J.ophthalmol.(Ukraine).2019;3:32-35.
|
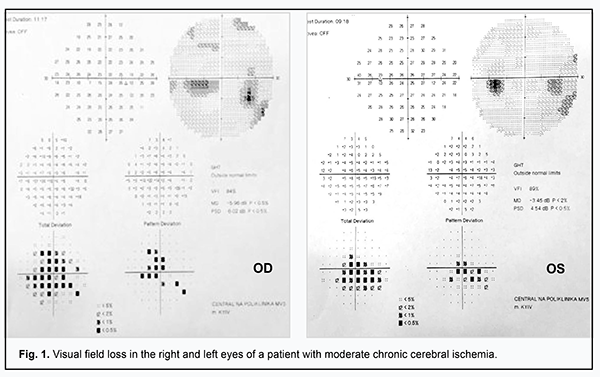
Received: 08 April 2019; Published on-line: 27 June 2019 http://doi.org/10.31288/oftalmolzh201933235 Neurological and ocular manifestations of chronic cerebral ischemia I.P. Ryzhova, Cand Sc (Med); O.V. Skorobogatova, Cand Sc (Med) Bogomolets National Medical University; Kyiv (Ukraine) TO CITE THIS ARTICLE: Ryzhova IP, Skorobogatova OV. Neurological and ocular manifestations of chronic cerebral ischemia. J.ophthalmol.(Ukraine).2019;3:32-5. http://doi.org/10.31288/oftalmolzh201933235 Purpose: To analyze neurological, neuropsychological, and ocular manifestations and their correlations in patients with chronic cerebral ischemia (CCI). Materials and Methods: One hundred and twenty patients (67 women and 53 men) with signs of mild or moderate CCI were involved in the study. They underwent clinical-and-neurologic, neuropsychologic and ocular examination, and assessment with a number of paraclinical diagnostic techniques (magnetic resonance imaging (MRI) of the brain, transcranial Doppler ultrasonography (TDS) of the major head and neck vessels, and electroencephalography. Results and Discussion: Neurological examination revealed signs of vestibulo-cerebellar, pyramidal and extrapyramidal syndromes, thereby evidencing moderate CCI. Neuropsychological tests found mild cognitive impairment syndrome in 21.5% of patients younger than 60 years. Patients with mild CCI demonstrated no significant visual impairments, but changes in electrophysiological parameters. Patients with moderate CCI demonstrated signs of chronic optic neuropathy, which was found in 71 (61.7%) cases. Non-specific results of paraclinical investigations of patients with CCI should be interpreted comprehensively. They revealed diffuse neurological symptoms of microangiopathic origin. Ocular symptoms and changes on MRI brain scans and TDS of the major head and neck vessels indicated abnormalities in the vertebrobasilar region. Conclusion: The signs of chronically impaired blood flow to the brain revealed both by clinical-and-neurologic and neuropsychologic examination, and evaluation with paraclinical diagnostic techniques may account for ocular syndromes and their severity. Visual abnormalities and changes in the electrophysiological characteristics of the visual system, in their turn, are potential predictors of chronic cerebral ischemia. Keywords: chronic cerebral ischemia, neurological symptoms, discirculatory encephalopathy, visual abnormalities, vertebrobasilar region Introduction Chronic cerebral ischemia (CCI) is one of the most prevalent cerebral vascular disorders. Unfortunately, overdiagnosis of this condition is quite common in the absence of clear and commonly adopted diagnostic criteria. Foreign studies [1, 2] have reported that vascular changes (most commonly related to microvessels) were found in one third of autopsied elderly cases, and this rate may correspond to the actual CCI prevalence rate for this age group. CCI is a form of chronic cerebrovascular insufficiency with a progradient course which is observed in young, middle-age and elderly individuals [3, 4], with the most common general causes being arterial hypertension and cerebral atherosclerosis [5, 6]. The pathogenetical basis of this cerebrovascular disorder, most commonly, is cerebral microangiopathy resulting in hypoperfusion and dysfunction of various brain regions. Subcortical and periventricular white matter are most affected due to the most unfavorable blood supply conditions [5, 7]. Although cognitive impairment is a major clinical manifestation of CCI, with the severity of impairment associated with the amount of affected brain tissue and frequently causing a severe patient condition, some patients may have additional clinical manifestations as visual abnormalities [8-12]. Since it is visual abnormalities that (a) are potential predictors of chronic cerebral ischemia, (b) worsen the general state in patients with diagnosed disease and (c) significantly affects quality of life as early as early CCI, this study aimed to investigate these syndromes [7, 13, 14]. The purpose of the study was to investigate neurological and visual manifestations in the presence of CCI. Materials and Methods One hundred and twenty patients (age, 59 ± 3.7 years; 67 (55.8%) women and 53 (44.2%) men) with signs of mild or moderate CCI were involved into the study. Those with mild CCI (45 individuals; 37.5%) were involved into the study after undergoing an annual physical examination. Patients