J.ophthalmol.(Ukraine).2020;1:28-31.
|
http://doi.org/10.31288/oftalmolzh202012831 Received: 16 December 2019; Published on-line: 21 February 2020 Surgical technique for persistent macular holes with application of the leucocyte and platelet rich plasma obtained with the Ycellbio system D.V. Zhmuryk, Cand Sc (Med); M.V. Miliienko; O.G. Volochanska Kyiv Municipal Clinical Eye Hospital “Eye Microsurgery Center”; Kyiv (Ukraine) E-mail: miliienko.m@gmail.com TO CITE THIS ARTICLE: Zhmuryk DV, Miliienko MV, Volochanska OG. Surgical technique for persistent macular holes with application of the leucocyte and platelet rich plasma obtained with the Ycellbio system. J.ophthalmol.(Ukraine).2020;1:28-31. http://doi.org/10.31288/oftalmolzh202012831
Background: Treatment of persistent macular holes (MH) remains a challenge in spite of recent advances in macular surgery. In re-surgery in case of persistent MH, there is lack of internal limiting membrane (ILM) tissue for adequate MH closure. Application of leucocyte and platelet rich plasma (PRP) to the macular hole is one of the various techniques that may be used to improve the success rate of surgery for persistent MHs. The use of the funnel-shaped Ycellbio system with a red blood cell (RBC) control lever provides easy and effective PRP extraction process. Purpose: To assess the efficacy of surgical treatment for persistent MHs with application of the PRP obtained with YCELLBIO PRP preparation kit to the MH area. Material and Methods: Ten patients with eyes diagnosed with persistent MH were under observation at the Kyiv Municipal Clinical Eye Hospital “Eye Microsurgery Center” from September 2018 to February 2019. Before re-surgery, mean macular hole size was 894 ± 115 ?m, and best-corrected visual acuity varied from 0.03 to 0.1. PRP was obtained using a fixed-angle rotor centrifuge at 3600 rpm with an YCELLBIO PRP preparation kit. Each patient received a closed subtotal vitrectomy with application of the PRP to MH area and subsequent vitreous endotamponade with 20% С3F8. Results: The surgical procedure for persistent MH promoted anatomical closure in 9/10 eyes (9/10 patients). In addition, postoperative BCVA was 0.1 or better in 8/10 patients, and worse than 0.1 in 2/10 patients. Conclusion: Application of the PRP obtained with the Ycellbio system is an effective method of treatment and may be considered as a method of choice for surgical treatment of persistent macular holes. Keywords: macular hole, leucocyte and platelet rich plasma маса, Ycellibiо
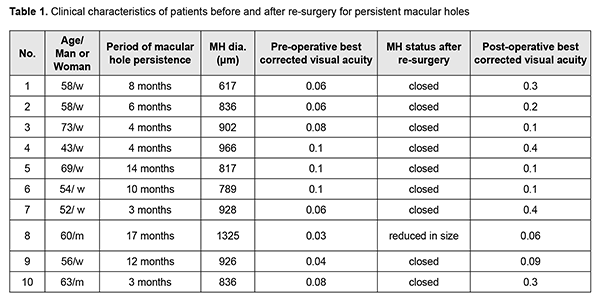
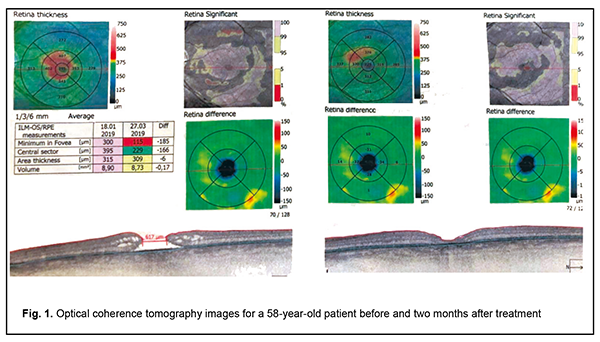
Introduction Although macular holes (MHs) were first described by Knapp as early as 1869, the condition was considered to be untreatable until 1991. In 1971, Machemer developed closed, pars plana vitrectomy (CV), thus improving the prospects for successful treatment of MHs [1]. The surgery to repair MHs was first reported by Kelly and Wendel [2] who described the clinical use of CV with subsequent facedown gas tamponade to help or stabilize vision. This approach was based on releasing tangential vitreous traction as suggested by the Gass’ theory of MH formation. In 30 (58%) of 52 patients, they were able to reattach successfully the detached macula with their surgical procedure, and the overall success rate for improved vision postoperatively was 42%. MH surgery has advanced significantly in recent decades. The use of the inverted internal limiting membrane (ILM) flap technique for large MHs [9] has contributed to an improvement in MH surgery success rate, with MH closure seen in as much as 98% of patients [3]. Treatment of persistent macular holes, however, remains a challenge. MH surgery failures are most commonly associated with treatment of MHs larger than 400 ?m, high myopia, late MH surgery, etc. In re-surgery in case of persistent MH, there is lack of ILM tissue for adequate MH closure. Application of “the biological glue”, leucocyte and platelet rich plasma (PRP), to the macular hole is one of the various techniques that may be used to improve the success rate of surgery for persistent MH. This approach facilitates