J.ophthalmol.(Ukraine).2019;4:23-27.
|
http://doi.org/10.31288/oftalmolzh201942327 Visualization of intraocular foreign bodies in the projection of the ciliary body by transpalpebral near-infrared transillumination M.B. Kogan, Ophthalmologist, Post-graduate Student; O.S. Zadorozhnyy, Cand Sc (Med), O.S. Petretska, Cand Sc (Med); T.A. Krasnovid, Dr Sc (Med); A.R. Korol, Dr Sc (Med); N.V. Pasyechnikova, Dr Sc (Med), Prof. SI " The Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine”; Odesa (Ukraine) E-mail: mihailkogan2@gmail.com TO CITE THIS ARTICLE: Kogan MB, Zadorozhnyy OS, Petretska OS, Krasnovid TA, Korol AR, Pasyechnikova NV. Visualization of intraocular foreign bodies in the projection of the ciliary body by transpalpebral near-infrared transillumination. J.ophthalmol.(Ukraine).2019;4:23-27. http://doi.org/10.31288/oftalmolzh201942327 Background: Despite advances in intraocular foreign body (IOFB) diagnosis, detecting IOFB is a challenge for the ocular traumatologist. Purpose: To assess the potential of near-infrared transpalpebral transillumination (NIR TPT) for visualization of IOFB in the projection of the ciliary body to the sclera. Materials and Methods: Ten patients (10 eyes) with penetrating globe injuries associated with IOFB were under observation. All patients underwent an X-ray examination with frontal and lateral projections (both with and without using the Komberg-Baltin prosthesis), ultrasound scanning of the anterior eye and posterior eye; ultrasound distant perimetry; metal detector examination; and NIR TPT. Results: In all patients, NIR TPT visualized scleral shadows of the ciliary body pars plicata and pars plana as well as the IOFB shadow. The IOFB was localized in relation to ciliary body structures in all cases. Conclusion: NIR TPT enables non-invasive visualization of IOFBs in the anterior segment, as well as localization of these IOFBs in relation to ciliary body structures in patients with penetrating globe injury. Keywords: penetrating globe injury, intraocular foreign body, infrared radiation, transillumination
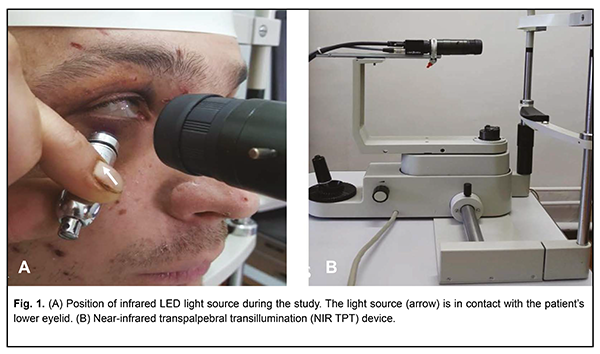
Introduction Ocular trauma is a major cause of monocular blindness and its management is an important public health issue. It is noteworthy that cases of ocular trauma vary in clinical characteristics. Most (80% of) ocular traumas occur in males, the majority of whom are of working age (20 - 40 year) [1, 2]. Penetrating globe injury is a major cause of post-traumatic loss of vision and requires prompt assessment of the severity of damage to ocular structures as well as highly specialized medical care. As much as 18% to 41% of patients with penetrating globe injury have intraocular foreign bodies (IOFB) [3]. Onсe IOFB-related ocular injury has occurred the visual prognosis depends on several factors, including IOFB size, origin, depth and location, as well as the severity of damage to the intraocular structures. Despite advances in IOFB diagnosis, detecting IOFB is a challenge for the ocular traumatologist. Visualizing IOFB in the ciliary body area is especially challenging. Ciliary body IOFBs account for approximately 5% of all intraocular foreign bodies [4, 5]. Currently, computed tomography, X-ray, ultrasound and magnetic resonance imaging (MRI) are the most effective techniques for detecting and localizing IOFBs. Plain X-ray is a conventional diagnostic method allowing the surgeon to detect and subsequently localize an IOFB in most cases. The technique involves frontal and lateral projections. High-density (e.g, metal or stone) foreign bodies can be clearly seen on X-ray films. However, plain X-ray is not always effective in visualizing small (i.e., measuring 1 mm or less) or nonmetallic IOFB. High-resolution computed tomography (CT; with 1.5-mm axial scans) remains the gold standard for the diagnosis of IOFB [6]. Compared to plain X-ray studies, CT provides much more reliable information regarding the size, shape, and localization of the IOFB, and