J.ophthalmol.(Ukraine).2019;3:20-25.
|
http://doi.org/10.31288/oftalmolzh201932025 Received: 18 March 2019; Published on-line: 27 June 2019 Qualitative assessment of the tear film in young adults I.M. Bezkorovaina, Dr. Sc. (Med.), Prof.; D.O. Nakonechnyi; Dun Fan Hui; A.O. Bezkorovaina Ukrainian Medical Stomatological Academy; Poltava (Ukraine) E-mail: ibezkor@gmail.com TO CITE THIS ARTICLE: Bezkorovaina IM, Nakonechnyi DO, Dun Fan Hui, Bezkorovaina AO. Qualitative assessment of the tear film in young adults. J.ophthalmol.(Ukraine).2019;3:20-5. http://doi.org/10.31288/oftalmolzh201932025 Introduction. Studying the quality of the tear film in young adults, who are the most active users of digital devices, is of extreme interest in clinical practice. Purpose. To study the qualitative characteristics of the tear film of the eye in young adults. Materials and Methods. We examined 486 eyes of 243 people, aged from 18 to 30, on average (23 ± 0.56). The Ocular Surface Disease Index was determined and the tests were performed in each patient. In addition, interferometry, tear meniscus and Non-invasive break-up time measurements were performed using the SBM ICP Tearscope (Italy) and iPad Pro (the USA) devices. Results. The examinees, aged 18-30, had the decreased tear film thickness, characterized by a positive correlation between the interferometry data and the tear production tests. The low (category I), moderate (category II), and high (III category) probability of dry eye disease was found in 35% (168 eyes), 31% (152 eyes), and 13% (65 eyes) of the examined young adults, respectively. Conclusions. Dry eye disease is a common chronic condition affecting the ocular surface in 38-64% of young adults. The thickness of the tear film lipid layer was decreased to 15 and 30-80 nm in 64% of cases; the tear meniscus was decreased in 42% of cases; and the tear film break-up time reduced in 57% of cases. It was possible to estimate the probability of dry eye disease in 79% of cases. Key words: interferometry, lipid layer thickness, tear meniscus, non-invasive break-up time
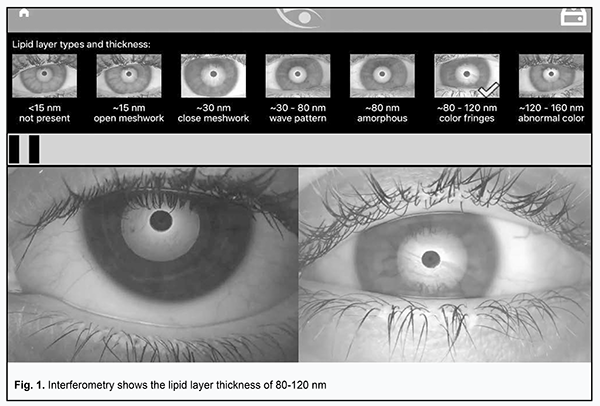
Introduction Dry eye disease (DED) is a chronic disease which affects millions of people worldwide. The incidence of DED ranges from 5 to 50% [8]. Such a wide range is due to the absence of the unified standard for DED diagnosis [11, 13, 14, 9, 2]. DED is more often described as a disease affecting older people [1]; however, the latest findings of international studies have demonstrated a demographic shift of DED [8]. This is facilitated by a multi-screen lifestyle, contact lens wear, refractive surgery complications, stress and other aspects which make the youngsters potential patients of an ophthalmologist [5, 3, 7]. Besides, there are significant difficulties in assessing the tear film, which make it complicated to study the ocular surface. They include the compensation of biological changes in the tear film composition by tear hypersecretion and the effect of diagnostic dyes on the tear break-up time, which lead to obtaining the false-positive results in standard testing methods. One of the recent methods to assess the quality and lipid layer thickness (LLT) of the tear film is interferometry. Based on the studies having assessed LLT in general population using a LipiView II Ocular Surface Interferometre, the data for interpretation have been determined as follows: more than 70 nm as norm; 70 to 50 nm as mild DED; and less than 50 nm as severe DED [12, 16]. However, in the available literature, there are no data on studying the qualitative state of the tear film in young adults, who are the most working-able users of digital gadgets, which gives the rationale for conducting the research in this area. Purpose. To study the quantitative characteristics of the tear film in young adults. Material and Methods The study was conducted at Otorhinolaryngology and Ophthalmology Department of Ukrainian Medical Stomatological Academy, Poltava, Ukraine. The study followed ethical and juridical principles according to World Medical Association Declaration of Helsinki. The exclusion group