J.ophthalmol.(Ukraine).2019;3:45-51.
|
Received: 14 March 2019; Published on-line: 27 June 2019 http://doi.org/10.31288/oftalmolzh201934551 A thermoelectric device for ophthalmic heat flux density measurements: results of piloting in healthy individuals L.I. Anatychuk,1,2 Institute Director, Member of the NAS of Ukraine, Dr Sc (Phys and Math), Prof.; N.V. Pasyechnikova,3 Assoc. Member of the NAMS of Ukraine, Dr Sc (Med), Prof.; V.A. Naumenko,3 Dr Sc (Med), Prof.; O.S. Zadorozhnyy,3 Cand Sc (Med); R.R. Kobylianskyi,1,2 Senior Research Fellow, Cand Sc (Phys and Math); N.V. Gavrilyuk,1,2 Research Fellow 1 Institute of Thermoelectricity of the National Academy of Science and Ministry of Education and Science; Chernivtsi (Ukraine) 2 Yuriy Fedkovych Chernivtsi National University; Chernivtsi (Ukraine) 3 Filatov Institute of Eye Diseases and Tissue Therapy, NAMS of Ukraine; Odesa (Ukraine) E-mail: zadoroleg2@gmail.com TO CITE THIS ARTICLE: Anatychuk LI, Pasyechnikova NV, Naumenko VA, Zadorozhnyy OS, Kobylianskyi RR, Gavrilyuk NV. A thermoelectric device for ophthalmic heat flux density measurements: results of piloting in healthy individuals. J.ophthalmol.(Ukraine).2019;3:45-51. http://doi.org/10.31288/oftalmolzh201934551 Background: Assessment of heat exchange processes in the human body is based on temperature and heat flux measurements. Today, there is no instrument for measuring the heat flux density from the eye. Purpose: To investigate the heat flux density from the ocular surface in healthy individuals using the developed thermoelectric device. Materials and Methods: The thermoelectric device for the measurement of heat flux from the eye has been developed within the framework of the partnership agreement between the Institute of Thermoelectricity and the Filatov Institute. Thirty-two healthy individuals (64 eyes) were under observation. Participants were divided into three age groups. They underwent a bilateral eye examination which included measurements of intraocular pressure, temperature of the external corneal surface, and heat flux density from the eye. Results: Mean room temperature during examination sessions was 21.3 ± 0.8 °С. In addition, mean temperature of the external ocular surface and mean heat flux density from the human eye were 34.6 ± 0.7°С and 7.7 ± 1.3 mW/cm2, respectively. We found that the heat flux density from the eye decreased with age in healthy subjects. Conclusion: The first ever thermoelectric device for real-time measuring of the heat flux density from the human eye was developed. The developed device was used to measure the heat flux density from the eye in healthy subjects, and to demonstrate the relationships of this characteristic with the temperature of the external ocular surface and subject age. Keywords: temperature of the external ocular surface, heat flux density, thermoelectric device
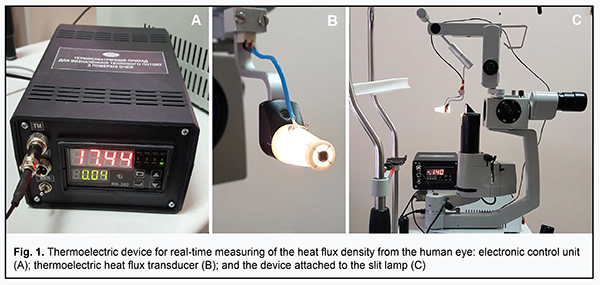
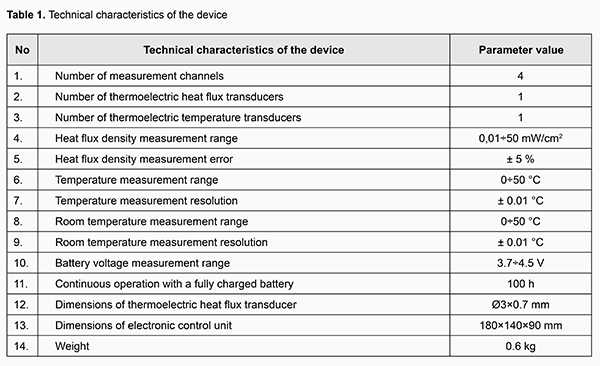
Introduction A wealth of data has been amassed on thermometry and thermography findings on the temperature and temperature distribution in the surface area of the human body and some of its internal organs. The field of knowledge on the temperature of the human body and its organs is well equipped with measurement instrumentation. The methods available for non-contact or contact registration of temperatures in various ocular compartments have their advantages and disadvantages. Non-contact temperature measurement techniques like infrared thermometry or thermorgraphy provide for safe assessment of temperatures and their distribution in the ocular surface, and are used in diagnosing various eye disorders [1-4]. Contact thermometry techniques are used to study temperatures not only of the cornea and sclera, but also of the internal structures of the eye. However, since introduction of the measurement probe into the human eye cannot be considered safe as a routine intraocular temperature measurement procedure, it is justified only if it is performed during surgery through the incision already made for insertion of surgical instrumentation. This is reasonable, e.g., for monitoring temperatures in the eye during vitreoretinal surgery which is usually performed under conditions of artificially induced uncontrolled local hypothermia [5]. Heat process characteristics