J.ophthalmol.(Ukraine).2019;2:33-38.
|
http://doi.org/10.31288/oftalmolzh201923338 Received: 21 January 2019; Published-online: 24 April 2019 Results of vitreous surgery with 20% C3F8/air mixture for macular holes larger than 800 μm A.A. Putienko, Dr Sc (Med) Filatov Institute of Eye Disease and Tissue Therapy; Odessa (Ukraine) E-mail: alputienko@gmail.com TO CITE THIS ARTICLE: Putienko AA. Results of vitreous surgery with 20% C3F8/air mixture for macular holes larger than 800 μm. J.ophthalmol.(Ukraine).2019;2:33-8. http://doi.org/10.31288/oftalmolzh201923338 Background: Vitreous surgery for large macular holes is still a challenge to the ophthalmologist. Purpose: To assess the efficacy of the 20% C3F8/air mixture in the vitrectomy surgery for macular holes > 800 μm in diameter. Materials and Methods: Twenty-two patients with macular hole of diameter ranging from 800 to 1,470 μm underwent vitrectomy with internal limiting membrane (ILM) peeling and tamponade with the 20% C3F8/air mixture. Results: At 2 months after gas resorption, the macular hole was completely closed in 20 of the 22 eyes (90.9%). In addition, diameter of the hole dropped from 1,100 μm to 150 μm in one eye, and the hole did not close in another eye. Visual acuity improved significantly (χ2 = 13.15, p = 0.001) to 0.08-0.35. In 3 eyes, 12 eyes and 7 eyes, visual acuity improved to 0.05 – 0.08, 0.09 – 0.12, and 0.14 – 0.35, respectively. Conclusion: The study demonstrated a high efficacy of the 20% C3F8/air mixture in the treatment of macular holes > 800 μm in diameter. Keywords: macular hole larger than 800 μm; vitreous surgery; tamponade with the 20% C3F8/air mixture
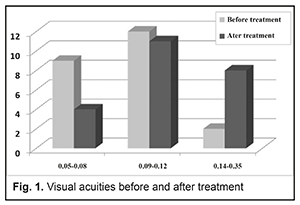
Introduction The population prevalence of macular holes is estimated to be 0.05%. The prevalence of idiopathic macular holes in individuals above 60 years is up to 0.3%, with a female-to male ratio varying from 1.8 to 1 to 3 to 1 [1, 2]. Gass has proposed a four-stage system of identifying idiopathic macular holes [3]. Stage 1A: Foveal detachment. Macular cyst. Tangential vitreous traction results in the elevation of the fovea marked by increased clinical prominence of xanthophyll pigment. This stage is occasionally referred to as the yellow dot stage. Stage 1B: As the foveal retina elevates to the level of the perifoveal, the yellow spot of xanthophyll pigment changes to a yellow ring. Persistent traction on the fovea leads to dehiscence of deeper retinal layers at the umbo. Stage 2: This is the first stage when a full-thickness break in the retina exists. It is defined as a full-thickness macular hole less than 400 µm in size. The full-thickness defect may appear eccentric, and there may be a pseudo-operculum at this stage. These opercula have been examined and found to be vitreous condensation and glial proliferation without harboring any retinal tissue. Stage 3: A full-thickness macular hole in the retina exists. It is greater than 400 µm in size and is still with partial vitreomacular traction. Stage 4: A full-thickness macular hole exists in the presence of a complete separation of the vitreous from the macula and the optic disc. There is recent evidence, however, that, even in the presence of an apparent posterior vitreous detachment, a thin shell of residual cortical vitreous may still remain and contribute to the macular hole. Surgical macular hole repair without internal limiting membrane (ILM) peeling was first reported in 1991, with macular reattachment achieved in 58% and an improvement in visual acuity of two lines or better attained in 42% of eyes [4]. Current macular hole repair techniques with the use of short acting gases for tamponade allows achieving a rate of hole closure of almost 100% for stage 2 [1, 5] and 69% for stage 3 or 4 macular holes [6, 7]. In addition, a hole rate closure for macular holes > 600-800 μm in diameter varies from 50 to 87% [8, 9]. In the inverted ILM flap technique, an ILM remnant attached to the