consisted of contact lens wearers, excimer-laser corrected patients, patients with inflammation of the eye and eyelid, and patients using any kind of eye drops. The study was performed within the autumn and winter period in a room with district heating; neither heaters nor air conditioner were used additionally. The temperature ranged from 20 to 23ºС, averaging 21.47±0.61 ºС; relative humidity ranged within 45-60%, averaging 53±1.5. The data obtained were recorded using a digital thermal hygrometer (Beurer HM16, Germany), thrice a day. 486 eyes of 243 patients, aged from 18 to 30 with an average of (23±0.56), were examined. Of them, there were 161 women (66%) and 82 men (345). To define the state of the ocular surface, each examinee was asked to complete the Ocular Surface Disease Index (OSDI) questionnaire, recommended by TFOS International Dry Eye WorkShop (DEWS II) [15]. The severity of symptoms was assessed by comparing the number of all questions answered with the sum of scores for all questions answered. The OSDI was evaluated using a formula: OSDI=Dx25/Е, where D is the sum of scores for all questions answered, and E is the number of questions answered. Afterwards, the corresponding shade of red was matched to the key below the chart to determine whether patient’s score indicated normal, mild, moderate, or severe dry eye disease. Then, each patient was performed interferometer measurements, tear meniscus measurements, the non-invasive break-up time (NIBUT) test using the devices SBM ICP Tearscope (Italy) and iPad Pro (the USA). The lipid layer thickness (LLT) was measured through analyzing interference images by a color profile of the pre-ocular tear film in the eyes blinking. The videos obtained were compared to the classification installed in the device and including seven short videos with different thicknesses of the tear film lipid layer (160-120 nm; 80-120 nm; 80 nm; 30-80 nm; 30 nm; 15 nm; <15 nm). The tear meniscus was measured using a high-power pre-shot image; result <0.22 mm was considered as deviation from the norm. In the NIBUT test, a special film was inserted into the interferometer to form Placido rings. A patient was encouraged to blink freely and, then, to stop blinking for as long as possible. The Placido rings image was projected on the eye and its deformation was monitored and video recorded. The time between the last complete blink and the first indication of pattern break-up and image deformation was measured. The result ≥ 10 s was considered as norm [10]. Video and image records were observed in real time on the iPad Pro screen using the ICP app by SBM Sistem and archived in the MacBook Air file database. The data obtained were interpreted by two independent experts at different time and the mean value was calculated for every statistical case. Also, lid-parallel conjunctival folds (LIPCOF) were evaluated biomicroscopically in the area of inferior lateral quadrant of the conjunctiva and basal tear production was defined using the Schirmer II test, following the 0.5% alcaine anesthesia. The data obtained were statistically processed using the STATISTICA 6.0 applied software package (StatSoft. Inc., the USA) and the EXEL descriptive statistics package. Results Low values of the OSDI, from 10.4 to 12.5 (an average of 11.4±0.63), were noted in most young adults, in 62% (151 persons), which was a characteristic of the normal ocular surface; mild DED was noted in 22% (54 persons), corresponding to the OSDI = 13.9-22.7 (an average of 16.8±1.92); moderate DED was noted in 16% (38 persons), corresponding to the OSDI = 25-31.3 (an average of 16.8±1.92); no severe DED was noted. The interferometry findings were different from the subjective perception. Thus, most examinees, 64% (310 eyes), had LLT disorders. Significant changes in the LLT was noted in 33% (218 eyes); of them, the LLT was minimal, 15 nm, in 10% (46 eyes). the LLT was 30 nm and 30-80 nm in 23% (112 eyes) and 31% (152 eyes), respectively. Normal values of the LLT were in 36% (176 eyes); of them, the LLT was 80 nm and 80-120 nm in 22% (109 eyes) and 14% (67 eyes), respectively (Fig. 1).
