J.ophthalmol.(Ukraine).2019;4:8-12.
|
http://doi.org/10.31288/oftalmolzh20194812 Current surgical rehabilitation techniques for patients with total bilateral symblepharon S.A. Iakimenko, Dr Sc (Med), Prof., P.O. Kostenko, Cand Sc (Med) SI " The Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine”; Odesa, Ukraine E-mail: piter1812@rambler.ru TO CITE THIS ARTICLE: Iakimenko SA, Kostenko PO. Current surgical rehabilitation techniques for patients with total bilateral symblepharon. J.ophthalmol.(Ukraine).2019;4:8-12. http://doi.org/10.31288/oftalmolzh20194812
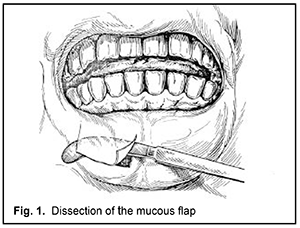
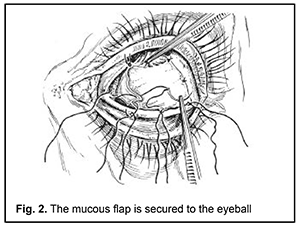
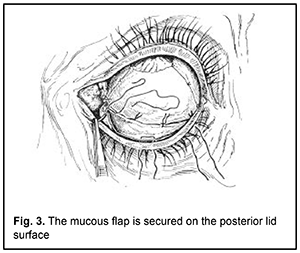
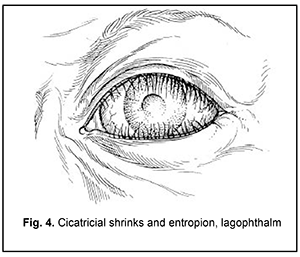
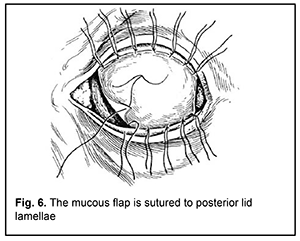
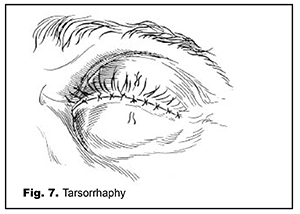
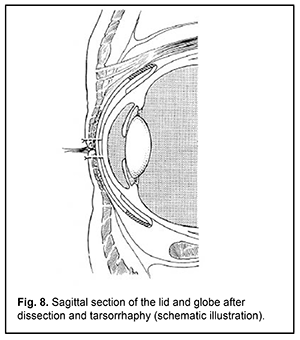
Purpose: To investigate the efficacy of a three-stage surgical rehabilitation technique for patients with bilateral total symblepharon; the technique has been developed and advanced and is being used at present at the Ocular Burn Injury Department. Materials and Methods: We investigated the outcomes of patients with bilateral total symblepharon undergoing either of the two oral mucosal autotransplantation procedures developed for symblepharon removal at the department. A total of 86 patients with bilateral total symblepharon underwent either of the two procedures during 2005 to 2018. Of these patients, 34 (39.5%) had the two-stage procedure, and 52 (60.5%), the three-stage procedure. Results: Constructed fornices were assessed with objective measurements of forniceal depth and symmetry, and presence or absence of entropion. Our three-stage technique allowed us to transplant more labial mucosal grafts during the first two stages, with a success rate of 86.5% (46 patients), compared to 76.5% (26 patients) for the two-stage technique. In addition, of the patients who had the three-stage surgical rehabilitation procedure, only 17.3% (9 patients) developed transitory intraocular hypertension, compared to 23.5% (8 patients) for those who had the two-stage procedure. Conclusion: The three-stage surgical rehabilitation technique for patients with total bilateral symblepharon was developed and piloted at the Ocular Burn Injury Department, and was found safe and effective. This allows recommending it for widespread use in ophthalmological practice. Keywords: symblepharon, ankyloblepharon, labial mucosal autogenous labial mucous membrane Introduction Functional and cosmetic rehabilitation of patients with total bilateral symblepharon secondary to severe burn, Stevens–Johnson syndrome, ocular pemphigoid, trachoma, atopic keratoconjunctivitis, or etc. is a challenge for the ophthalmic plastic surgeon and a serious social-and-psychological problem for the patient. The operative treatment is labor-intensive, has many stages, and involves various surgical interventions associated both with autogenous labial mucous membrane (ALMM) transplantation and local tissue flaps; however, treatment outcomes are not always predictable. The difficulty of solution is due to the anatomic tomography and physiologic structure of the area, variable etiology and clinical picture of the disease, development of systemic autosensitization to collagen in patients who have undergone a number of reconstructive surgeries, and patient’s preference for the best cosmetically acceptable result. Many different techniques have been suggested for symblepharon removal, but the most widely used strategies of fornix reconstruction for symblepharon at present are those involving ALMM transplantation [1-3]. There have been reports on the use of autologous cultivated conjunctival or skin cells in combination with ALMM transplantation [4, 5]. These methods share such disadvantages as (a) an additional trauma to the patient due to preparation of an additional operative field and (b) increased complexity and duration of surgery. There have been reports on grafting the area with either cadaveric labial mucosa or the conjunctiva or peritoneum from dead born fetuses in order to avoid additional trauma [6-8]. The disadvantage of these approaches is poor conjunctival fornix restoration due to the poor viability of these tissues. In addition, the use of the material from fetuses dead born raises concerns related to ethics and risk of transmitted diseases. The above approaches are very rarely employed