J.ophthalmol.(Ukraine).2019;5:22-26.
|
http://doi.org/10.31288/oftalmolzh201952226 Received: 03 July 2019; Published on-line: 30 October 2019 Neuroophthalmological symptoms of pituitary adenomas with supraparasellar extension K.S. Iegorova, Cand Sc (Med); M.O. Guk, Dr Sc (Med); O.M. Guk, Cand Sc (Med); L.O. Danevych, Cand Sc (Med); D.M. Tsiurupa, Cand Sc (Med); A.O. Mumliev, Cand Sc (Med) Romodanov Neurosurgery Institute; Kyiv (Ukraine) E-mail: iegorova_katya@ukr.net TO CITE THIS ARTICLE: Iegorova KS, Guk MO, Guk OM, Danevych LO, Tsiurupa DM, Mumliev AO. Neuroophthalmological symptoms of pituitary adenomas with supraparasellar extension. J.ophthalmol.(Ukraine).2019;5:22-26. http://doi.org/10.31288/oftalmolzh201952226 Background: Pituitary adenomas (PA) are benign neoplasms that arise from adenohypophysis; they are most common skull base tumors, and account for 12% to15% of all intracranial tumors. In PA with supraparasellar extension, a tumor grows upward, causing chiasmal and lateral cavernous sinus compression. Because prolonged compression of the optic nerve/chiasm complex results in the development of primary descending ONA in 31% to 72% of patients, leading to blindness in 3.5% to 16% of patients, the issue is worthy of attention. Purpose: To investigate neuro-ophthalmological symptoms in pituitary adenomas with a supraparasellar extension before and after treatment. Materials and Methods: This retrospective study included the records of 107 patients who received treatment for pituitary adenomas with a supraparasellar extension at the Romodanov Institute during 2017 to 2018. The main group included 49 patients (98 eyes) who had visual impairments and/or visual field deficits. Patients underwent clinical and neurological, eye and otoneurological examination (including neuroimaging studies) before and after treatment. Results: Visual impairments with the development of markedly asymmetric chiasmal syndrome were most common in the clinical picture, with a severe visual acuity loss (25.5% of eyes) and significant sensitivity loss (39.8% of eyes) in the more affected eye, mild or moderate visual acuity loss and visual field loss in the less affected eye, and development of primary descending optic nerve atrophy in 36 (73.5%) patients. After treatment, visual acuity restored or improved in 57 (58.2%) eyes, and arithmetic mean of the sensitivity loss, the mean defect (MD), improved in 46 (46.9%) eyes (these improvements were significant, p < 0.05). Conclusion: Pituitary adenomas with supraparasellar extension were characterized by the development of visual and oculomotor impairments, which evidenced the presence of various directions of tumor expansion. Visual impairments with the development of markedly asymmetric chiasmal syndrome were most common in the clinical picture. Mean BCVA improved from 0.51±0.04 at baseline to 0.66±0.03 after treatment, and mean overall visual field sensitivity loss improved from 12.11 ± 0.69 dB at baseline to 8.6 ± 0.7 dB after treatment (both improvements were significant, p < 0.05). Keywords: optic nerve atrophy, pituitary adenoma, chiasmal syndrome
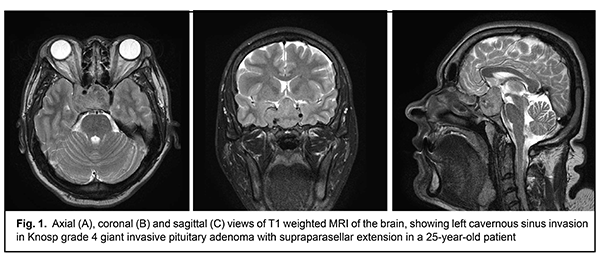
Introduction Pituitary adenomas (PA) are benign neoplasms that arise from adenohypophysis; they are most common skull base tumors, and account for 12% to15% of all intracranial tumors [1, 2]. The clinical picture depends on whether or not the neoplasm is secreting one or more of a variety of hormones, as well as on tumor size, mass effect and extension. In a functioning (i.e., secreting) pituitary adenoma (SPA), a severe clinical disorder or syndrome (acromegaly, Cushing's disease, or hyperprolactinemia) develops, and, therefore, the diagnosis can be made early, when the tumor is small. In a non-secreting pituitary adenoma (NSPA), the early stage is often asymptomatic. In elderly patients, NSPA and prolactinomas may be large and even giant-sized, which causes difficulties in their management [3, 4]. The clinical picture depends on the PA growth direction. The Yasargil classification of 1996 [5] reflects PA growth directions in details and is important in extracellular pituitary adenomas. In pituitary adenomas with a supraparasellar extension, a tumor grows upward, causing chiasmal compression and lateral cavernous sinus (CS) compression (Fig. 1). The Knosp classification of CS invasion [6] is frequently used.