underwent detailed clinical and neurologic, neuropsychologic and ocular examination. Brain MRI, transcranial Doppler ultrasonography (TDS) of the major head and neck vessels and electroencephalography (EEG) were used to quantify clinical impairments. An ocular examination included visual acuity (VA), total visual fields (TVF), ophthalmoscopy and electrophysiological tests (critical flicker-fusion frequency (CFF), electric sensitivity threshold (EST), and lability of the visual system (LVS)). Statistical analyses were conducted using Statistica 13.0 (StatSoft, Tulsa, OK, USA) software. Results Besides fatigue (98%), irritability (89%), impaired memory and attention (97%), frequently reported complaints included visual fatigue even in mild visual loads (asthenopia; 99%), periodic double vision (65%), reduced capacity for focusing vision (47%), periodic blurred vision (82%), seeing small black spots while looking ahead or turning one’s head (28%), periodic numbness and weakness in extremities (36%), instability when walking (52%), transient vertigo, especially when changing position of the body (63%), and somewhat constrained and retarded movements (27%). In addition, more than half of patients complained of impaired mood and feeling of tension. Clinical and neurologic examination revealed diffused microorganic CCI symptomatology in 93.5% of patients. In addition, there were signs of vestibulo-cerebellar, pyramidal and extrapyramidal syndromes, thereby substantiating the diagnosis of moderate CCI. Our neuropsychological study revealed that, with an increase in severity of CCI, the rates of mixed anxiety–depressive disorder and apparent deadaptation syndrome increased to 83% and 47%, respectively. Neuropsychological defects in patients with late CCI included neurodynamic impairments (86%), optical-spatial impairments (57%), praxis impairments (43%), auditory arrhythmia (38%), memory (mostly, auditory-verbal memory) impairments (89%), and abstraction impairments (55%). Short-term and long-term memory impairments were observed in 89% and 33%, of patients, respectively. During memory assessment, signs of developing asthenia were frequently observed (47%), and were mostly related to fatigue and flaccidity. The hypersthenic type of the asthenic syndrome was found in 19% of patients. Irritable weakness was noted in one-third of patients. The ocular examination found that, in 37 patients (30.8%), visual acuity was 0.2 ±0.04 lower than the norm of 1.0, and, in 44 patients (36.7%), there was either relative or absolute scotoma in the paracentral or peripheral visual field (Fig. 1).
Changes in electrophysiological characteristics were noted in almost all patients. Electric sensitivity threshold (EST) increased by 128 ± 11.3 μA, lability of the visual system (LVS) decreased by 28 ± 6.3 Hz, and critical flicker-fusion frequency (CFF) decreased by 19.2 ± 1.9 Hz. In addition, optic disc pallor was observed, and average vascular index was 0.7-0.8. The severity of visual impairment depended on the severity of brain damage in CCI. Thus, in mild CCI, no significant visual abnormalities were found, and there were just changes in electrophysiological characteristics. In moderate CCI, signs of chronic optic neuropathy were found in 74 patients (61.7%). Brain MRI found focal and diffuse brain changes in 13% and 79% of patients, respectively. CCI progression was accompanied by (a) an increase in the area (p < 0.05) of diffuse and small-foci-related changes in the white matter, with predominant locations in the frontal-parietal (or, less frequently, in the occipital) lobes, and (b) extension of the subarachnoid spaces and ventricular system (presumably, of the lateral ventricles and the third ventricle of the cerebrum). TDS of the major head and neck vessels found decreased blood flow velocity in the middle cerebral artery (68.3±3.1 cm/s) and/or vertebral artery (79.7±3.9 cm/s) without hemodynamic signs of stenosis in these arteries. Impaired blood flow velocity in the vertebrobasilar region was observed in 69.3% of patients, whereas in rest of patients (36.1%), the blood flow velocity in the carotid region was the most prominently impaired. The EEG findings included impaired topological distribution of brain potentials and decreased total amplitude and alpha rhythm power. Either permanent o transient increases in theta and/or delta EEG activity were noted in aggravation of clinical manifestations of the disease (p < 0.05). The EEG showed disorganized basic activity in 82% of patients. Theta or, less frequently, delta