is less invasive. In addition, a CT scan is considered superior to plain X-ray studies in differentiating between tissues of different density and assessing damage to thin bone structures as well as changes in soft tissue structures. CT enables (a) simultaneous visualization of the globe, optic nerve, extraocular muscles, orbital soft tissue and bone structures, and (b) determination of location and depth of IOFB [7]. Drawbacks of CT include separate scanning in axial and coronal planes leading to prolonged scanning time. Artefacts in the form of light and dark stripes reflected from IOFB are commonly seen on CT images of metal fragments. Any fragment measuring less than 3mm is seen as a round-shaped structure on CT images, although its actual shape may be different. In addition, with the use of CT, it is difficult to localize an IOFB in relation to the ciliary body. Moreover, difficulties in identifying nonmetallic IOFB such as wood of plastic have been reported [8]. In traumatic eye injuries, ultrasonography is useful for determining the subsequent treatment strategy. High-resolution ultrasonography enables the detection of intraocular structural disorders like retinal detachment, ciliochoroidal detachment, etc, and identification and localization of metallic and nonmetallic IOFB measuring less than 0.5 mm. A ciliary body IOFB is difficult to identify using the probes designed for exploring the posterior or anterior segments. Echosemiotics of the fragments adjacent to the globe walls is similar to that of the intravitreal fragments, but is more difficult since the image of the fragment commonly merges with the image of the retina, choroid and sclera. In patients with penetrating globe injury, ultrasound studies are associated with the risk of iatrogenic complications [9, 10]. MRI is helpful in identifying and localizing nonmetallic fragments, but is not widely used since magnetic IOFBs are more common, and it is contraindicated to use MRI in cases of magnetic IOFBs. Near-infrared transpalpebral transillumination (NIR TPT) is another technique enabling visualization of the intraocular structures. It allows, e.g., visualization of the shadows of the pars plana, pars plicata and intraocular tumors [11]. As opposed to ultrasonography, NIR TPT enables capturing clear scleral landmarks, which helps to perform surgical procedures in a precise manner. Performing visible-light transillumination of the globe requires the use of a traumatic transcorneal or transscleral illumination pathway. NIR TPT provides a ciliary body image without contact with the globe and enables the accurate estimation of the projection of ciliary body structures to the sclera [12, 13]. The purpose of the study was to assess the potential of NIR TPT for visualization of IOFB in the projection of the ciliary body to the sclera. Materials and Methods The study protocol was approved by the Bioethics Committee of the Filatov Institute. Ten patients (10 eyes) with penetrating globe injuries associated with IOFB were under observation. All patients were males aged 20 to 45 years. They underwent an X-ray examination with frontal and lateral projections (both with and without using the Komberg-Baltin prosthesis), ultrasound scanning of the anterior eye and posterior eye; ultrasound distant perimetry; metal detector examination; and NIR TPT. The NIR TPT equipment used consisted of (1) a wireless infrared light-emitting-diode light source with a dominant wavelength of 940 nm, (2) slit-lamp attachable monochrome video camera (Blackfly®, FLIR Integrated Imaging Solutions Inc., Canada) capable of recording NIR images and video [13]. Since we used the transpalpebral illumination pathway, the study was conducted without the use of topical anesthetics. The transpalpebral illumination study was performed with the patient sitting at the slit lamp (Fig. 1). Images of scleral shadows of the IOFB extending to the pars plicata, pars plana and ora serrata were taken and saved in the computer.