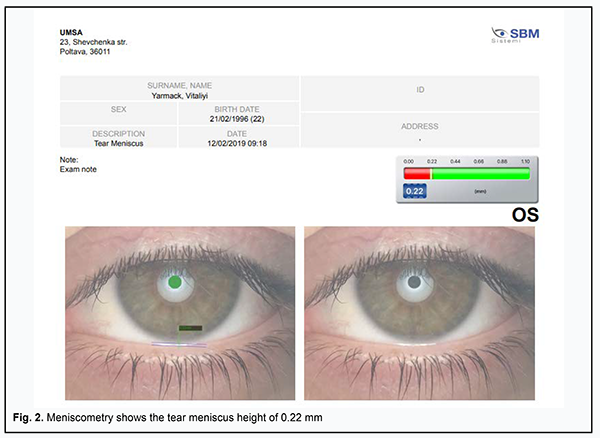
The tear meniscus height (TMH) measurements characterized the changes in the aqueous and mucin layers of the tear film. Thus, the TMH was <0.22 mm, an average of 17±0.12 mm (Fig. 2) in 42% (203 eyes); ≥0.22-25 mm, an average of 23±0.08 mm in 43% (211 eyes); and >0.25 mm, an average of 26.5±0.5 mm в 15% (72 eyes).
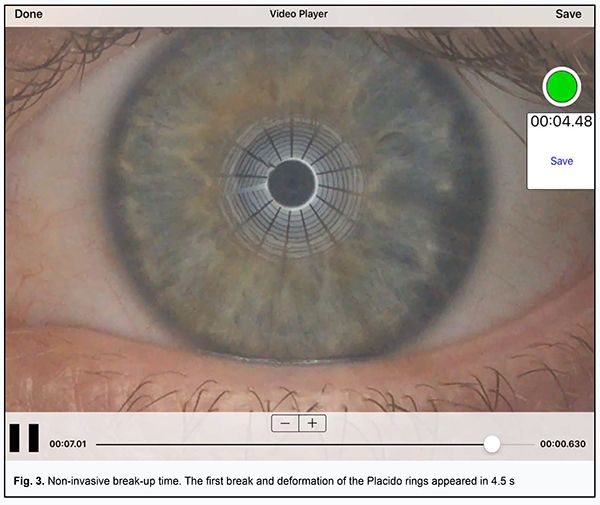
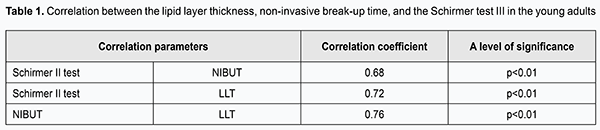
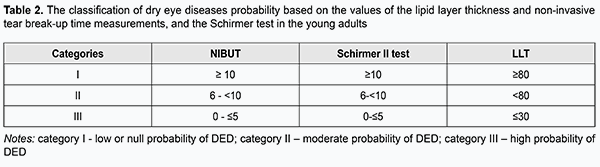
Tear film stability was assessed using the NIBUT test. Thus, toxicological effects of dyes were excluded. Tear film instability was noted in 57% (227 eyes). Thus, NIBUT was ≤5 s, an average of 4.6±0.06 s, in 13% (65 eyes); and <10 s, an average of 8.3±0.09 s, in 44% (212 eyes). Normal values of tear film stability were in 43% (209 eyes); of them, ≤15 s, an average of 13.7±0.05 s, in 23% (114 eyes); ≤20 s, an average of 17.9±0.1 s, in 20% (95 eyes). Lid-parallel conjunctival folds (LIPCOF) were evaluated biomicroscopically in the area of inferior lateral quadrant of the conjunctiva. LIPCOF-0, LIPCOF-1, LIPCOF-2 were revealed in 25% (123 eyes), 53% (259 eyes), and 21% (104 eyes), respectively; LIPCOF-3 was not revealed. Basal tear production was defined using the Schirmer II test, which showed disorders in 53% (259 eyes). Of them, the Schirmer II test values varied from 2 to 5 mm, averaging 4.13±0.02, in 16% (75 eyes) and from 6 to 10 mm, averaging 8.06±0.5, in 38% (184 eyes). Normal values of the Schirmer II test, >10 mm, were revealed in 47% (227 eyes); of them, 38% (182 eyes) had the Schirmer test value of 14±1.08, ranging from 10 to 15 mm, and 9% (45 eyes) had the Schirmer test value more than 15 mm, averaging 18±1.02. The data obtained demonstrate a significant correlation between the NIBUT, Schirmer and LLT tests (Table 1). Thus, the LLT ranged from 15 to 120 μm, the time of first deformation of the tear film was 3 to 20 s with an average of 11.43±3.45, and the Schirmer test showed from 2 to 21 mm per 5 min with an average of 9.04±3.28. The dependence between the above tests was positive and had a strong significant correlation (Table 2), which indicates that these tests can be used for qualitative assessment of the ocular surface.
