J.ophthalmol.(Ukraine).2020;1:32-34.
|
http://doi.org/10.31288/oftalmolzh202013234 Received: 17 December 2019; Published on-line: 21 February 2020 Morphological features of the lamina cribrosa in patients with various degrees of myopia P.A. Bezditko, Dr Sc (Med), Prof.; A.O. Gulida, Post-Graduate Student Kharkiv National Medical University; Kharkiv (Ukraine) E-mail: anastasiiagulida@gmail.com TO CITE THIS ARTICLE: Bezditko PA, Gulida AO. Morphological features of the lamina cribrosa in patients with various degrees of myopia. J.ophthalmol.(Ukraine).2020;1:32-34. http://doi.org/10.31288/oftalmolzh202013234
Background: The lamina cribrosa plays an important role in the development of vision and undergoes changes as myopia evolves. Purpose: To examine morphological features of the lamina cribrosa in high, moderate and low myopes vs generally healthy controls using optical coherence tomography (OCT)-derived markers. Methods: Fourier-Domain OCT of the outer portion of the optic disc was performed in 40 low myopes (Group 1), 39 moderate myopes (Group 2), 41 high myopes (Group 3), and 20 generally healthy controls (Group 4) using an RTVue-100 instrument (Optovue Incorporated). The RTVue software version 6.11 was used to calculate the optic disc parameters based on the LC morphology markers we designed. Results: Length of the line connecting the flanking edges of Bruch’s membrane, maximum LC depth, depth of the LC insertion, and length of the line connecting the margins of LC insertion were statistically significantly greater (p < 0.05) in patients than in controls. In addition, we found these characteristics to significantly increase with an increase in severity of myopia. Conclusion: The lamina cribrosa is an important ocular structure and warrants further research for better understanding the pathogenesis of and prophylaxis against myopia. Keywords: myopia, lamina cribrosa, optical coherence tomography
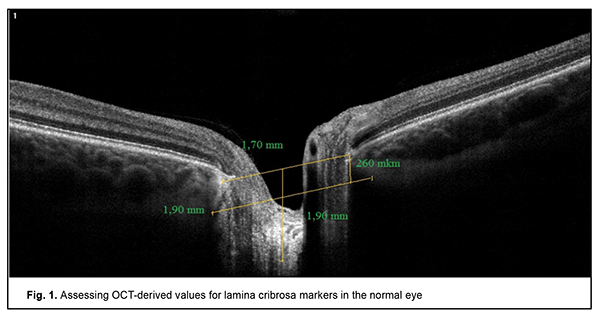
Introduction The lamina cribrosa is an important ocular structure through which the retinal ganglion cell axons and retinal blood vessels pass. Advances in imaging techniques, particularly optical coherence tomography (OCT), allowed for non-invasive research on the cribriform plate and optic disk. Before the use of OCT, the pathological changes of highly myopic eyes in human could only be studied in enucleated globes and ocular structures were measured histomorphometrically [1]. There have been a number of reports on studies (mostly in patients with glaucoma) on the state of the cribriform plate using various OCT modalities such as adaptive optics scanning laser ophthalmoscopy (AO-SLO) [2], swept source OCT (SS-OCT) [3, 4, 6] and enhanced depth imaging-optical coherence tomography (EDI-OCT) [5]. As myopia progresses, the eye stretches and this leads to degenerative conditions developing with age in the posterior pole. Unfortunately, OCT apparatuses with an EDI-OCT mode are poorly available in Ukraine. In addition, to the best of our knowledge, there have been no reports on studies on the state of the lamina cribrosa in patients with various degrees of myopia. Understanding the pathogenesis of changes in the lamina cribrosa in myopic eyes will lead to the development of advanced treatments and early prevention strategies. The purpose of the study was to investigate morphological characteristics of the lamina cribrosa in mild myopes, moderate myopes, and severe myopes versus generally healthy individuals (controls). Material and Methods One hundred and twenty patients (204 eyes; 64 women (53.3%) and 56 men (46.7%)) with mild, moderate or severe myopia were supervised and examined at the municipal healthcare institution (Regional Clinical Hospital for Emergency and Disaster Medicine) and Zir medical center by the staff of Ophthalmology Department of Kharkiv National Medical University. The control group comprised 20 age- and gender-matched generally healthy volunteers (11 women and 9 men). All study participants were of working age and between 18 and 45 years. The mean age of patients was 31.5 ±13.5 years. Fourier-Domain OCT of the outer portion of the optic disc was conducted using an RTVue-100 instrument (Optovue Incorporated, Fremont, CA). The RTVue software version 6.11 was used to calculate the optic disc parameters based on the LC morphology markers we designed [1, 2, 3]. This lamina cribrosa scanning methodology may be adapted for widely available OCT systems, and does not require specialized devices, additional software and/or additional equipment to be installed on or attached to the OCT system. Fig. 1 presents an example for OCT-assisted assessment of the LC morphology markers.
