J.ophthalmol.(Ukraine).2019;6:70-75.
|
http://doi.org/10.31288/oftalmolzh201967075 Received: 17 October 2019; Published on-line: 08 January 2020 A case report of uveitis with ocular hypertension N. V. Konovalova, Dr. Sc. (Med.); V. V. Savko, Dr. Sc. (Med.); N. I. Khramenko, Cand. Sc. (Med.); O. V. Guzun, Cand. Sc. (Med.); S. B. Slobodianyk, Cand. Sc. (Med.); Iu. A. Zhuravok, Cand. Sc. (Med.); V. V. Savko, Jr., Cand. Sc. (Med.) SI "The Filatov Institute of Eye Diseases and Tissue Therapy of the National Academy of Medical Sciences of Ukraine"; Odesa (Ukraine) E-mail: kvnkonovalova@gmail.com TO CITE THIS ARTICLE: Konovalova NV, Savko VV, Khramenko NI, Guzun OV, Slobodianyk SB, Zhuravok IuA, Savko VV, Jr. A case report of uveitis with ocular hypertension. J.ophthalmol.(Ukraine).2019;6:70-75. http://doi.org/10.31288/oftalmolzh201967075 Based on a clinical case, we analyzed the characteristics of diagnosis, course, and treatment of uveitis in the presence of ocular hypertension. Keywords: uveitis, ocular hypertension, prostaglandin analogues
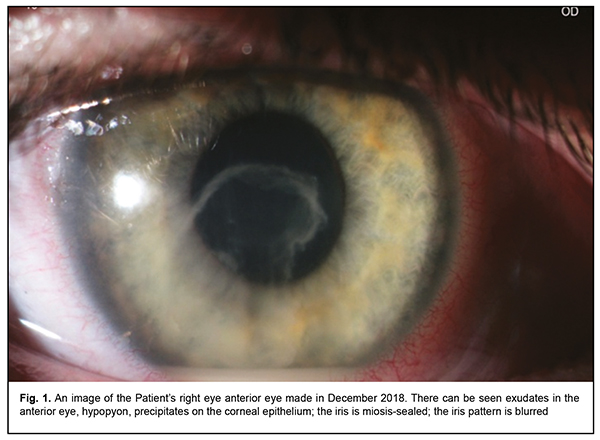
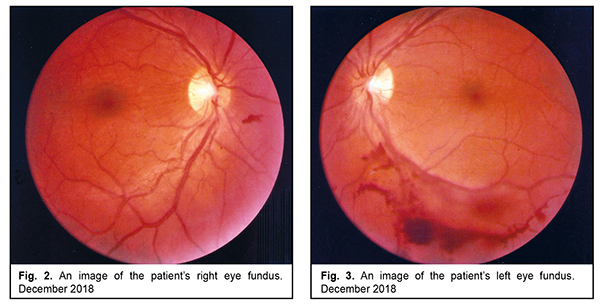
Introduction Streptococcal uveitis is one of the most severe inflammatory diseases of the eye. It often affects young working-age people and is characterized by high rates of complications which, in 10-15 % of cases, lead to vision impairment or blindness of an affected eye with a fellow eye, often involved in the process. This defines the social significance of the disease [1, 2, 3]. Treatment of severe forms of uveitis is a challenging task, especially when inflammation is accompanied by secondary hypertension. An increase of intraocular pressure (IOP) causes a deformation of the lamina cribrosa. Impression of the lamina cribrosa followed by deformation of the vascular bundle unbalances intraocular and perfusion pressures with a decrease of the latter and causes atherosclerotic changes of vessels. Disorders in hemodynamics and retinal perfusions and ischemia are risk factors of retinal vein occlusion and retinal vasculitis. A decrease in perfusion pressure in the pool of posterior small arterial vessels is a mechanism of anterior ischemic neuropathy. Ischemia leads to cell loss, including that of axons, myelin sheaths, and glial cells. To protect from irreversible changes and prevent apoptosis, direct and indirect neuroprotection is required [4, 9]. Takeuchi M. And colleagues have analyzed the changes in IOP and inflammation in the patients with uveitis-associated ocular hypertension treated using latanoprost [7, 8, 11]. The authors have reported that preventive local antihypertensive therapy reduces 4.5-fold the rates of post-uveal glaucoma in patients with chronic uveitis and persistent ocular hypertension and prevents from developing secondary glaucoma in patients with transient ocular hypertension. Indirect neuroprotection is associated with the effective hypotensive action; it sustains the viability and prevents from apoptosis of retinal ganglion cell. A direct anti-apoptosis effect of latanoprost is associated with inhibiting caspase-3, an apoptosis-inducing enzyme, through the activation of protein kinases. The secondary neuroprotective action is associated with the effect on the blood flow in the optic disc region: protection of the posterior segment (neuroprotection) and protection of the anterior segment (epithelial protection) [4, 