include not only temperatures and temperature distribution, but also heat flux, which is a major heat exchange index and reflects the function of organs and organs more completely than the two former characteristics [6]. Recently, progress has been made in the development of advanced instrumentation for the local measurement of the heat flux from human body surface. Thermoelectric heat flux transducers have been developed, which have high sensitivity and accuracy and rapid response times, provide robust performance in a wide temperature range, and incorporate interfaces for communication with up-to-date registration equipment [7-9]. The use of these transducers provides for high-accuracy measurement of heat-flux density [10]. However, to the best of our knowledge, there have been no reports on the measurement of heat flux from the eye. Early diagnosis of eye conditions characterized by changes in intraocular circulation and metabolism (inflammation, uveal tumors, glaucoma, etc.) is still a challenge for ophthalmologists. Obviously, impaired ocular circulation and metabolism must be accompanied by changes in heat exchange indices [4, 11]. Thus, relationships of ocular surface temperature with circulation, intraocular pressure, and presence of inflammation or intraocular tumors have been demonstrated [1, 12, 13]. A change in heat characteristics of the eye may occur in early disease, before clinical symptoms are apparent, and recording these characteristics might be a promising approach in early diagnosis of various eye disorders. The purpose of this study was to investigate the heat flux density from the ocular surface using the developed thermoelectric device. Materials and Methods The thermoelectric device for determining the heat flow from the eye has been developed within the framework of the partnership agreement between the Institute of Thermoelectricity of the NAS of Ukraine and MES of Ukraine and the Filatov Institute, and was used for piloting. To the best of our knowledge, there have been no reports on any device for measurement of the heat flow from the eye. Photographs and characteristics of the device are presented in Fig.1 and Table 1, respectively.
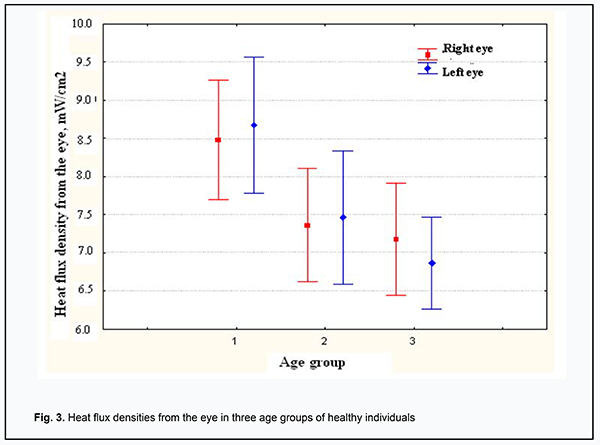
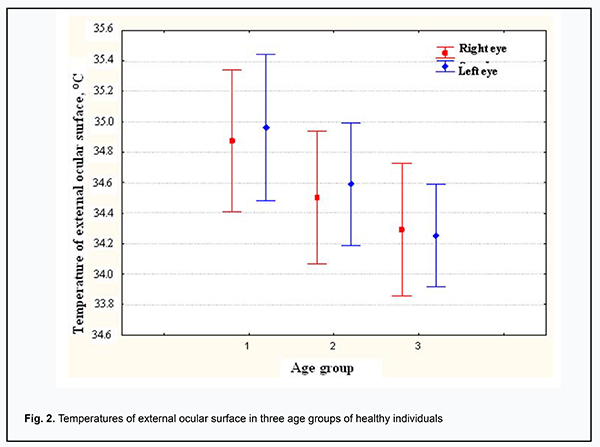
The multichannel device for determining the heat flow from the eye consists of the electronic control unit and the thermoelectric heat-flux transducer. The miniature thermoelectric heat-flux transducer was developed and manufactured for the above device according to the patented proprietary technology of the Institute of Thermoelectricity [14-16]. A thermoelectric micromodule of dimensions 2 × 2 × 0.5 mm incorporates 100 p-type and n-type crystals (0.17 × 0.17 × 0.4 mm) of Bismuth Telluride-based thermoelectric material. The module is placed between two Al2O3–based ceramic plates of 3 mm diameter and 0.1 mm thickness, and has its side faces sealed with a special sealant. Therefore, the manufactured thermoelectric heat-flux transducer is 0.7 mm high and 3 mm in diameter. It is fixed on a custom-made contact prism, the prism-transducer assembly is easily attached to the conventional prism mount of the Goldmann tonometer, and the latter can be connected to slit lamps of various manufacturers. In addition, the assembly can be easily removed for disinfection between patients. The thermoelectric heat-flux transducer is fastened at the center of the contact prism, and comes into direct contact with the individual’s ocular surface (in our study, with the central cornea or scleral conjunctival surface). Aloe of note is that the contact surface of the thermoelectric heat-flux transducer is non-traumatic to the eye (trimmed) and can be easily disinfected. The electronic unit incorporates a heat flux channel for (a) accurate measurement of the voltage generated by the thermoelectric heat-flux transducer and (b) subsequent transformation of the voltage to the physical quantity expressed in heat flux density units (mW/cm2). In addition, it incorporates (a) a temperature measurement channel for accurate measurement of the surface temperature of the investigated target (here, the ocular surface structures) with thermocouple transducer and (b) an ambient temperature measurement channel. The device is provided with a battery power