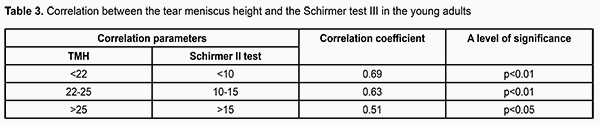
Based on the revealed correlation relationships, it was possible to make an interferometric classification to predict the occurrence of DED in young adults. According to the classification (Table 2), there are high rates of correlation on two sides of the LLT assessment scale in the SBM ICP Tearscope. When the LLT values were high, ≥80 nm in 36% (176 eyes), the NIBUT values were also increased and the Schirmer test values were increased in 35% (168 eyes) of 36% (176 eyes). When the LLT values were low, <80 nm in 64% (310 eyes), the NIBUT values were below the normal ranges in 54% (264 eyes) of 64% (310 eyes) and the Schirmer test values were below the norm in 52% (251 eyes) of 64% (310 eyes). These clinical findings are based on the tear film data obtained in young adults as specified in Table 2. They correspond to the statistical findings calculated from the whole set of data (Table 1). In addition, our findings demonstrate a significant correlation between the TMH values and the Schirmer test (Table 3). Thus, TMH varied from 0.13 to 0.27 mm with an average of 0.20±1.52 while the Schirmer test showed 2 to 21 mm per 5 minutes with an average of 9.04±3.28. Correlation between the tests above was positive and had a strong significant relationship (Table 3). When the TMH values were within the normal ranges, i.e. ≥0.22-0.25 mm in 43% (211 eyes), the Schirmer test was in norm in 37% (178 eyes). When the TMH values were low, i.e. <0.22 mm in 42% (203 eyes), the Schirmer test showed the decreased values in 42% (203 eyes). However, when the TMH values were increased, i.e. >0.25 mm in 15% (72 eyes), the Schirmer test showed an increase in 9% (45 eyes) and a decrease in 6% (27 eyes), which could testify to reflex tear flow or clinical insignificance of the values.