dysrhythmia was found in 23% of patients. Signs of non-specific middle structures were observed in 47% of patients and prevailed in moderate CCI. In moderate CCI, the long-term memory was more significantly decreased, whereas attention impairment and fatigue were increased, which in some cases was accompanied by changes in personality characteristics (increased irritability, shyness and depressiveness, and decreased balance, sociability and social activity). Mild cognitive impairment syndrome was found in 21.5% of patients younger than 60 years. Conclusion First, clinical and neurologic manifestations of mild or moderate CCI included diffuse microorganic CCI symptomatology in the vast majority of cases. However, patients with moderate CCI manifested neurological symptoms and syndromes evidencing chronic brain tissue ischemia predominantly in the vestibulo-cerebellar region (р < 0.05). Second, as the clinical and para-clinical signs of chronically impaired blood flow to the brain become more apparent, the symptoms of potential neuropsychological manifestations of CCI become the core clinical manifestations of the disease. These signs may become apparent enough to manifest moderate cognitive impairments in patients with moderate CCI (21.5% of patients). Third, although the severity of ocular impairments parallels the severity of other neurological manifestations, in some cases, these impairments may precede other neurological manifestations and have a prognostic value. Therefore, from a practical point of view, an ocular evaluation including electrophysiological characteristics of the visual system should be recommended for patients of the relevant age group. Finally, non-specific results of paraclinical investigations of patients with CCI were interpreted as comprehensively as they should be, and provided support for the microangiopathic origin of the detected impairments. With the development of visual symptoms and brain MRI syndromes in patients with CCI, TDS of the major head and neck vessels most commonly reveals impairments in the vertebrobasilar region. References 1.Besson M, Forget B. Cognitive dysfunction, affective states, and vulnerability to nicotine addiction: A multifactorial perspective. Front Psychiatry. 2016 Sep 21;7:160. 2.Madjidova YN, Usmanova DD. Cognitive status in patients with chronic cerebral ischemia. International Journal of BioMedicine. – 2013; 3 (4): 244-6. 3.Mishchenko TS. [Discirculatory encephalopathy: and obsolete term or clinical reality]. Mezhdunarodnyi nevrologicheskii zhurnal. 2013; 2(56): 68–71. Russian. 4.Mishchenko TS, Mishchenko VN, Lapshina IA. [Optimization of treatment of patients with discirculatory encephalopathy]. Ukrainskyi visnyk psykhonevrologii. 2015; 22(1): 37–41. Russian. 5.Dziak LA, Miziakina EV, Suk VM. [New capabilities for the correction of cognitive deficiency in discirculatory encephalopathy resulting from atherosclerotic brain damage]. Zhurnal Nevrologii im. B. M. Man'kovskogo. 2017; 5(1): 34–41. Russian. 6.Rykov SO, Vasiuta VA, Zadoianyi LV. [Retrospective analysis and clinical characteristics of patients with optic nerve atrophy]. Visnyk naukovykh doslidzhen’. 2012;(1):71-3. Russian. 7.Gorbunov AV, Bogomolova AA, Khavronina KV. [Ocular symproms as signs of brain damage]. Vestnik TGU. 2014;19(4):1108-10. Russian. 8.Zavgorodnia NG. [Ways for improving microcirculation in ocular ischemic syndrome]. Oftalmol Zh. 2008;(1):32-6. Russian. 9.Lazarev VV. [Visual abnormalities in discirculatory encephalopathy]. [Cand Sc (Med) Thesis]. Moscow; 2011. Russian. 10.Ryzhova IP. [Current aspects of endovascular treatment of central retinal artery embolism]. Oftal’mologiia. Vostochnaia Evropa. 2014;22(3):8-14. Russian. 11.Ryzhova IP, Shcheglov VI. [Information Bulletin No. 21, based on Pat. of Ukraine Patent of Ukraine №84,835 issued 11.11.2013. Method for treatment of patients with the vascular disorder of the visual system. Endovascular Neuroroentgensurgery Center, Academy of Medical Science of the Ukraine]. Ukrainian. 12.Makkaieva SM. [Features of ocular ischemic syndrome]. Abstract of Dr Sc (Med) Dissertation. Moscow; 2010. Russian. 13.Besditko PA, Shishkina DI. [On the neoroprotective treatment of anterior ischemic optic neuropathy]. Tavricheskii medico-biologicheskii vestnik. 2013;16(3): 26–28. Russian. 14.Zavgorodnia TS, Sarzhevska LE, Bezdenezhna OA, Bezugla EA. [Ocular ischemic syndrome. Current principles of diagnosis and treatment]. Zaporizhzha: Orbita-Iug; 2012. Russian. The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|