6, 8]. Retinal vasculitis is a characteristic of rheumatoid lesion of the retina and requires neuroprotection. Ischemia leads to cell loss, including that of axons, myelin sheaths, and glial cells. A risk factor of neuroretinitis is hypoperfusion in posterior ciliary arteries. In vascular diseases of the retina and optic nerve, these are prostaglandins and their analogs that reduce intraocular pressure most effectively [4, 5, 6, 10]. The purpose of the present paper was to describe the characteristics of diagnosis, course, and treatment of streptococcal eye lesion (uveitis with ocular hypertension) with the use of latanoprost prostaglandin analog on a follow-up clinical example. Material and Methods At Inflammatory Eye Disease Department of the Filatov Institute, we followed up a 21-year-old Patient R., diagnosed with chronic iridocyclitis and ocular hypertension with retinal vasculitis in both eyes. Ophthalmic examination included visual acuity testing, IOP measurements, biomicroscopy, ophthalmoscopy, phosphene threshold current, ocular rheography, perimetry, optical coherence tomography (OCT), OCT-angiography, fluorescein angiography (FAG), photo recording. A REOCOM rheograph (Kharkiv, Ukraine) was used to perform computer ocular rheography (ORG) and calculate the Rheographic Quotient, RQ (‰), a parameter indicating a volume of blood which enters the eye within a cardiac cycle and tonic properties of large (? 1/Т) and small (? 2/Т) vessels. Results In June 2018, the Patient had tonsillitis; three weeks later, in July, the patient started complaining of photophobia, eye-watering, impaired vision, and pain in both eyes. At the place of residence, she was diagnosed with iridocyclitis and prescribed a two-week course of standard anti-inflammatory therapy. Treatment made it possible to jugulate iridocyclitis in both eyes. The follow-up visit at the place of residence was in November 2018. The patient with recurrent chronic iridocyclitis in the right eye was referred to the Filatov Institute of Eye Diseases and Tissue Therapy where she was diagnosed with chronic iridocyclitis with ocular hypertension (an acute stage in the right eye; unstable remission in the left eye). Retinal vasculitis was in both eyes. Diagnostic findings Visual acuity. OD: best corrected visual acuity (BCVA) = 0.4; Sph = -1.0, D = 0.7; OS: BCVA = 0.5, Sph = -1.0; D = 0.7. IOP by Maklakov was 28 mm Hg and 27 mm Hg in the right and left eyes, respectively. The corneal thickness was 532 µm and 529 µm in the right and left eyes, respectively. Refraction was myopia -1.0 D in both eyes. The patient was found healthy by a dentist; a consultation by an otorhinolaryngologist showed nasal septal deviation, chronic vasomotor rhinitis, and left-sided maxillary sinusitis. Nose culture revealed Group A beta-hemolytic streptococcus. Signs. Right eye: exudates in the anterior eye; hypopyon; precipitates on the corneal epithelium; mild corneal edema; the miosis-sealed iris; blurred iris pattern (Fig. 1). In the vitreous, there were floaters, destruction of the destroyed fiber suspension, exudation flakes. Ophthalmoscopy showed the pale pink optic disk with a sharp contour; the fundus arteries were constricted and tortuous and the veins were full-blooded and tense. We noted a small longitudinal hemorrhage downwards from the optic disc, sized 1/8 of the disc diameter, and the folded retina (Fig. 2).