supply. The clinical portion of this study was an open pilot study, followed the ethical standards stated in the Declaration of Helsinki and was approved by the Local Ethics Committee of the Filatov Institute. Written informed consent was obtained from all individual participants included in the study. Thirty-two healthy individuals (64 eyes) who had given written informed consent were under observation. Participant age ranged from 16 to 86 years, and participants were divided into three age groups (16-30, n=11; 31-60, n=10; >60, n=22). They underwent a bilateral eye examination which included measurements of IOP, temperature of the external corneal surface, and heat flux density from the eye. Ocular examination was performed under stable environmental conditions (air temperature and humidity control and minimal indoor air velocity). Before evaluation, participants spent 15 minutes indoors for adaptation to the room environment. They were administered epibulbar anesthesia with ophthalmic 0.5% proparacaine hydrochloride (ALCAINE®, SA Alcon-Couvreur NV, Puurs, Belgium). Temperatures and heat flux density were recorded 15 minutes after instilling a drop of the anesthetic. During evaluation, patients were positioned before a slit-lamp apparatus. The thermoelectric heat-flux transducer came into direct contact with the subject’s central cornea in all cases. Real-time measurements were repeated at least three times for each eye. Fifteen subjects (30 eyes) underwent heat flux density measurements for not only the subject’s central cornea, but also for projections of the pars plana ciliaris in the nasal and temporal quadrants. In these 15 subjects, heat flux density measurements for the central cornea were repeated three times by another examiner 15 minutes after completion of initial three measurements. Statistical analyses Statistical analyses were conducted using Statistica 10.0 (StatSoft, Tulsa, OK, USA) software. Data are presented as mean and standard deviation (SD). Pearson correlation was used to assess the independent correlation between the temperature of the external ocular surface and heat flux density from the eye. A two-tailed Student test was used for group comparisons and the level of significance p ≤ 0.05 was assumed. Results Mean room temperature and relative humidity during examination sessions were 21.3 ± 0.8°С and 48.5 ± 1.6%, respectively. In addition, mean IOP, temperature of the external ocular surface, and heat flux density from the human eye were 16.5±2.7 Hg, 34.6 ± 0.7°С (range, 33 to 36°С), and 7.7±1.3 mW/cm2 (range, 4.9 to 11.7 mW/cm2), respectively. Temperature of the external ocular surface was positively correlated with heat flux density from the eye (r = 0.34; p = 0.006). There was no significant difference in temperature of the external ocular surface or heat flux density from the eye between the right and left eyes (p = 0.78 and p = 0.9, respectively). In the fifteen subjects (30 eyes) that underwent additional measurements, the mean heat flux density for the central cornea was 7.84±1.54 mW/cm2, whereas those for projections of the pars plana ciliaris in the nasal and temporal quadrants were 7.2±1.18 mW/cm2 (p=0.19) and 6.95±0.97 mW/cm2 (p=0.07), respectively. Moreover, in these 15 subjects, heat flux density measurements for the central cornea were repeated three times by another examiner 15 minutes after completion of initial three measurements, and mean heat flux density for the central cornea measured by the first and second examiners was 7.84±1.54 mW/cm2 and 8.1±1.68 mW/cm2, respectively (p = 0.64). We also assessed the relationships of temperature of the external ocular surface and heat flux density from the eye with patient age (Fig. 2, 3). The temperature of the external ocular surface in group 1 (34.9 ± 0.7°С) was somewhat higher than in group 2 (34.6 ± 0.7°С; p = 0.07) and in group 3 (34.6 ± 0.7°С; p = 0.002), although the difference in this index between group 3 and group 2 was not statistically significant (p = 0.13). In addition, the heat flux density from the eye in group 1 (8.6 ± 1.2 mW/cm2) was somewhat higher than in group 2 (7.4 ± 1.1 mW/cm2; p = 0.003) and in group 3 (7.0 ± 1.0 mW/cm2; p < 0.001), although the difference in this index between group 3 and group 2 was not statistically significant (p = 0.2).