margins of the macular hole is left in place and then inverted upside-down to cover the macular hole. This technique has demonstrated an improved hole closure rate for large macular holes [10, 11]. The surgical approach based on the formation of retinal detachment in the posterior pole with creation of additional radial breaks in order to relax the retina is rather traumatic [12, 13]. Therefore, there is a need for new approaches to treatment of macular holes. The purpose of the study was to assess the efficacy of the 20% C3F8/air mixture in the vitrectomy surgery for macular holes > 800 μm in diameter. Materials and Methods Twenty two patients (14 women and 8 men; mean age, 69.6 SD (14.3) years) with a macular hole diameter ranging from 800 to 1,470 μm were involved in the study. OCT-based assessment of macular hole size was performed taking into account the maximum area of free RPE. The duration of the macular hole exceeded 6 months in all affected eyes. At baseline, visual acuity ranged from 0.04 to 0.23, 5 eyes had dry age-related macular degeneration, 14 eyes were phakic and 8 eyes were pseudophakic. A routine three-port approach was used to perform the intravitreal procedure with a 25+ Alcon CONSTELLATION® vitreous cutter (Alcon, Fort Worth, TX). First, vitrectomy with stripping of the posterior hyaloid to the equator was performed. The vitreous was stained with Brilliant Peel® Dual Dye, if required. The same dye was then used to stain the ILM. The ILM was peeled to half a distance between the outer optic disc margin and the foveola. Thereafter, injection of sterile air into the vitreous cavity was performed with simultaneous aspiration of the aqueous humor from the bed of the macular hole for at least 5 minutes. Finally, vitreous tamponade with the 20% C3F8/air mixture was performed. Routine variational statistics methods were used. Chi-square analysis (χ2) was used to assess nonparametric data. Results and Discussion No intraoperative complications were observed. In the early post-operative period, no complications were observed, and the percentage of gas in the vitreous was at least 75%. Patients maintained face-down position for 10-12 days after surgery. At 2 months after gas resorption, the hole was completely closed in 20 (90.9%) of the 22 patients. In addition, diameter of the hole dropped from 1,100 μm to 150 μm in one eye, and the hole did not close in another eye. Visual acuity improved significantly (χ2 = 13.15, p = 0.001) to 0.08-0.35. In 3 eyes, 12 eyes and 7 eyes, visual acuity improved to 0.05 – 0.08, 0.09 – 0.12, and 0.14 – 0.35, respectively. Visual acuities before and after treatment are represented in Fig. 1.
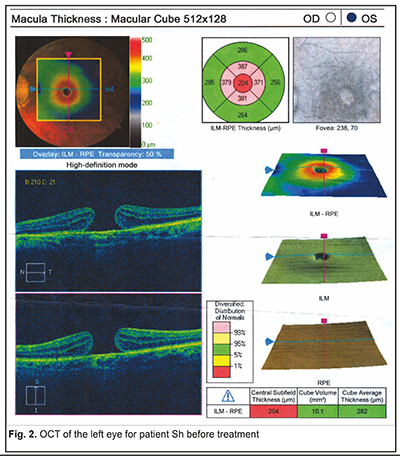
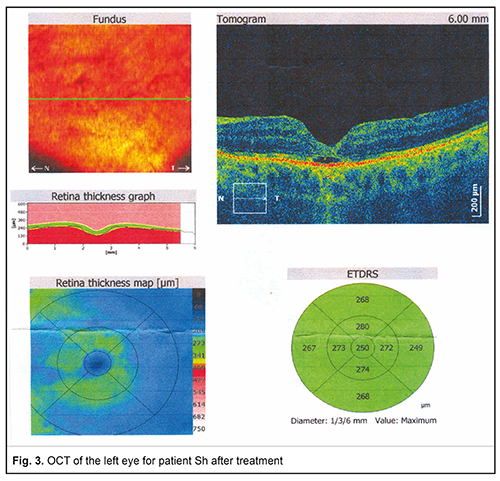
ILM removal results in retinal tissue relaxation and filling the site of bare RPE (the major mechanism of macular hole closure). It is known that the longer the time the macular hole is in contact with the gas bubble only, the higher is the chance for macular hole closure [5, 14]. The importance of adequate tamponade of macular hole edges has been confirmed in the study by Shimada et al [15] who determined adherence to face-down positioning (FDP) among patients who underwent vitrectomy and gas tamponade for macular hole (MH) repair. Nurses recorded whether the patient complied with FDP each time they examined the patient. FDP score was obtained from the nursing records; patients were given a score of 1 if they complied with the FDP and 0 if they did not. The score was recorded four times per day for the first 3 postoperative days. A perfect FDP score was 12. The closure rate in patients with FDP score <7 was significantly lower than in patients with an FDP score >7 [15]. In the current study, the use of the 20% C3F8/air mixture enabled a long lasting tamponade of the macular hole, with a hole closure rate of 91%. Our previous experience has demonstrated that, with the C3F8 of such concentration used in gas-air