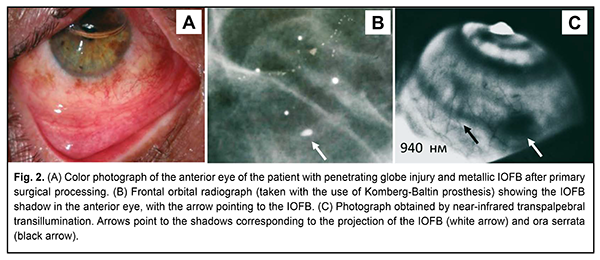
The Aviso ultrasound (Quantel Medical) with a 50-MHz linear probe (axial resolution: 35 µm; lateral resolution: 60 µm) was used to perform ultrasound biomicroscopy with the patient lying on his back, and with the head of the bed raised [1]. In the ultrasound study with the 20-MHz probe designed for exploring the anterior segment, patients were administered topical anesthesias with ophthalmic 0.5% proparacaine hydrochloride (ALCAINE®, SA Alcon-Couvreur NV, Puurs, Belgium), and, subsequently, Vidisic Eye Gel (Dr. GERHARD MANN Chem.-Pharm. Fabrik, Berlin, Germany) as a contact gel. Results In all patients, NIR TPT visualized scleral shadows of ciliary body structures (pars plicata and pars plana) and the IOFB shadow, with the IOFB localized in relation to ciliary body structures. In addition, clear scleral landmarks in the projection of the IOFB were captured. In all cases of radio-opaque foreign bodies in the projection of the ciliary body to the sclera, the IOFB was detected by X-ray and ultrasound. There were difficulties in detecting an IOFB by ultrasound with the probes designed for exploeing the anterior or posterior segments, since in some cases IOFB was located in the area with marginal potential for visualization by ultrasound. NIR TPT detected both radio-opaque and radiolucent (such as wood) foreign bodies, whereas X-ray failed to detect radiolucent IOFBs. Ultrasound with the 20-MHz probe designed for analysis of the anterior segment detected radiolucent IOFBs. In addition, NIR TPT enabled visualization of the scleral shadow of IOFB in the projection of the ciliary body and localization of IOFB in relation to ciliary body structures. Example case A patient received a traumatic right eye injury (Fig. 2) as a result of hammering metal. He underwent primary surgical processing of the penetrating corneal wound, and, thereafter, was referred to the Filatov institute for subsequent treatment. An X-ray examination with the Komberg-Baltin prosthesis and NIR TPT enabled visualization of the IOFB as well as localization of IOFB in relation to ciliary body structures. Since the fragment was small, an ultrasound failed to determine IOFB location. The IOFB was found to be abutting the inner surface of the ciliary body, and its actual dimensions (length, 1 mm; width, 1 mm; and thickness, < 1 mm) were determined after its diascleral removal. The visual acuity in the affected eye was accurate light projection preoperatively, and improved to 0.5 after surgery and active anti-inflammatory therapy.
In addition, in eyes with IOFBs in the lens, NIR TPT enabled (a) visualization of IOFB even in the presence of traumatic cataract and corneal opacity, and (b) localization of IOFB and measurement of its dimensions. Moreover, defects of the sclera and iris were clearly seen in the images obtained with NIR TPT. Discussion Poor IOFB visualization is known to be a major cause for failure in or delayed removal of the IOFB. IOFB visualization may be problematic mostly due to the location of the IOFB (e.g., for the IOFB located in the projection of the ciliary body). In addition, radiolucent or small (< 1.0 mm) IOFBs are especially difficult to identify and localize. Anterior IOFBs may be overlooked due to their shape or location in the anterior chamber angle, under the iris or in the ciliary body area. Therefore, despite advances in the diagnosis of IOFB, detection and localization of anterior IOFBs is still problematic [4, 6, 14]. In penetrating globe injuries with radiolucent IOFBs, the latter are difficult to visualize and accurately localize. Ultrasound provides the most effective approach to IOFB visualization in these patients. It should be noted that, in patients with penetrating globe injury, ultrasound studies are associated with the risk of iatrogenic damage (like prolapse of the retina, choroid and sclera resulting from probe contact with the globe) and additional infection. In addition, ultrasound examination is painful for the patient and associated with patient discomfort. The use of near-infrared LED illumination in NIR TPT enables transillumination not only through the sclera, but even through the patient’s lid, which provides a number of advantages. Compared to ultrasound, NIR TPT is more comfortable and safe for the patient, and requires no use of topical anesthesia. In this way, the possibility of the development of allergic reactions to topical anesthetics is excluded. In addition, absence of physical contact between LED light source and the cornea and sclera allows excluding complications and trauma of these ocular structures, which is especially important in penetrating