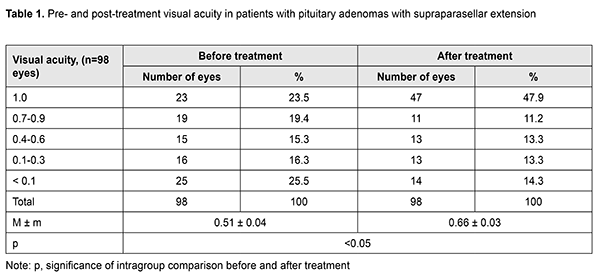
Ocular motility disorders (OMD) are common in PA with CS invasion, occurring in 1.4% to 17% of patients with a conventional disease course and in 57% of patients with pituitary apoplexy [7, 8, 9]. Ocular motility impairments develop as a result of compression or infiltration of the medial wall of the CS by the tumor, with damage to cranial nerve III, IV, and/or VI. Paralytical strabismus is accompanied by diplopia, dizziness, headache, nausea and instability of gait. Oculomotor nerve (CN III) injury is more common than those of CN IV and/or VI, and is evident by ptosis, mydriasis, and limited upward, downward and inward movements of the globe. Anterior visual pathway compression by the neoplasm develops at the ophthalmological phase of the disease and is characterized by a development of chiasmal syndrome, with decreased visual acuity, bitemporal visual field defects, and primary descending optic nerve atrophy (ONA) [1, 10]. Although visual disturbances commonly develop gradually, a sudden substantial visual function loss with the development of OMD can occur in pituitary apoplexy. Because prolonged compression of the optic nerve/chiasm complex results in the development of primary descending ONA in 31% to 72% of patients, leading to blindness in 3.5% to 16% of patients, the issue is worthy of attention [11-14]. The purpose of the study was to investigate neuro-ophthalmological symptoms in pituitary adenomas with a supraparasellar extension before and after treatment. Materials and Methods This retrospective study included the records of 107 patients who received treatment for pituitary adenomas with a supraparasellar extension at the Romodanov Institute during 2017 to 2018. The main group included 49 patients (98 eyes) who had visual impairments (22 women (44.9%) and 27 men (55.1%); age, 21 to 74 years; mean age, 50.3 ± 1.9 years). The inclusion criterion was surgical evidence of pituitary adenoma with a supraparasellar extension as well as the presence of visual impairments (visual loss and/or visual field loss). Patients underwent clinical and neurological, eye, and otoneurological examination (a routine otoneurological examination with assessment of cranial nerve function) before treatment (at day 1 or 2 after admission) and at day 5 to 7 after treatment. Instrumental and laboratory studies were conducted. Neuroimaging included sella turcica X-ray study, magnetic resonance imaging (MRI) of the brain and computed tomography. Neuro-ophthalmic examination included best-corrected visual acuity assessment, biomicroscopy, kinetic and static perimetry, and direct and indirect ophthalmoscopy. Best-corrected visual acuity was classified as normal (1.0), mild impairment (0.7-0.9), moderate impairment (0.4-0.6), severe impairment (0.1-0.3), and very severe impairment (< 0.1). Static automated perimetry (SAP) was performed with the Centerfield 2 Perimeter (Oculus, Wetzlar, Germany). Aside from defect localization, the arithmetic mean of the sensitivity loss, the mean defect (MD), was used to assess visual field loss severity. Visual field loss severity was classified as “no visual field loss” (Grade 0; normal visual field), mild visual field loss (Grade 1; MD, –2 dB to –4 dB), moderate visual field loss (Grade 2; MD, –4 dB to –12 dB), severe visual field loss (Grade 3; MD, –12 dB to –20 dB), and very severe visual field loss (Grade 4; MD, worse than –20 dB). The visual field loss was classified as very severe if it was not possible to assess visual fields due to the extremely poor visual function. A chiasmal syndrome was considered symmetric if both eyes had the same grade of visual field loss. In addition, a chiasmal syndrome was considered asymmetric if the difference between eyes in grade of visual field loss severity was 1, and it was considered markedly asymmetric if the difference was 2 or greater. Eye movement limitation in four directions of gaze was scored. Direct and indirect pupil light responses as well as pupil width and symmetry were investigated. Visual acuity was assessed with a diaphragm if there was mydriasis caused by oculomotor nerve palsy. The data were statistically processed using Statistica 6.0 (StatSoft, Tulsa, OK). Results are presented as the mean and standard deviation (M ± SD). Student’s unpaired t test was used to determine differences between independent groups. The level of significance p ? 