mixture, the percentage of vitreous cavity gas fill was greater than 50% for at least 3 postoperative weeks, and, if the patient poorly adhered to the face-down positioning after macular hole surgery, the volume of the gas bubble remained large enough to make an effective tamponade of the macula, which is an essential advantage of this approach. Studies have been reported on vitrectomy for large diameter macular holes, but most of them are related to functional and anatomic outcomes of vitrectomy for macular holes with a diameter greater than 400 μm [1, 16]. Yamashita et al [17] reported on the efficacy of surgery for macular holes with a diameter greater than 550 μm. Wong et al [13] reported the outcomes of vitrectomy for macular holes with a diameter of at least 650 μm. Because the current study involved 22 patients who underwent surgery for macular holes with a diameter greater than 800 μm, it is rather difficult to compare this study with other reports evaluating treatment outcomes of vitrectomy for large macular holes. Most of the studies compare the inverted ILM flap technique with the classic macular hole surgery with regard to efficacy. Michalewska et al [10] and Mahalingam and Sambhav [11] found the former to be more efficacious, but Kannan et al [18] found no significant difference between the two approaches with regard to closure rate for macular holes with a diameter greater than 600 μm. A number of studies involved patients that underwent of vitrectomy for macular holes of different diameters (including large diameters), and compared different tamponade agents with regard to treatment outcomes. No significant difference in closure rate for large diameter macular holes or for stage 3 or 4 macular holes has been found between sulfur hexafluoride (SF6) or perfluoropropane (C3F8) tamponade groups [14,19]. Kim et al [20], however, have found macular hole surgery with the 15% C3F8/air mixture to be more beneficial than that with the 20% SF6/air mixture with regard to visual outcomes. Rao et al [21] have reported the efficacy and safety of outpatient fluid-gas exchange with 15% C3F8 or 20% SF6 for open macular hole after primary vitrectomy. They found that of the 36 eyes, 32 (89%) achieved anatomic success. In addition, the success rate for macular hole surgery has been found to depend on the duration of intraocular gas tamponade [22]. Therefore, the current study demonstrated a high efficacy of the 20% C3F8/air mixture in the treatment of macular holes > 800 μm in diameter. These findings indicate that the approach has the potential for wide use in clinical practice. Example cases A 75-year-old woman with a 850-μm diameter macular hole and visual acuity of 0.07 in her left eye (OCT, Fig. 2) underwent vitrectomy with ILM peeling and tamponade with the 20% C3F8/air mixture. The macular hole was found to be closed, and visual acuity improved to 0.17 (Fig. 3) at 2 months after surgery.
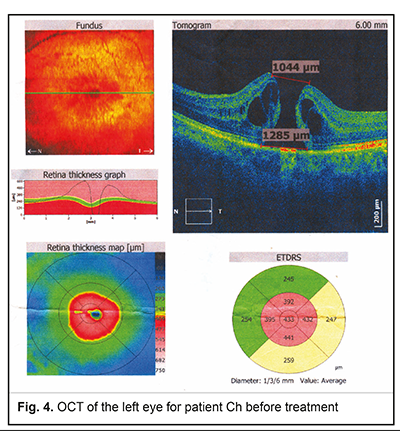
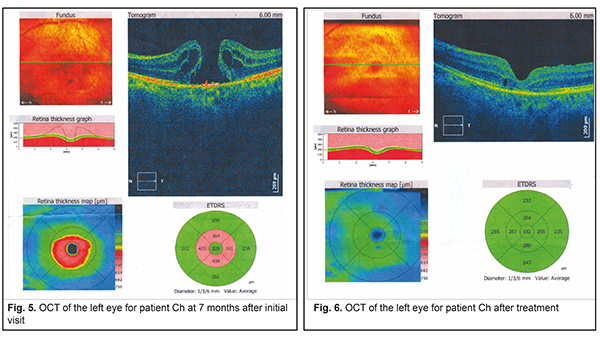
A 63-year-old woman presented with a macular hole in the left eye. Her visual acuity in the affected eye was 0.09, and the hole was 1,200 µm in diameter (Figure 4), but the patient declined surgery. Seven months after presentation, the macular hole enlarged to 1,300 µm (Fig. 5), the patient’s visual acuity decreased to 0.06, and she underwent vitrectomy with ILM peeling and tamponade with the 20% C3F8/air mixture. The macular hole was found to be closed, and visual acuity improved to 0.17 (Fig. 6) at 2 months after surgery.
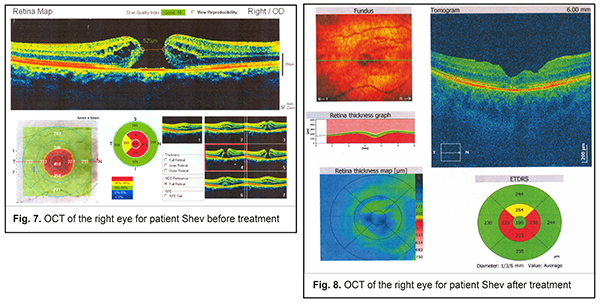
A 59-year-old presented with a macular hole of 4 months duration in the right eye. Her visual acuity in the affected eye was 0.08, and the hole was more than 900 µm in diameter (Figure 7). She underwent vitrectomy with ILM peeling and tamponade with the 20% C3F8/air mixture. The macular hole was found to be closed, and visual acuity improved to 0.2 (Fig. 8) at 1.5 months postoperatively.