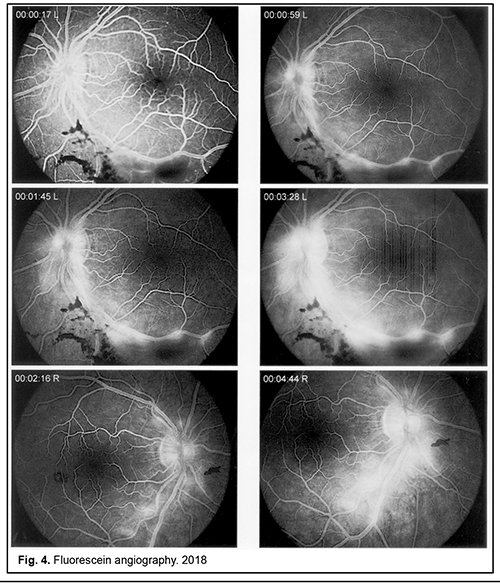
Left eye: we observed that the cornea was transparent, spherical, and smooth with mild corneal edema and pigment remnants on the anterior lens capsule. In the vitreous, there were floaters and fine-grain destruction of the fiber suspension. Ophthalmoscopy showed the pale pink optic disc with a sharp contour. Multiform hemorrhages of various intensity could be seen along the inferior temporal branch of the central retinal vein and retinal edema was detected along vessels. The veins were tense and full-blooded with permeated transudate along the vessel wall (Fig. 3). Based on the examination, the patient was diagnosed with anterior iridocyclitis with ocular hypertension and retinal vasculitis in both eyes; an acute stage in the right eye and unstable remission in the left eye. The patient was performed FAG (Fig. 4), which showed that: the right eye had the optic disc with no abnormalities; there could be seen arterial tortuosity and side-wall permeation in both superior and anterior branches of the central retinal vein, moniliform dilation of arteries, exudation along the veins, and hemorrhages outwards from the optic disc. Reflexes were blurred in the macular area.
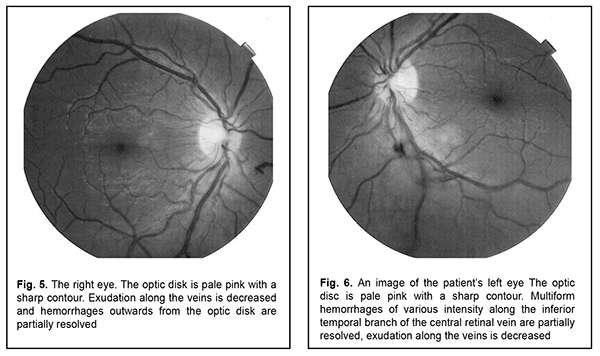
The left eye had: beads-like current of transudate from the disk and along the inferior temporal branch of the central retinal vein; various intensity multiform hemorrhages along vessels in the arterial and venous phase. Pathologic reflexes were observed in the macular area. Treatment for the patient included a traditional therapy with methotrexate, 25 mg per week, local corticosteroids (0.5 ml, parabulbarly), low molecular heparin, vasoprotectives, non-steroidal anti-inflammatory drugs (ETOL FORT, per os, 1 pill twice a day), antisensitizer (LAROTODIN, per os, 1 pill once a day), electrophoresis with anti-inflammatory drugs (FLOXAL, INDOCOLLYRE). A prostaglandin analog was prescribed due to secondary ocular hypertension. Disorders in hemodynamics and retinal perfusion, as well as ischemia, are risk factors of retinal vein occlusion. With the purpose to reduce intraocular pressure for direct and indirect neuroprotection we chose MONOPROST, 1 drop once a day, the major mechanism of which lies in the capacity to increase the uveoscleral outflow. Treatment outcome BCVA=1.0; IOP = 18.0 mm Hg in both eyes. Visual field was without alterations. Precipitates on the corneal epithelium were resolved. No corneal edema was noted. Exudates in the anterior chamber were resolved. In the vitreous, there was fine-grain destruction of the fiber suspension. The optic disk was pale pink with sharp contours; hemorrhages and edema along the vessels were partially resolved; the reflexes became clearer in the macular area. The follow-up visit was in February 2019. The patient was diagnosed with episcleritis in both eyes; chronic iridocyclitis in remission; retinal vasculitis. Visual acuity: OD: BCVA=0.7, Sph = -0.1, D=1.2; OS: BCVA=0.5, Sph = -0.1, D=1.0. IOP by Maklakov was 21.0 mm Hg in both eyes (MONOPROST instillations, 1 drop once a day). Refraction: myopia -1.0 D in both eyes. The patient was found healthy by a dentist; a consultation by an otorhinolaryngologist showed nasal septal deviation, chronic vasomotor rhinitis. Signs. Visual examination showed that both eyes were hyperemic due to sectoral edema and inflammation of the conjunctiva in the outer upper quadrant; there was conjunctival edema, mixed hyperemia of conjunctival vessels, and a small scleral staphyloma. We detected the perspired corneal epithelium and no synechiae; remnants of the pigment could be seen on the anterior lens capsule. Floaters in the vitreous were in a form of separated fibrils. Ophthalmoscopy in the right eye showed that the optic disk was without abnormalities; arterial tortuosity was detected in both superior and inferior temporal branches of the central retinal artery with moniliform dilation of arteries; exudation along the veins and hemorrhages outwards from the optic disk was partially resolved (Fig. 5).