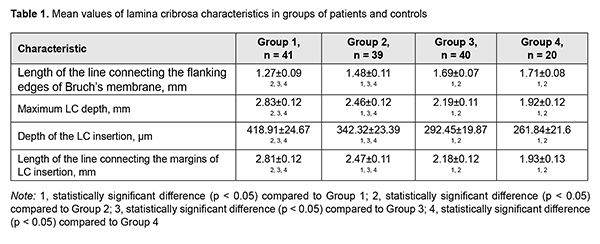
The study was performed in compliance with bioethical principles adopted by the First National Congress on Bioethics (Ukraine, Kyiv, 2001) and approved by a local Bioethics Committee of the Kharkiv National Medical University. Patients were divided into three groups based on the severity of myopia: Group 1 of 41 high myopes (19 women [(47.06 ± 12.11) %] and 22 men [(52.94 ± 12.11) %]); Group 2 of 39 moderate myopes (18 women [(46.67 ± 12.88)%] and 21 men [(53.33 ± 12.88) %]); and Group 3 of 40 low myopes (23 women [(60.71 ± 9.23)%] and 17 men [(39.29 ± 9.23)%). Group 4 (controls) comprised 20 generally healthy individuals (40 eyes; 11 women [(58.33±14.23)%] and 17 men [(41.67±14.23)%). The RTVue software version 6.11 was used to calculate lamina cribrosa characteristics for all study patients based on the LC morphology markers we designed. Findings of previous studies [2, 3, 4] on the structure of the lamina cribrosa have been taken in account to develop markers assisting in identification of the structure and morphological features of the lamina cribrosa in patients with various degrees of myopia. The developed markers were adapted for the OCT apparatus and software that had been authorized for use in Ukraine. Length of the line connecting the flanking edges of Bruch’s membrane, maximum LC depth, depth of the LC insertion, and length of the line connecting the margins of LC insertion were assessed. Results and Discussion Table 1 presents mean index values for study groups. There was a significant difference in LC characteristics in patients of Groups 1 and 2 versus controls (Group 4). In addition, there was a significant difference in LC characteristics between groups of patients with various degrees of myopia (Group 1 vs Group 2 vs Group 3).
Mean length of the line connecting the flanking edges of Bruch’s membrane in high myopes and moderate myopes was almost 25% and 14%, respectively, longer than in controls (1.71 ± 0.08 mm). Maximum LC depth in high myopes and moderate myopes was 47% and 28%, respectively, deeper than in controls. Depth of the LC insertion and mean LC depth in high myopes and moderate myopes were 1.5-fold and 1.3-fold greater than in controls. As there have been few studies examining the state of the lamina cribrosa in myopia, mostly associated with glaucoma [7, 8, 9], investigating changes in the morphology of the lamina cribrosa in patients varying in severity of myopia is deemed to be important. Conclusion Changes in characteristics of the LC were observed with an increase in the severity of myopia. High myopes exhibited the most substantial changes compared to normal controls. Early diagnosis of changes in optic disc and lamina cribrosa morphology will facilitate early treatments aimed at preventing vascular and visual dysfunction and disability. References 1.Ng DS, Cheung CY, Luk FO et al. Advances of optical coherence tomography in myopia and pathologic myopia. Eye (Lond). 2016;30(7):901–916. doi:10.1038/eye.2016.47. 2.Akagi T, Hangai M, Takayama K et al. Reproducibility of In-Vivo OCT Measured Three-Dimensional Human Lamina Cribrosa Microarchitecture. Invest Ophthalmol Vis Sci. 2012;53(7):4111–4119. 3.Nuyen B, Mansouri K, Weinreb RN. Imaging of the Lamina Cribrosa using Swept-Source Optical Coherence Tomography. J Curr Glaucoma Pract. 2012 Sep-Dec;6(3):113-9. doi: 10.5005/jp-journals-10008-1117. 4.Lee EJ, Kim TW, Weinreb RN, Park KH, Kim SH, Kim DM. Visualization of the lamina cribrosa using enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol. 2011;152:87–95.e1. 5.Park SC, Kiumehr S, Teng CC et al. Horizontal Central Ridge of the Lamina Cribrosa and Regional Differences in Laminar Insertion in Healthy Subjects. Invest Ophthalmol Vis Sci. 2012; 53:1610-1616. doi:10.1167/iovs.11-7577. 6.Omodaka K, Takahashi S, Matsumoto A et al. Clinical Factors Associated with Lamina Cribrosa Thickness in Patients with Glaucoma, as Measured with Swept Source Optical Coherence Tomography. PLoS One. 2016; Apr 21;11(4):e0153707. doi: 10.1371/journal.pone.0153707. 7.Xiao H, Xu XY, Zhong YM, Liu X. Age related changes of the central lamina cribrosa thickness, depth and prelaminar tissue in healthy Chinese subjects. Int J Ophthalmol. 2018;11(11):1842–1847. doi: 10.18240/ijo.2018.11.17. 8.Tan NYQ, Tham Y-C, Thakku SG et al. Changes in the Anterior Lamina Cribrosa Morphology with Glaucoma Severity. Sci Rep. 2019; 9: 6612. doi:10.1038/s41598-019-42649-1. 9.Miki A, Ikuno Y, Asai T et al. Defects of the Lamina Cribrosa in High Myopia and Glaucoma. PLoS ONE. 2015;10(9):e0137909. doi:10.1371/journal.pone.0137909.
The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|