due to these reasons. Attempts have been made to combine the use of several treatment methods. A combined approach of cicatrix lysis, intraoperative mitomycin C (MMC) application, oral mucosal transplantation (OMT) and amniotic membrane transplantation (AMT) is available, with the aim of both removing a symblepharon and reducing the risk of its recurrence [9]. Given the possibility of severe complications after the use of MMC, new AMT approaches avoiding the use of MMC are being developed. In a retrospective, interventional case series by Zhao et al [10], 16 eyes of 14 patients with symblepharon were consequently operated by conjunctival recession, sealing the gap between recessed conjunctiva and Tenon capsule with a running 9-0 nylon suture, and covering of the bare sclera with amniotic membrane. The authors concluded that this method not only avoids the use of mitomycin C, but also creates a strong barrier to prevent recurrence, restore ocular surface integrity, reform a deep fornix, and regain full ocular motility [10]. However, even the most advanced techniques for total symblepharon require the use of ALMM transplantation. A so-called two-stage approach to removal of an extensive or total symblepharon or ankyloblepharon was proposed by N.O. Puchkivska in 1951 [11], detailed and investigated by G.V. Legeza in 1956 [12, 13], and has been used for decades and worked well at the Ocular Burn Injury Department. With the lapse of time, however, some drawbacks of this approach have been identified. Thus, in eyes with secondary glaucoma, raised intraocular pressure (IOP) is common and very difficult to combat after this procedure. The purpose of the study was to investigate the efficacy of a three-stage surgical rehabilitation technique patients with bilateral total symblepharon; the approach has been developed and advanced and is being used at present at the Ocular Burn Injury Department. Materials and Methods We investigated the outcomes of patients with bilateral total symblepharon undergoing either of the two oral mucosal autotransplantation procedures developed for symblepharon removal at the department. A total of 86 patients with bilateral total symblepharon underwent either of the two procedures during 2005 to 2018. Of these patients, 34 (39.5%) had the two-stage procedure, and 52 (60.5%), the three-stage procedure. In the three-stage procedure, the adhesion between the lower eyelid and the globe is removed during the first stage, and that between the upper eyelid and the globe, during the second stage, with the two stages conducted with a gap of two to three months. Care should be taken while separating the adhesion between the globe and the eyelid to prevent palpebral cartilage from damage and to prevent the eyelid from being perforated. Intraoperatively, the mucous flap is set into place in half of the globe episclerally, in the limbal plane and in the fornix, with edge-to-edge apposition between it and the adjacent conjunctiva, if this conjunctiva is partially maintained, at the anterior lid margin, and is sutured with U-shaped buried sutures to eyelids (Fig. 1, 2, 3). In the two-stage procedure, the globe is covered completely, and the lids are covered partially with the labial mucous membrane grafts during the first stage. Since in the three-stage procedure, the mucous membrane covers only half of the globe during the first and second stages, an increase in IOP will be insubstantial, and easier to manage. The third stage is performed 2 to 3 months after the second stage; it is aimed at elimination of lagophthalm and entropion, since the mucous graft shrinks during fixation to the posterior lid surface (Fig. 4). This surgical procedure consists in lengthening the posterior eyelid lamella using a labial mucosal flap, and performing a permanent tarsorrhaphy (Fig. 5-8). The tarsorrhaphy is opened in 6 to 8 months, after the cicatricial process is completed. The two points related to conduct of this stage are noteworthy since their non-observance may result in failure of the procedure. First, when performing dissection of the upper eyelid, attention must be paid not to violate the integrity of the upper eyelid levator muscles. Second, before sewing the eyelids together, it is important to trim their margins properly. That is, only the epithelium between the anterior and posterior margins of the lid is removed, paying attention not to damage lid margins and/or eyelashes.