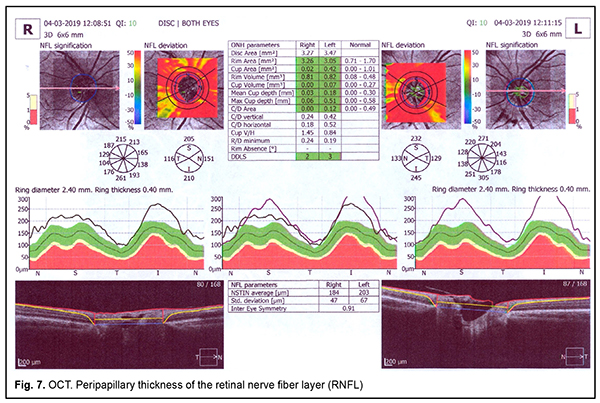
The left eye had the pale pink optic disc with sharp contours; multiform hemorrhages were partially resolved along the inferior temporal branch of the central retinal vein; exudation along the vessels decreased (Fig. 6). Special examinations. At the patient’s admission, RQ was 1.4‰ and 2.0 ‰ in the right and left eyes, respectively, which was lower than the RQ age normal ranges by 60% and 42.8%, respectively. We also noted an increase in the tonic properties of small vessels by 34% in both eyes. At discharge, RQ decreased by 14% and 50% in the right and left eye, respectively, which indirectly reflects a decreased inflammation in the uvea and requires a dedystrophic therapy in the intercurrent period. Biomicroscopy showed a decreased relative count of natural killers (CD16) as compared to the norm, 9% vs. 10-20%, respectively, and decreased neutrophil phagocytosis, 37% vs. 40-80% in the norm, which testifies to the decreased activity in controlling an intracellular infection and the immune system compromised in controlling an infectious agent. We noted increased levels of the expression of molecular markers of peripheral blood lymphocyte activation (CD5=21%, CD25=20%, CD54=29%) which was 2.0-2.05-fold higher than those in the norm and reflected a compensatory activation of the immune system for increasing not only intercellular adhesion and cooperation but cell apoptosis. The Golden Standard of retinal vasculature assessment is FAG; however, it does not allow visualizing intraretinal vascular plexuses separately. OCT-angiography makes it possible to visualize four capillary plexuses and to perform quantitative analyses of microcirculation and to calculate the density of the capillary net and the zones with the absence of capillary perfusion. OCT-angiography is a more sensitive diagnostic technique for macular capillary perfusion as compared with FAG and makes it possible to reveal initial signs of ischemic maculopathy before they can be visualized by FAG or screened due to hemorrhages. OCT-angiography in the right eye showed the extent of the foveolar avascular zone and the presence of zones without capillary perfusion in the region of the inferior temporal arcade with the macular area involved in the superficial and deep capillary plexuses. OCT-angiography in the left eye showed a decreased density of the perifoveolar capillary net with local portions of ischemia in the superficial and deep capillary plexuses. OCT revealed several structural changes as well. Nevertheless, it is important to bear in mind that the presence of uveitis is the major interfering factor when assessing the retinal nerve fiber layer (RNFL) thickness. Thus, mean RNFL values were 184 µm and 203 µm in the right and left eyes, respectively, (Fig. 7). D. B. Moore and colleagues have reported on the significantly thickened RNFL in patients with active uveitis, which is associated with the breakdown of the blood-retinal barrier and increased production of prostaglandin analogs [5. 11]. RNFL measurements can make it easier to detect signs of damage before the optic disc and the visual field are altered and, consequently, determine a subgroup which requires more active treatment [11]. When inflammation remits, the retinal thickness decreases with a reduction of RNFL thickness, which is consistent with our patient’s findings. Thus, after 4 months, the mean RNFL was 163 µm and 172 µm in the right and left eyes, respectively.