fibroglial cell proliferation for MH closure [4]. PRP may be easily prepared using an YCELLBIO PRP preparation kit (Ycellbio MEDICAL Co., Seoul, Douth Korea) that has a unique design and is supplied with a red blood cell (RBC) control lever to facilitate the PRP extraction process, minimizing the amount of RBCs mixed in PRP. The purpose of the study was to assess the efficacy of surgical treatment for persistent MHs with application of the PRP obtained with YCELLBIO PRP preparation kit to the MH area. The purpose of the study was to assess the efficacy of surgical treatment for persistent MHs by applying the leucocyte and platelet rich plasma obtained with YCELLBIO PRP preparation kit. Material and Methods Ten patients with eyes diagnosed with persistent MH were under observation at the Kyiv Municipal Clinical Eye Hospital “Eye Microsurgery Center” from September 2018 to February 2019. Previously, all these had primary MH surgery. In each case, cataract phacoemulsification was conducted with intraocular lens implantation, vitrectomy, ILM peeling and subsequent air and gas tamponade. Before re-surgery, mean macular hole size was 894 ± 115 ?m, and best-corrected visual acuity varied from 0.03 to 0.1 (Table 1). Conventional diagnostic procedures (visual acuity, perimetry and intraocular pressure measurements), optical coherence tomography (OCT) and a coagulogram were performed on each patient. PRP was obtained using a fixed-angle rotor centrifuge at 3600 rpm with an YCELLBIO PRP preparation kit (Ycellbio MEDICAL Co., Seoul, Douth Korea) that has a unique design and is supplied with an RBC control lever to facilitate the PRP extraction process, minimizing the amount of RBCs mixed in PRP.
PRP preparation technique Blood (13.5-14.0 mL) was collected from the cubital vein into the YCELLBIO tube, mixed with anticoagulant (sodium citrate), and centrifuged in a fixed-angle rotor centrifuge for 4 min at 3600 rpm. Using the control lever in the bottom of the Ycellbio kit®, some PRP containing leucocytes was raised to the mid-line to minimize the amount of RBC mixed in PRP. Operation technique Local subtenon anesthesia was administered. Vitrectomy was performed under control of operating microscope OMS-800 OFFISS (Topcon, Japan) and using 25-G and 27-G tools. An injection of betamethasone dipropionate into the vitreous was used to enhance better visualization of the residual vitreous. A cannula was used to introduce some PRP (0.05 mL) into the eye through the vitrectomy port, and the macular site was exposed to the PRP under air for 3 minutes. Subsequently, vitreous endotamponade with 20% С3F8 was performed. Results The surgical procedure for persistent MH promoted anatomical closure in 9 eyes (9 patients). In addition, postoperative BCVA was 0.1 or better in 8 patients, and worse than 0.1 in 2 patients (Table 1). In the case with no anatomical closure after surgery, revision was performed with subsequent silicone oil tamponade. Complications included ocular hypertension that developed in 3 cases. In all these 3 cases, it was successfully treated with hypotensive eye drops administered for 3 to 5 days. Discussion The study deals with resurgery for persistent MHs. Since there is lack of ILM for adequate MH closure in these cases, treatment of persistent macular holes is still a challenge for a vitreoretinal surgeon in spite of recent advances in macular surgery. Chen and Yang [5] have reported on the clinical results of lens capsular flap transplantation in refractory MH. They created a flap using the autologous anterior or posterior lens capsule (i.e., the connective tissue) that may facilitate the development of proliferation and subsequent MH closure. Macular hole closure was achieved in 15 eyes (75%). The common characteristics for the eyes without closed holes was that all of the five eyes has a non-fibrotic posterior capsule or that only a sparse curled posterior capsular flap could be obtained, which could not properly fill the hole in one place. In the follow-up OCT, the flap appeared dislodged after the operation and no flap was visible in the OCT image in the two eyes without closed holes.
