The isolated cornea. J Exp Biol. 1953;30:160–3. 34.Zandman F. The photoelastic effect of the living eye. Experim Mechanics. 1966;6(5):19–25. 35.Penkov MA, Kochina ML. [Interference method in strabismus diagnosis]. Vestn Oftalmol. 1981 Jan-Feb;(1):39-41. Russian. 36.Vodovozov AM, Kovylyn VV. [The use of an optical polarization method for the evaluation of oculomotor muscle function in vertical deviation]. Oftalmol Zh. 1990;(4):201-4. Russian. 37.Bosenko TA. [Diagnosis of asymmetry of the outer muscles of the eye in polarized light with squint]. Aktualnye voprosy oftalmologyy: sbornyk nauchnykh trudov. Kharkiv; 1987:33–5. Russian. 38.Kochina ML, Demin YuA, Kovtun NM, Kaplin IV. [Model of stress-strain state of the cornea of the eye]. East European Scientific Journal. 2017; 2(18):61-66. Russian. 39.Kochyna ML, Kalymanov VG. [Results of modeling the stress – strain state of the cornea of the eye using the ANSYS engineering analysis system]. Klynycheskaya informatika i telemeditsina. 2009;5(6):26–30. Russian. 40.Kochina M L, Kovtun NM. [Results of Modeling the Stress–Strain Stat of the Eye Cornea with Extraocular Muscles Pathology]. Ukrainian journal of medicine, biology and sport. 2020;5(23):135-43. 41.Kochyna ML, Kalymanov VG. [Classification of oculomotor muscle lesions using fuzzy logic apparatus]. Kibernetika i vychislitelnaya tekhnika. 2011;166: 97–107. Russian. 42.Kochina ML, Demin YuA, Kovtun NM, Kaplin IV. [Peculiarities of interferential pictures of eyes at horizontal heterotropy]. Ukrainian journal of medicine, biology and sport. 2017;2(4):75-81. Russian. 43.Kovtun NM. [Interference Patterns of the Eye Cornea with Different States of Oculomotor Muscles]. Ukrainian journal of medicine, biology and sport. 2017; 2(6): 81–86. Russian. 44.Kaplin IV, Kochina ML, Demin YuA, Firsov AG. [The conception of telemedicine system for express estimation of intraocular pressure’s level]. Kibernetika i vychislitelnaya tekhnika. 2018;1 (191):76-94. Ukrainian.
The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|