J.ophthalmol.(Ukraine).2019;2:70-76.
|
http://doi.org/10.31288/oftalmolzh201927076 Received: 13 February 2019; Published-online: 24 April 2019 Coloboma of the optic disc: a case report N.V. Konovalova, Dr. Sc. (Med.); N.I. Khramenko, Cand. Sc. (Med.); S.B. Slobodyanyk, Cand. Sc. (Med.); O.V. Guzun, Cand. Sc. (Med.) SI “The Filatov Institute of Eye Diseases and Tissue Therapy, NAMS of Ukraine”; Odessa (Ukraine) E-mail: kvnkonovalova@gmail.com TO CITE THIS ARTICLE: Konovalova NV, Khramenko NI, Slobodyanyk SB, Guzun OV. Coloboma of the optic disc: a case report. J.ophthalmol.(Ukraine).2019;2:70-6. http://doi.org/10.31288/oftalmolzh201927076 Clinical manifestations of coloboma and a pit of the optic disc are variable, which conditions the need for differentiated diagnosis of this rare pathology and proper treatment. The article describes characteristics of diagnosis and clinical course of optic nerve coloboma in dynamics. Keywords: coloboma of the optic nerve disk
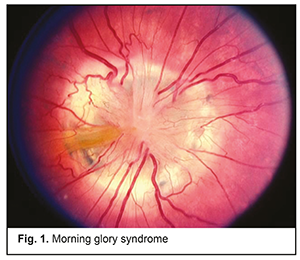
Introduction Coloboma of the optic nerve is an unprogressive congenital anomaly in which there is a defect of the optic disc filled with retinal cells. It occurs in 0.075 % of people [1, 2]. Congenital colobomas of the optic nerve and other ocular tissues are associated with incomplete or abnormal position of the proximal ends of the optic fissure, which, in the normal eye, begins to close in the fourth-fifth week of fetal development. Abnormal or incomplete closure of the optic fissure results in a defect of ocular layers and in congenital coloboma of the optic disk. Defects can be located in various ocular structures: in the iris, choroid, retina, and optic nerve. The optic nerve, and, more precisely, optic disc and fibres, form from the third to tenth week of fetal development. Any disorders in embryogenesis within this period of time lead to anomalies of the optic nerve such as coloboma, hypoplasia, gliosis, and pseudoneuritis. The disease can be passed in the autosomal dominant mode of inheritance and is of a sporadic character. In some cases, mothers of children who were revealed an anomaly took opiates across pregnancy or had an intrauterine cytomegalovirus disease [5, 6, 7]. One of the optic nerve coloboma complications is increased cupping of the optic disc, even when the intraocular pressure is in the norm, and a thinning of the neural rim. Besides, nonrhegmatogenous retinal detachment develops in some cases as well as serous macular detachment, the pathogenesis of which is still unclear. Some authors, based on optical coherent tomography, have been convincing in demonstrating a timeline of serous macular detachment stages in patients with optic nerve anomalies [8, 7]. As a rule, dissection of the outer and inner retinal layers and macular detachment develop against the background of full-thickness macular hole, preceded by macular edema. Similar complications are quite often observed in patients with an optic nerve pit. Another optic nerve coloboma-associated complication, which is quite rare, is a peripapillary subretinal neovascular membrane. The pathogenesis of peripapillary subretinal neovascular membranes is unclear. This complication usually occurs in people aged between 40 and 50 [3, 4, 9]. There are three types of optic nerve coloboma according to central retinal vessel patterns. Type 1 is characterized by blood vessels seen emanating from the inferior border of the defect. In type 2, blood vessels are seen in the center or near the superior border. Type 3 is characterized by homogeneous distribution along the whole border of the defect. Visual acuity in the presence of coloboma can vary from completely preserved to total blindness. Visual function depends on the size and location of a defect. With coloboma located at the papillomacular bundle, visual acuity is low. When coloboma is located in the nasal part of the disc, visual acuity can be high, frequently reaching 1.0. Quite often, optic nerve coloboma is diagnosed in a patient together with microphthalmos, choroidal coloboma, and other ocular anomalies [10, 6, 11] Types of coloboma according to the time of its appearance: 1.Congenital coloboma develops in consequence of damaging factors affecting the eye anlage. As a result, the embryonic fissure fails to closure completely and the forming structures are formed improperly. 2.Acquired coloboma develops when the eyeball is damaged. Being injured, some portions can lose viability and necrotize. A postoperative defect is also referred to as acquired coloboma. Anatomical investigations have shown that, in most cases, the structure of the optic nerve is not changed in the presence of coloboma. Ophthalmoscopically, an ophthalmologist reveals a typical picture of cyst-like scleral ectasia located in the inferior entrance of the optic nerve. In the actasia area, the pigment epithelium and choroid is absent. Herewith, retinal elements are preserved to a greater or lesser degree. It is more rare that disorders are noted in the optic nerve and optic nerve layers. In other words, in fact, coloboma of the optic nerve is more like an ectatic cyst of the choroid or an underdeveloped orbital cyst. Thus, some scientists, for example, von Hippel, consider such anomalies not colobomas of the optic nerve but defects in the optic nerve entrance [3, 10, 2]. A more rare form of optic nerve coloboma is peripapillary staphyloma. Herewith, the optic papilla is placed in the deepening of a regular cylindrical form. Isolated coloboma of the optic nerve should be differentiated from morning glory syndrome. Morning glory syndrome is a rare congenital anomaly of unknown etiology, usually unilateral [5, 6]. The disc has a cone shape, a whitish mass in the centre, a pigment rim around the disc. Small branching of retinal vessels is seen along the disc border (Fig. 1).