0.05 was assumed. Results A total of 465 patients with pituitary adenoma underwent surgery during 2014 по 2017. Of these, 107 (23%) had pituitary adenomas with a supraparasellar extension, and were included for the analysis. Of the 107 patients, isolated visual loss and/or visual field defects were found in 42 patients (39.3%). In addition, isolated oculomotor impairments were found in 5 patients (4.7%). Moreover, both visual function loss and oculomotor impairments were found in 7 patients (6.5%). The main group included 49 patients (98 eyes) with visual function loss. Of these, 7 had oculomotor impairments. Pituitary adenomas were hormonally inactive in 42 (85.7%) patients, and prolactin-, and growth hormone-secreting, in 5 (10.2%) and 1 (2%), respectively. Of the 49 patients, 37 (75.5%) had pituitary macroadenomas (with a diameter >15 mm and < 35 mm), and 12 (24.5%) had giant pituitary adenomas. The disease was manifested by visual impairments in 41 (83.6%) patients. Seven (14.3%) patients complained of diplopia. Visual disorders usually developed gradually over one to three years. Ten patients had acute visual function impairment in the presence of sudden headache. Forty-six (93.8%) patients had decreased vision in one or both eyes; in 17 (37%) patients, only one eye had a VA lower than 1.0; in 11 (23.9%), both eyes had a VA lower than 1.0; in 14 (30.4%), one eye had a VA lower than 1.0, and another, a VA lower than 0.1; in 4 (8.7%), both eyes had a VA lower than 0.1. The distribution of visual acuity among the 49 patients (98 eyes) with visual function loss is presented in Table 1.
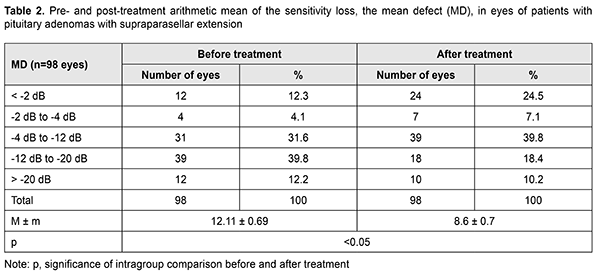
Static perimetry found unilateral or bilateral visual field defects in all these patients. Temporal hemianopia (either complete or partial) only was the commonest field defect (43 eyes; 43.9%), followed by temporal hemianopia with central scotoma (18 eyes; 18.4%), homonymous hemianopia (11 eyes; 11.2%), central scotoma only (7 eyes; 7.2%), residual visual field in the nasal inner quadrant, with a complete loss of central vision (6 eyes; 6.1%), and nasal hemianopia (1 eye; 1%). Visual field was not measurable due to extremely low visual function in 10 (10.2%) eyes. The distribution of loss of sensitivity to light among the 49 patients (98 eyes) with visual function loss is presented in Table 2. Symmetric, asymmetric or markedly asymmetric chiasmal syndrome was found in 12 (24.5%), 11 (22.5%), and 26 (53%) patients, respectively. Ophthalmoscopy found primary descending optic nerve atrophy (ONA) in 36 (73.5%) patients (including 27 patients (54 eyes) with bilateral ONA and 9 patients (9 eyes) with unilateral ONA). In addition, 35 eyes demonstrated retinal angiopathy. Oculomotor disturbances were observed in 7 patients, including 3 with isolated CN VI palsy, 2 with isolated CN III palsy, and 2 with combined CN III, IV, and VI palsies. Of the 49 patients, two were conservatively treated with Dostinex (cabergoline) for prolactinoma, and 47 received transnasal transsphenoidal surgery. BCVA maintained at 1.0 in 23 (23.5%) eyes, restored to 1.0 in 24 (24.5%) eyes, improved in 33 (33.7%) eyes, did not change in 16 (16.3%) eyes, and worsened in 2 (2%) eyes (Table 1), and mean BCVA improved from 0.51±0.04 at baseline to 0.66±0.03 after treatment (the improvement was significant, p < 0.05). In addition, visual field remained normal in 10 (10.2%) eyes, restored to normal in 14 (14.3%) eyes, improved in 32 (32.7%) eyes, did not change in 41 (41.8%) eyes, and worsened in 1 (1%) eyes. Moreover, mean overall visual field sensitivity loss improved significantly from 12.11 ± 0.69 dB at baseline to 8.6±0.7 dB after treatment (p < 0.05; Table 2).