No corneal trauma or other complications were observed in any participant during the examination. Discussion This paper presents the first findings of measurements of heat flux density from the eye in healthy humans using the developed thermoelectric device. Preliminary results of clinical piloting the device demonstrated that it is safe in operation which is ensured by the design of the thermocouple transducer and by the use of battery power supply. Attachment of the prism-transducer assembly to the conventional prism mount of the Goldmann tonometer contributed to easy and prompt measurements, since the pressure exerted by the transducer on the cornea did not vary from eye to eye, thereby improving also stability of measurements. Our findings demonstrated that interocular symmetry in heat flux density is high in healthy subjects. It is noteworthy also that the temperature of the external corneal surface is of the same order in the right and left eyes, which is in agreement with previous studies [1, 11, 17]. Heat flux measurements can be made not only for the central cornea, but also for some other portions of the ocular surface. In the current study, the heat flux density for the central cornea was higher than those for projections of the pars plana ciliaris in the nasal and temporal quadrants. This was possibly because the ciliary body has an intensive blood supply, whereas the cornea has no own blood supply, and thus easily looses heat when the eye is opened. In addition, heat flux density measurements for the central cornea and for projections of the pars plana ciliaris in the nasal and temporal quadrants were smooth. We, however, failed to ensure adequate contact between the entire contact surface of the transducer and ocular surface for projections of the pars plana ciliaris in the superior and inferior quadrants in some cases. Therefore, although attachment of the prism-transducer assembly to the conventional prism mount of the Goldmann tonometer has undisputable advantages, it also has limitations, and additional design solutions are required to remove these limitations. Also of note are some differences in ocular heat flux characteristics between age groups. Thus, we found that the temperature of the external corneal surface and the heat flux density from the eye decreased with increase in age of healthy subjects. This can be explained based on well known facts. The blood flow in the choroid acts as the major source of heat for the human or animal eye. Blood entering the eye has a temperature that is practically equal to that of the body, and produces a temperature gradient between the choroid and cornea which induces a heat transfer from blood to ocular tissues. The heat distributed across ocular tissues is lost to the environment by convective, conductive, radiative, and evaporative mechanisms [4, 17]. The choroid gets thinner with age. Spaide introduced the notion of age-related choroidal atrophy [18]. Spectral-domain ocular coherence tomography (SD-OCT) thickness of the choroid and rheoophthalmographic indices (rheographic coefficients) has been found to correlate with age in patients with age-related macular degeneration [19]. Therefore, age-related atrophic choroidal changes and associated decreased blood volume in the uveal tract might be a cause of a decrease in heat flux density from the eye with age in healthy individuals. Thus, preliminary results of clinical piloting the developed thermoelectric device for ophthalmic heat flux density measurements demonstrated that it is easy and safe in operation. Also of note is also that the device is self-sufficient, universal (i.e. our prism-transducer assembly is designed to connect to any Goldmann tonometer through the conventional prism mount, and thus is compatible with any slit lamp) and can be used for real-time measurements. Further studies targeted at investigating the heat flux density from the eye in various eye disorders are warranted to assess the potential of ophthalmic heat flux density measurement technique for application in diagnostic purposes. The authors thank Prof. A.S. Buiko for his methodological help. Conclusion First, we tested the first ever thermoelectric device for real-time