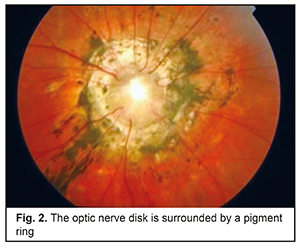
Approximately 100 cases of morning glory syndrome have been reported in the literature. The anomaly was first described by W. Reis in 1908, and Handmann reported on six more patients with this rare syndrome in 1929. Such an unusual name was given to a syndrome after P. Kindler had published an article with wonderful illustrations (1970) where he described 10 children with changes in the fundus which looked like a morning-glory flower [4, 9]. The disease is almost always unilateral and almost twice more often occurs in women than in men. There are single reports on bilateral defects, the authors of which suggest the inherited nature of the anomaly. In the case of a unilateral defect, the right eye is affected more frequently (in 60%). Family cases of morning glory syndrome are extremely rare. A case of trisomy 4q syndrome in combination with unilateral morning glory syndrome has been reported. Coloboma is often surrounded by pigmentary deposits [11, 8]. The size of coloboma most commonly is significantly higher than the diameter of the optic nerve (Fig. 2). A bottom of the deepening is uneven and has several levels. Coloboma is pink at the top and white throughout the rest of it.
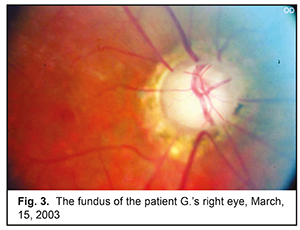
Choroidoretinal colobomas should be distinguished from focal spots of toxoplasmic or other choroidal atrophy located in the inferior fundus. The latter usually have pigmentation in the centre of an atrophic focus. Visual acuity is usually impaired in patients with optic disc coloboma. In choroidoretinal coloboma, there is a visual field defect corresponding to the location of coloboma [7, 12]. At the present time, there is no preventive treatment for colobomas. Photocoagulation of the neovascular membrane is required in the presence of complications as choroidal neovascularization; and surgical treatment (vitrectomy, gas tamponade, photocoagulation of the edges of the macular hole) is performed for retinal detachment. Purpose of the present paper was to view the characteristics of diagnosis and course of optic nerve coloboma in dynamics using a clinical example. Material and Methods A sixty-one-year-old patient with optic nerve coloboma in the right eye had been followed up for 32 years at Department for Inflammation Diseases in the Filatov Institute of Eye Diseases and Tissue Therapy. The examination included visual acuity testing, the activity of axial bundles, macular scanning of the papillomacular bundle activity, phosphene current threshold, tonometry, ophthalmic rheography, perimetry, ophthalmoscopy, optical coherent tomography (OCT), fluorescein angiography (FAG). Computed rheoophthalmography (ROG) was performed using a REOCOM rheograph (Kharkiv, Ukraine) and rheographic quotient, RQ (‰), was determined. RQ is a parameter indicating a volume of blood which enters the eye within a cardiac cycle and tonic properties of large (α 1/Т) and small (α 2/Т) vessels. Humphrey Visual Field Analyzer II 750i (Carl Zeiss) was used to measure visual fields; threshold programs SITA Central 30-2 and Peripheral 60-4 were used to measure central and peripheral visual fields, respectively. Findings were assessed visually and based on the values of retinal light sensitivity (dB) using Mean Deviation (MD), Рattern Standart Deviation (PSD), and Visual Field Index (VFI). Results and Discussion Taking into account a low rate of the disease incidence, we decided to review, based on a clinical case, characteristics of diagnosis and course of optic