References 1.Kang HK, Chang AA, Beaumont PE. The macular hole: report of an Australian surgical series and meta-analysis of the literature. Clin Exp Ophthalmol. 2000 Aug;28(4):298–308. 2.Mc Cannel CA, Ensminger JL, Diehl NN, et al. Population-based incidence of macular holes. Ophthalmology. 2009 Jul;116(7):1366–9. 3.Gass JD. Reappraisal of biomicroscopic classification of stages of development of a macular hole. Am J Ophthalmol. 1995 Jun;119(6):752–9. 4.Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol. 1991 May;109(5):654–9. 5.Gander IC, Senn P, Lüthi M, Schipper I. [Prognostic factors and results after surgical treatment of idiopathic macular holes, stage 2 and 3]. Klin Monbl Augenheilkd. 2000 May;216(5):272–7. German. 6.Freeman WR, Azen SP, Kim JW, et al. Vitrectomy for the treatment of full-thickness stage 3 or 4 macular holes. Results of a multicentered randomized clinical trial. The Vitrectomy for Treatment of Macular Hole Study Group. Arch Ophthalmol. 1997 Jan;115(1):11–21. 7.Tadayoni R, Gaudric A, Haouchine B, Massin P. Relationship between macular hole size and the potential benefit of internal limiting membrane peeling. Br J Ophthalmol. 2006 Oct; 90(10): 1239–41. 8.Jackson TL, Donachie PH, Sparrow JM, Johnston RL. United Kingdom National Ophthalmology Database study of vitreoretinal surgery: report 2, macular hole. Ophthalmology. 2013 Mar;120(3):629–34. 9.La Cour M, Friis J. Macular holes: classification, epidemiology, natural history and treatment. Acta Ophthalmol Scand. 2002 Dec;80(6):579–87. 10.Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010 Oct;117(10):2018–25. 11.Mahalingam P, Sambhav K. Surgical outcomes of inverted internal limiting membrane flap technique for large macular hole. Indian J Ophthalmol. 2013 Oct;61(10):601-3. 12.Charles S, Randolph JC, Neekhra A, et al. Arcuate retinotomy for the repair of large macular holes. Ophthalmic Surg Lasers Imaging Retina. 2013 Jan-Feb;44(1):69-72. 13.Wong R, Howard C, Orobona GD. RETINA EXPANSION TECHNIQUE FOR MACULAR HOLE APPOSITION REPORT 2: Efficacy, Closure Rate, and Risks of a Macular Detachment Technique to Close Large Full-Thickness Macular Holes. Retina. 2018 Apr;38(4):660-663. 14.Casini G, Loiudice P, de Cillà S, et al. Sulfur hexafluoride (SF6) versus perfluoropropane (C3F8) tamponade and short term face-down position for macular hole repair: a randomized prospective study. Int J Retina Vitreous. 2016 Apr 1;2:10. 15.Shimada Y, Seno Y, Mizuguchi T, et al. Patient adherence to the face-down positioning after macular hole surgery. Clin Ophthalmol. 2017 Jun 8;11:1099-1104. 16.Pak KY, Park JY, Park SW, et al. Efficacy of the Perfluoro-N-Octane-Assisted Single-Layered Inverted Internal Limiting Membrane Flap Technique for Large Macular Holes. Ophthalmologica. 2017;238(3):133-138. 17.Yamashita T, Sakamoto T, Terasaki H, et. al. Best surgical technique and outcomes for large macular holes: retrospective multicentre study in Japan. Acta Ophthalmol. 2018 Dec;96(8):e904-e910. 18.Kannan NB, Parida H, et. Comparative study of inverted internal limiting membrane (ILM) flap and ILM peeling technique in large macular holes: a randomized-control trial. BMC Ophthalmol. 2018 Jul 20;18(1):177. 19.Briand S, Chalifoux E, Tourville E, et al. Prospective randomized trial: outcomes of SF6 versus C3F8 in macular hole surgery. Can J Ophthalmol. 2015;50:95–100. 20.Kim SS, Smiddy WE, Feuer WJ, Shi W. Outcomes of sulfur hexafluoride (SF6) versus perfluoropropane (C3F8) gas tamponade for macular hole surgery. Retina. 2008 Nov-Dec;28(10):1408-15. 21.Rao X, Wang NK, Chen YP, et. al. Outcomes of outpatient fluid-gas exchange for open macular hole after vitrectomy. Am J Ophthalmol. 2013 Aug;156(2):326-333.e1. 22.Thompson JT, Smiddy WE, Glaser BM, et al. Intraocular tamponade duration and success of macular hole surgery. Retina. 1996;16(5):373-82.
The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|