globe injures. We managed to conduct NIR TPT diagnostic procedures quickly and safely with as little pain and discomfort to the patient as possible in all cases of the study. The use of LED as a source of infrared light simplifies the globe transillumination system, and there is no need for the use of optic fibers to transmit the light radiation to the eye. The LED light source is a compact wireless device that needs no additional infrared filters. One may use infrared LEDs of different wavelengths to achieve better visualization of the globe. With the use of near-infrared light for globe transillumination, there is no glare from bright visible light, which makes the conduct of studies in this patient category easier. The proposed visualization approach enables taking real-time photographs and shooting real-time video of TPT pictures [15]. NIR TPT enables visualization, localization and measurement of the dimensions of ciliary body structures [12, 13]. We believe that NIR TPT methodology can be adapted for intraoperative determination of IOFB projection, because. This is because, as opposed to ultrasonography, NIR TPT enables (a) determination of the projection of the ciliary body, (b) localization of the IOFB in relation to the scleral projection of the ciliary body, and, consequently, (c) selection of the best surgical treatment strategy. Therefore, in all patients of the current study, we managed to identify and localize the IOFB located in the projection of the ciliary body or in the lens with the use of non-invasive NIR TPT technique. Non only radio-opaque, but also radiolucent IOFBs were visualized by this approach. In all cases, IOFBs were localized in relation to ciliary body structures, and clear scleral landmarks were captured in the projection of the IOFB. In addition, we managed to visualize IOFBs in the presence of opaque media using NIR TPT. Conclusion NIR TPT enables non-invasive visualization of IOFBs in the anterior segment, as well as localization of these IOFBs in relation to ciliary body structures in patients with penetrating globe injury. Further research is warranted to assess the potential and value of the proposed method in diagnosing IOFBs of various origins and locations. References 1.Erikitola O, Shahid S, Waqar S, Hewick S. Ocular trauma: classification, management and prognosis. Brit J Hosp Med. 2013;74:108-11. 2.Loporchio D, Mukkamala L, Gorukanti K, Zarbin M, Langer P, Bhagat N. Intraocular foreign bodies. Surv Ophthalmol. 2016; 61(5):582-96. 3.Lima-G?mez V, Blanco-Hern?ndez D, Rojas-Dosal J. Ocular trauma score at the initial evaluation of ocular trauma.CIR CIR. 2010 May-Jun;78(3):209-13. 4.Arora R, Sanga L, Kumar M, Taneja M. Intralenticular foreign bodies: report ofeight cases and review of management. Indian J Ophthalmol. 2000;48:119-22. 5.Zhang Y, Zhang M, Jiang C, Qiu HY. Intraocular foreign bodies in Сhina: clinical characteristics, prognostic factors, and visual outcomes in 1,421 eyes. Am J Ophthalmol. 2011;152(1):66-73. 6.Raina U, Kumar V, Kumar V, Sud R, Goel N, Ghosh B. Metallic intraocular foreignbody retained for four years – an unusual presentation. Cont Lens Anterior Eye. 2010;33:202-4. 7.Gundorova RA, Stepanov AV, Kurbanova NF. [Current ocular traumatology]. Moscow: Meditsina; 2007. Russian. 8.Pandey A.N. Ocular Foreign Bodies: A Review. J Clin Exp Ophthalmol. 2017; 8: 645. 9.Gundarova R, Chentsova E, Leparskaya N, Lugovkina K, Pavlova V, Shaldin P. [Ultrasound biomicroscopy and laser Doppler fluormetry study of the ciliary body in traumatic retinal detachment due to ocular contusion]. Rus Ophthalmol J. 2012;3:14-8. Russian. 10.Kaushik S, Ichhpujani P, Ramasubramanian A, Pandav SS. Occult intraocular foreign body: ultrasound biomicroscopy holds the key. Int Ophthalmol. 2008;28:71-3. 11.Koch FHJ, Deuchler S, Singh P, Hessling M. Diaphanoskopie am Auge. Ophthalmologe. 2017;114(9):857-64. 12.Zadorozhnyy O, Alibet Yassine, Kryvoruchko A, Levytska G, Pasyechnikova N. Dimensions of ciliary body structures in various axial lengths in patients with rhegmatogenous retinal detachment. Journal of Ophthalmology (Ukraine). 2017;6:32-6. 13.Zadorozhnyy O, Korol A, Nevska A, Kustryn T, Pasyechnikova N. Ciliary body imaging with transpalpebral near-infrared transillumination – a pilot study. Klinika oczna. 2016;3:184-6. 14.Wylegala E, Dobrowolski D, Nowinska A, Tarnawska D. Anterior segment optical coherence tomography in eye injuries. Graef Arch Clin. Exp.2009;247:451-5. 15.Pasyechnikova N, Naumenko V, Korol A, Zadorozhnyy O. Digital imaging of the fundus with long-wave illumination. Klinika oczna. 2009;111(1-3):18-20. The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|