According to our interferometric classification, there is low probability for DED symptoms (category I) to occur in 35 eyes (168 eyes) while moderate (category II) and high (category III) probability of DED symptoms was noted, respectively, in 31% (152 eyes) and 13% (65 eyes) of the young adults examined. In 21% (101 eyes), it was not possible to match the data obtained with the classification, which once more gives the support to the fact that there is no single standard for DED diagnosis. Thus, this study showed that the tear film in young adults was characterized by the decreased lipid layer thickness, shortened tear film break-up time, decreased basal tear production, and the decreased tear meniscus height. This testifies to insufficient quality of the tear film in 44% (217 eyes) of the young adults studied, which brings them at high risk of DED and requires appropriate correction. To conclude, firstly, dry eye disease is a common chronic condition which affects the ocular surface of 38-64% of young adults. Secondly, the examination of young adults (18-30 y/o) showed a decrease in the tear film lipid layer thickness to 15 and 30-80 nm in 64%, a decrease in the tear meniscus height in 42%; and a shortening of tear film break-up time in 57%. Thirdly, it was possible to predict the probability of dry eye disease occurrence in 79%. References 1.Bezkorovayna IM, Nakonechnyi DO, Bezkorovayna AO. Characteristics of crystallographic changes in tear in different stages of diabetic retinopathy. J.ophthalmol.(Ukraine).2018;6:35-39. 2.Brzheskii VV, Egorova GB, Egorov EA. [Laboratory methods for diagnosis of dry eye syndrome]. In: [Dry eye syndrome ocular surface diseases]. 2016: 179-87. In Russian. 3.Zavgorodnya NG, Poplavska IO, Zavgorodnya TS, Litvinenko EE. [Treatment of dry eye syndrome manifistations using an Oxial drug in excimer-laser surgery]. Aktualni pytannya medychnoi nauky ta praktyky. Zaporizhzhya. 2009;75(2): 248-52. In Russian. 4.Maichuk DYu. [Pathogenetic Substantiation of treatment and prophylaxis of secondary tear formation disorders: Author’s thesis for Dr. of Med. Sc. M.;2005. 36p. In Russian. 5.Pimenidi MK, Polunin GS, Safonova TN. [Meibomian gland disfunction in computer vision syndrome]. Vestn. Oftalmol. 2010;6:49-52. In Russian. 6.Polunin GS, Polunina EG. [From dry eye to team film disease]. Oftalmologiia. 2012;9(44):78-84. In Russian. 7.Acosta M, Gallar J, Bellmonte C. The influence of eye solutions on blinking and ocular comfort at rest and during work at video display terminals. Expertimental Eye Research. 1999;68(6):663 – 9. 8.Craig JP, Nichols KK, Akpek EK et al. TFOS DEWS II Definition and Classification Report. Ocul Surf. 2017;15(3):276 – 83. 9.Farrand KF, Fridman M, Stillman IO, Schaumberg DA. Prevalence of diagnosed dry eye disease in the United States among adults aged 18 years and older. Am J Ophthalmol. 2017;182:90-8. 10.Fuller D.G. Noninvasive tear breakup times and ocular surface disease / D. G. Fuller, K. Potts, J. Kim. // Optom Vis Sci [PUBMED] – 2013 – 90 – P. 1086 – 1091 11.Galor A, Feuer W, Lee DJ et al. Prevalence and risk factors of dry eye syndrome in a United States veterans affairs population. Am J Ophthalmol. 2011;152(3): 377-84. 12.Ji Won Jung, Si Yoon Park, Jin Sun Kim at al. Analysis of factors associated with the tear film lipid layer thickness in normal eyes and patients with dry eye syndrome. IOVS 2016;57(10):223 – 7. 13.Paulsen AJ, Cruickshanks KJ, Fischer ME et al. Dry eye in the beaver dam offspring study: prevalence, risk factors, and health-related quality of life. / A. J. Paulsen. Am J Ophthalmol. 2014;157(4):799 – 806. 14.Tan LL, Morgan P, Cai ZQ, Straughan RA. Prevalence of and risk factors for symptomatic dry eye disease in Singapore. Clin Experiment Optom. 2015;98(1):45-53. 15.TFOS DEWS II - Diagnostic Methodology. Available at: https://www.tfosdewsreport.org/report-diagnostic_methodology/131_36/en/#... 16.Zhao Y, Tan CL, Tong L. Intra-observer and inter-observer repeatability of ocular surface interferometer in measuring lipid layer thickness. BMC Ophthalmol. 2015; 15:53. The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|