measuring of the heat flux density from the human eye. Second, heat flux density from the human eye was 7.7±1.3 mW/cm2 with room temperature of 21.3±0.8 °С. Third, temperature of the external ocular surface was moderately positively correlated with heat flux density from the eye (r = 0.34; p = 0.006). Finally, the study provided preliminary data of the relationship between heat flux density from the human eye and age in healthy individuals: the heat flux density from the eye in groups of individuals aged 16-30, 31-60 and above 60 years was 8.6 ± 1.2 mW/cm2, 7.4 ± 1.1 mW/cm2, and 7.0 ± 1.0 mW/cm2, respectively. References 1.Maletskiĭ AP, Puchkovskaia NA, Kremenchugskiĭ LS, Buĭko AS, Terent'eva LS. [Diagnostic value of distance thermometry of the anterior surface of the eye in epibulbar and intraocular neoplasms]. Oftalmol Zh. 1985;(1):12-5. Russian. 2.Buĭko AS, Tsykalo AL, Terent'eva LS, Niankina EE. [Thermography based on liquid crystals in ophthalmologic oncology]. Oftalmol Zh. 1977;32(2):110-4. Russian. 3.Zadorozhnyy OS, Savin NV, Buiko A.S. Improving the technique for controlled cryogenic destruction of conjunctival tumors located in the projection of the ciliary body onto the sclera: A preliminary report. J Ophthalmol. (Ukraine). 2018; 5:60-65. 4.Tan JH, Ng EYK, Acharya U R, Chee C. Infrared thermography on ocular surface temperature: A review. Infrared Phys Techn. 2009; 52:97-108. 5.Nazaretian RE, Zadorozhnyy OS, Umanets NN, et al. Intraocular temperature changes during vitrectomy procedure. J Ophthalmol (Ukraine). 2018; 6:30-34. 6.Grischenko TG, Dekusha LV, Vorobiov L.Y. [Heat flow measuring: theory, metrology, practice]. Book 1. [Methods and means of heat flow measuring]. Kyiv: Institute of Engineering Thermophysics of NASU; 2017. Russian. 7.Anatychuk LI, Ivaschuk OI, Kobylianskyi RR, et al. [Thermoelectric device ALTEC-10008 for temperature and heat flux density measurement]. Journal of Thermoelectricity. 2016; 1:76-84. Russian. 8.Anatychuk LI, Yuryk OYe, Kobylianskyi RR, et al. [Thermoelectric device for the diagnosis of inflammatory processes and neurological manifestations of vertebral osteochondrosis]. Journal of Thermoelectricity. 2017; 3:54-67. Ukrainian. 9.Anatychuk LI, Kobylianskyi RR, Cherkez RG, et al. Thermoelectric device with electronic control unit for diagnostics of inflammatory processes in the human organism. Tekhnologiya i konstruirovanie v elektronnoi apparature. 2017; 6:44-48. 10.Anatychuk LI, Ivaschuk OI, Kobylianskyi RR, et al. [On the effect of environmental temperature on the readings of thermoelectic sensors for medical applications]. Sensorna elektronika I microsystemni tekhnologii. 2018; 15(1):17-29. Ukranian. 11.Zadorozhnyy OS, Guzun OV, Bratishko AIu, Kustrin TB, Nasinnik IO, Korol AR. Infrared thermography of external ocular surface in patients with absolute glaucoma in transscleral cyclophotocoagulation: a pilot study. J Ophthalmol. (Ukraine). 2018; 2:23-28. 12.Galassi F, Giambene B, Corvi A, Falaschi G. Evaluation of ocular surface temperature and retrobulbar haemodynamics by infrared thermography and colour Doppler imaging in patients with glaucoma. Br J Ophthalmol. 2007; 91:878-81. 13.Sodi A, Giambene B, Falaschi G, et al. Ocular surface temperature in central retinal vein occlusion: preliminary data. Eur J Ophthalmol. 2007 Sep-Oct;17(5):755-9. 14.Anatychuk LI, Konstantynovych IA. [Method for manufacturing thermoelectric microbatteries]. Patent Ukraine No. 93217. September 25, 2014. 15.Anatychuk LI, Kobylianskyi R.R. [Method for manufacturing thermoelectric microbatteries]. Patent Ukraine No. 117719. July 10, 2017. 16.Anatychuk LI, Kobylianskyi RR, Konstantynovych IA, at al. [Technology for manufacturing thermoelectric microthermopiles]. Journal of Thermoelectricity. 2016; 6:49-54. 17.Mapstone R. Determinants of corneal temperature. Brit J Ophthalmol. 1968; 52:729-41. 18.Spaide RF. Age-related choroidal atrophy. Am J Ophthalmol. 2009; 147:801-10. 19.Korol AR, Zadorozhnyy OS, Hramenko NI, Kustrin TB. [Interrelationship of choroidal morphometric characteristics and ocular blood volume in patients with age-related macular degeneration]. J Ophthalmol (Ukraine). 2013; 3:23-27. The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|