A few points related to postoperative patient management are also noteworthy. First, a tight dressing is applied for 2 to 3 days. Second, thorough cavity and suture hygiene is a must. After the tight dressing is removed, dressing changes are usually performed 3-4 times a day, accompanied by cavity irrigation with antibiotic (or antiseptic) solution through openings between the eyelids at the external or internal canthus. To prevent infectious complications after reconstructive and plastic surgery, we widely use active systemic anti-inflammatory therapy with selective and nonselective NSAIDs and antibacterial therapy with broad-spectrum antibiotics. Results Constructed fornices were assessed with objective measurements of forniceal depth and symmetry, and presence or absence of entropion. The surgical outcome was considered a success if the conjunctival fornices were completely restored. Our three-stage technique allowed us to transplant more labial mucosal grafts during the first two stages, with a success rate of 86.5% (46 patients), compared to 76.5% (26 patients) for the two-stage technique. Thus, entropion developed after opening the tarsorrhaphy in eyes of some patients, which required a modified Millingen-Sapezhko procedure (for a mild entropion) or lengthening the posterior eyelid lamella. We employ a Millingen-Sapezhko procedure modified by Tagibekov [2, 14]. Because eyes of some patients exhibit rough eyelid margins and/or a small or no space between the anterior and posterior margins of the lid, the labial mucosal graft for transplantation to the intermarginal space is cut out not as a flat stripe without submucosal tissue, but as a wedge-shaped stripe with partial involvement of this tissue. Dissection in the intermarginal space is made along the entire length of the lid, and the labial mucosal stripe graft is placed in between the dissected structures and fixed with interrupted sutures. Of the patients who had the three-stage surgical rehabilitation procedure, only 17.3% (9 patients) developed transitory intraocular hypertension, compared to 23.5% (8 patients) for those who had the two-stage procedure. Since aqueous humor hypersecretion and aqueous outflow abnormalities are major causes of postoperative intraocular hypertension, active anti-inflammatory agents and aqueous secretion inhibitors should be used as therapeutic measures. We have found that acetazolamide has a strong hypotensive effect in patients with transitory intraocular hypertension. Conventional therapeutic doses of oral acetazolamide (0.125-0.250 g, two to three times daily for 2-5 days, with a two-day drug-free interval after each five-day acetazolamide treatment period) are usually enough, with patient’s urine checked every 5-7 days. A requirement for time intervals between treatment periods, contraindication in patients with renal disease, and acidosis are the disadvantages of acetazolamide. In addition, patients are treated with topical 2% dorzolamide hydrochloride, the latter being a carbonic anhydrase inhibitor. Inhibiting the carbonic anhydrase of the ciliary body results in reduced aqueous humor (AH) secretion, mostly due to reduced production of bicarbonate ions followed by reduced sodium ion and AH transport. Topical dorzolamide hydrochloride reduces elevated AH, which is a risk factor for optic nerve damage. In our single-drug treated patients, two drops of dorzolamide hydrochloride were administered two to three times daily, and local side effects (eye tingling and/or burning sensation) were very uncommon and short-term, and did not pose a contraindication to continuation of treatment. No systemic side effects were observed. Conclusion
The three-stage surgical rehabilitation technique for patients with total bilateral symblepharon was developed and piloted at the Ocular Burn Injury Department, and was found safe and effective. This allows recommending it for widespread use in ophthalmological practice.
References 1.Puchkovskaia NA, Iakimenko SA, Nepomiashchaia VM. [Eye burns]. Moscow: Meditsina;2001. Russian. 2.Iakimenko SA. [Keratoprosthesis]. Odesa: SIMEKS-PRINT;2018. Russian. 3.Mai C, Bertelmann E. Oral mucosal grafts: old technique in new light. Ophthalmic Res. 2013;50(2):91–8. 4.Li T, Shao Y, Lin Q, Zhang D. Reversed skin graft combining with lip mucosa transplantation in treating recurrent severe symblepharon: A case report. Medicine (Baltimore). 2018 Aug; 97(35):e12168. 5.Scuderi GL, Mancino R, Nucci C, Alfano C, Scuderi N. Clinical transplantation of cultured conjunctiva in oculoplastic surgery. In: Proceedings of the 28th International Congress of Ophthalmology. Amsterdam, the Netherlands. June, 1998. p.171. 6.Alekseev SA. [Our experience of labial mucous membrane transplantation from cadavers in a Millingen-Sapezhko procedure]. Vestn Oftalmol. 1963;(6):76-9. Russian. 7.Gundorova RA, Bordiugova GG, Travkin AG. [Surgical reconstruction of the eye globe]. Moscow: Meditsina;1983. Russian. 8.Zaikova MV. [Ophthalmic plastic surgery]. Moscow: Meditsina;1980. Russian. 9.Kheirkhah A, Ghaffari R, Kaghazkanani R, et al. A combined approach of amniotic membrane and oral mucosa transplantation for fornix reconstruction in severe symblepharon. Cornea. 2013 Feb;32(2):155–60. 10.Zhao D, Yin HY, Cheng A, et al. Sealing of the gap between the conjunctiva and tenon capsule to improve symblepharon surgery. Am J Ophthalmol. 2015 Sep;160(3):438–446.e1. 11.Puchkovskaia NA. [Operative treatment of extensive and complete symblepharons]. Vestn Oftalmol. 1951 Jul-Aug;30(4):6-13. Russian. 12.Legeza GV. [Surgical treatment of extensive or total symblepharon in the presence of the globe]. Cand Sc (Med) Thesis Abstract. Odessa: Filatov Institute of Eye Disease and Tissue Therapy; 1956. Russian. 13.Legeza GV. [On the use of labial mucous membrane grafts]. In: [Ocular trauma in industry and agriculture]. Kyiv;1967. p. 77-9. Russian. 14.Tagibekov KK. [Operative treatment of conjunctival cavity failure in anophthalmos and some issues related to cosmetic prosthesis]. Cand Sc (Med) Thesis Abstract. Odessa: Filatov Institute of Eye Disease and Tissue Therapy; 1971. Russian.
The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|