Previously, we have reported on a short-term PFCL tamponade in an attempt to improve the success rate of this technique. The methodology, however, is difficult to follow, and the technique requires certain experience [6]. The application of PRP in MH repair is substantiated by its features, since PRP contains high levels of platelet-derived growth factor and transforming growth factor-beta and modulates the fibroglial proliferation in the MH area, facilitating effective MH closure [7]. In addition, when transformed into fibrin, plasma fibrinogen provides proliferation and differentiation of cells in the foveal area [8]. The methodology, however, has not become a widespread practice, since the anatomical success did not contribute to an improvement in visual function. Contrary to this, a recent study by Shkvorchenko et al [9] demonstrated that the use of PRP as an adjunct provided high anatomic and functional success in re-surgery for persistent MHs that were deemed of low potential for success with conventional surgical treatment approaches. These findings are in agreement with ours. The use of the funnel-shaped Ycellbio system with an RBC control lever contributed to easy, safe and effective PRP extraction process. The only complication we observed in the MH surgery performed with the use of PRP obtained with the Ycellbio system was ocular hypertension that is common for gas tamponade. Conclusion Application of the leucocyte and platelet rich plasma obtained with the Ycellbio system is an effective method of treatment and may be considered as a method of choice for surgical treatment of persistent macular holes. In our case series, the surgical procedure for persistent MH promoted anatomical closure in 9/10 eyes (9 patients). In addition, postoperative BCVA was 0.1 or better in 8/10 patients.
References 1.Machemer R, Buettner H, Norton EW, Parel JM. Vitrectomy: a pars plana approach. Trans Am Acad Ophthalmol Otolaryngol. 1971; 75(4): 813-20. 2.Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol. 1991; 109(5):654-9. 3.Michalewska Z, Michalewski J, Adelman RA, et al . Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010; 117(10):2018-25. 4.Cheung CMG, Munshi V, Mughal S, et al. Anatomical success rate of macular hole surgery with autologous platelet without internal-limiting membrane peeling. Eye. 2005; 19(11):1191-3. 5.Chen A-N, Yang C-M. Lens capsular flap transplantation in the management of refractory macular hole from multiple etiologies. Retina. 2016; 36(1):163-70. 6.D.V. Zhmuryk, M.V. Miliienko. [Optimizing tactics for management of patients with persistent large macular holes]. Oftalmologiia. Vostochnaia Evropa. 2017;7(2):181-6. Russian. 7.Dimopoulos S, William A, Voykov B, et al. Anatomical and visual outcomes of autologous thrombocyte serum concentrate in the treatment of persistent full-thickness idiopathic macular hole after ILM peeling with brilliant blue G and membrane blue dual. Acta Ophthalmol. 2017; 95(5):429-30. 8.Gaudric A, Massin P, Paques M, et al. Autologous platelet concentrate for the treatment of full-thickness macular holes. Graefes Arch Clin Exp Ophthalmol. 1995; 233(9). 549-54. 9.Shkvorchenko DO, Zakharov VD, Krupina EA, et al. [Surgical treatment of macular holes with application of platelet-rich plasma]. Oftalmokhirurgiia. 2017;(3):27-30. Russian.
The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|