After treatment, five patients demonstrated complete resolution of oculomotor deficits, and two demonstrated incomplete resolution of oculomotor deficits. Therefore, our study revealed patterns of visual impairments and post-treatment changes in these impairments in a large cohort of patients with pituitary adenoma with supraparasellar extension. These patients had not only visual loss and/or visual field loss, but also oculomotor disturbances, which evidenced the presence of various directions of tumor expansion, with compression of the optic nerve/chiasm complex by the suprasellar portion of the mass and lesions in the intracavernous portions of cranial nerves III, IV and VI. Prolonged compression of the optic nerve/chiasm complex results in irreversible ischemic or atrophic changes in the optic nerve. Visual impairments with the development of markedly asymmetric chiasmal syndrome were most common in the clinical picture, with a severe visual acuity loss (25.5% of eyes) and significant sensitivity loss (39.8% of eyes) in the more affected eye, mild or moderate visual acuity loss and visual field loss in the less affected eye, and development of primary descending optic nerve atrophy in 36 (73.5%) patients. After treatment, visual acuity restored or improved in 57 (58.2%) eyes, and arithmetic mean of the sensitivity loss, the mean defect (MD), improved in 46 (46.9%) eyes (these improvements were significant, p < 0.05). Conclusion Pituitary adenomas with supraparasellar extension were characterized by the development of visual and oculomotor impairments, which evidenced the presence of various directions of tumor expansion. Visual impairments with the development of markedly asymmetric chiasmal syndrome were most common in the clinical picture. Mean BCVA improved from 0.51±0.04 at baseline to 0.66±0.03 after treatment, and mean overall visual field sensitivity loss improved from 12.11 ± 0.69 dB at baseline to 8.6 ± 0.7 dB after treatment (both improvements were significant, p < 0.05). References 1.Abouaf L, Vighetto A, Lebas M. Neuro-ophthalmologic exploration in non-functioning pituitary adenoma. Ann Endocrinol (Paris). 2015 Jul;76(3):210-9. doi: 10.1016/j.ando.2015.04.006.. 2.Guk MO. [Diagnosis and comprehensive treatment of hormonally-inactive pituitary adenomas]. Dissertation for Doctor of Medical Sciences. Kyiv. 2017. 3.Kitthaweesin K, Ployprasith C. Ocular manifestations of suprasellar tumors. J Med Assoc Thai. 2008; 91(5):711-5. 4.Ntali G., Wass J.A. Epidemiology, clinical presentation and diagnosis of non-functioning pituitary adenomas. Pituitary. 2018 Apr;21(2):111-118. doi: 10.1007/s11102-018-0869-3. 5.Yasargil M. G. Microsurgery Applied to Neurosurgery. Stuttgart: Thieme, 1969. 6.Knosp E, Steiner E, Kitz K, Matula C. Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery. 1993 Oct;33(4):610-7; discussion 617-8. 7.Kim SH, Lee KC, Kim SH. Cranial nerve palsies accompanying pituitary tumour. J Clin Neurosci. 2007 Dec;14(12):1158-62. 8.Chuang CC, Chen E, Huang YC, Tu PH, Chen YL, Pai PC. Surgical outcome of oculomotor nerve palsy in pituitary adenoma. J Clin Neurosci. 2011 Nov;18(11):1463-8. doi: 10.1016/j.jocn.2011.02.041. 9.Hage R., Eshraghi S.R., Oyesiku N.M., Ioachimescu A.G., Newman N.J., Biousse V., Bruce B.B. Third, fourth, and sixth cranial nerve palsies in pituitary apoplexy. World Neurosurg. 2016 Oct;94:447-452. doi: 10.1016/j.wneu.2016.07.026. 10.Kan E, Kan EK, Atmaca A, Atmaca H, Colak R. Visual field defects in 23 acromegalic patients. Int Ophthalmol. 2013 Oct;33(5):521-5. doi: 10.1007/s10792-013-9733-7. 11.Poon A., McNeill P., Harper A., O’Day J. Patterns of visual loss associated with pituitary macroadenomas. Aust N Z J Ophthalmol. 1995 May;23(2):107-15. 12.Kerrisson JB, Lynn MJ, Baer CA, Newman SA, Biousse V, Newman NJ. Stages of improvement in visual fields after pituitary tumor resection. Am J Ophthalmol. 2000; 130(6): 813-20. 13.Serova NK. [Clinical neuroophthalmology: neurosurgical aspects]. Tver’: Triada; 2011. Russian. 14.Tron EZh. [Visual pathway disorders]. Moscow: Medgiz; 1955. Russian.
The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|