In addition, OCT has also become a standard to confirm a diagnosis of macular edema. Based on examination, the patient had severe uveitis and ocular hypertension and was treated using IOP-reducing. Uveitis, however, was not associated with glaucomatous lesion of the retina and our findings are in accordance with similar results of other authors [11]. Conclusions First, a comprehensive complex examination including both morphometric and functional diagnostic methods is required for performing pathogenetically substantiated treatment. Second, to protect from irreversible alterations in the retina and optic nerve, direct and indirect neuroprotection is required that contributes to improving biochemical and regenerative properties of neural cells, stimulating ion-exchanging pumps and receptors, has an anti-edematous action, and inhibits apoptosis. Third, once-a-day latanoprost instillations maintain indirect neuroprotection by the effective hypotensive action; as direct neuroprotection, they sustain the viability and prevent from apoptosis of retinal ganglion cell. Fourth, a combination of antibacterial and immunosuppressive agents, latanoprost and prednisolone make it possible to jugulate inflammation in shorter terms and to achieve stable remission. References: 1.Arbenyeva NS, Chekhova TA, Bratko GV, Chernakh VV. [Comparative analysis of diseases incidence in patients with uveitis]. [The Annual All-Russian Scientific Practical Conference of Young Scientists «Current Problems of Ophthalmology». Abstract book]. M.: Oftalmologiia; 2012: 28-29. In Russian 2.Drozdova EA. [The classification and epidemiology of uveitis]. RMZh. Klinicheskaia Oftalmologiia; 2016;3:155-9. In Russian. 3.Panova IE, Drozdova EA. [Uveitis: Guidance for practitioners]. M.: Meditsinskoie informatsionnoie agenstvo; 2014. 144p. In Russian. 4.Аnamori A, Naka M, Fukuda M et al. Latanoprost protects rat retinal ganglion cells from apoptosis in vitro and in vivo. Exp. Eye Res. 2009;88(3):535–41 5.Asrani S, Moore DB, Jaffe GJ. Paradoxical changes of retinal nerve fiber layer thickness in uveitic glaucoma. JAMA Ophthalmology. 2014; 132(7): 877–80. doi: 10.1001/jamaophthalmol.2014.954. 6.Boltz A, Schmidl D, Weigert G et al. Effect of latanoprost on choroidal blood flow regulation in healthy subjects.Invest. Ophthalmol. Vis. Sci. 2011;52(7):4410–5. 7.Horsley MB, Chen TC. The use of prostaglandin analogs in the uveitis patient. Seminars in Ophthalmology. 2011;26(4-5):285–9. 8.Kurashima H, Watabe H, Sato N et al. Effects of prostaglandin F(2?) analogues on endothelin-1-induced impairment of rabbit ocular blood flow: comparison among tafluprost, travoprost, and latanoprost. Exp. Eye Res. 2010; 91(6):853–9. 9.Markomichelakis NN, Kostakou A, Halkiadakis I, Chalkidou S, Papakonstantinou D, Georgopoulos G. Efficacy and safety of latanoprost in eyes with uveitis glaucoma. Graefe's Arch for Clin and Exp Ophthalmol. 2009;247(6):775–80. 10.Nakanishi Y, Nakamura M, Mukuno H et al. Latanoprost rescues retinal neuro-glial cells from apoptosis by inhibiting caspase-3, which is mediated by p44/p42 mutagen-activated protein kinas. Exp. Eye Res. 2006;83(5):1108–17. 11.Takeuchi M, Kanda T, Taguchi M et al. Evaluation of Efficacy and Safety of Latanoprost/Timolol versus Travoprost/Timolol Fixed Combinations for Ocular Hypertension Associated with Uveitis. Ocul Immunol Inflamm. 2017; Feb 25 (1):105-10.
|