nerve coloboma. A patient G., born in 1957, first applied to the Department for Inflammatory Diseases in 1987 and complained of poor vision in both eyes. Vision in the left eye had been poor since his childhood. The patient was diagnosed: coloboma of the optic disc in the right eye; high hyperopia and refractive amblyopia in the left eye. The patient was recommended a follow-up by an ophthalmologist. The next follow-up visit was in 2013. Uncorrected visual acuity (UCVA) was 0.25 in the right eye and 0.02 in the left eye; OU intraocular pressure (IOP) by Makhlakov was 18 mmHg; refraction testing showed emmetropia in the right eye and +5.0 D hyperopia in the left eye. Biomicroscopy in both eyes showed a smooth spherical transparent cornea and phacosclerosis. Ophthalmoscopy of the right eye showed that the pink optic nerve disc of the right eye was significantly increased and located in a cone-like deepening. The bottom of the deepening was uneven and levelled. Coloboma was pink in the superior part and white in the rest of it. Excavation-surrounding borders of the retina have irregularly protruding edges; retinal pigmentation was not destroyed. In the centre of the deepening above the defect there was a white glial tissue. Vessels in the disc appeared closer to the deepening edges; there was a vessel angulation in the peripapillary area and an abnormally forward stroke of retinal vessels with a tendency to branch at an acute angle. Dystrophic foci were located on the retina parapapillaryly, along vascular arcades (Fig. 3). Ophthalmoscopy of the left eye showed that the optic disk was pink with sharp contours, constricted arteries, and tense kinked veins.
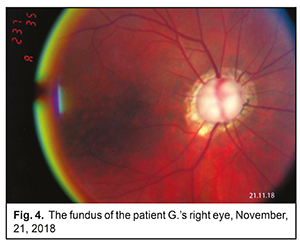
Based on the diagnostic findings, the patient was diagnosed: coloboma of the optic nerve disc in the right eye; and high hyperopia and refractive amblyopia in the left eye. The next follow-up visit was on the 21st of November 2018. UNVA was 0.2 and 0.02 in the right and left eyes, respectively; Makhlakov IOP was 18 mmHg in both eyes; refraction testing showed emmetropia in the right eye and +5.0 D hyperopia in the left eye. Objectively, the cornea was transparent, spherical, and smooth in both eyes; phacosclerosis was noted. Ophthalmoscopy of the right eye showed that the pink optic nerve disc was significantly increased and located in a cone-like deepening with an uneven bottom. In the centre of the deepening there was a white glial tissue above the defect. Vessels in the disc appeared closer to the deepening edges; there was a vessel angulation in the peripapillary area and an abnormally forward stroke of retinal vessels with a tendency to branch at an acute angle. There was a ring of scleral staphyloma with pigment deposits. Dystrophic foci with sharp contours were noted parapapillaryly, along vascular arcades (Fig. 4). Ophthalmoscopy of the left eye showed the same picture with the pink optic disk, sharp contours, constricted arteries, and tense kinked veins.
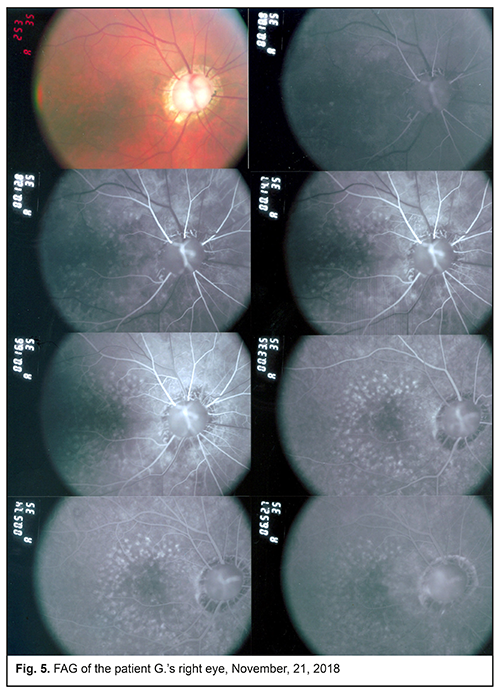
FAG findings showed that the optic disk was increased, rounded, and surrounded by a wide ring of scleral staphyloma (Fig. 5). The parapapillary tissue was depigmented with defects of retinal pigment epithelium located parapapillaryly along vascular arcades. Optic disc coloboma looked like an area of hypofluorescence at early and intermediate stages and an area of hyperfluorescence at a late stage. There are numerous retinal vessels around the disc which come out from the disc at the level of its edge.
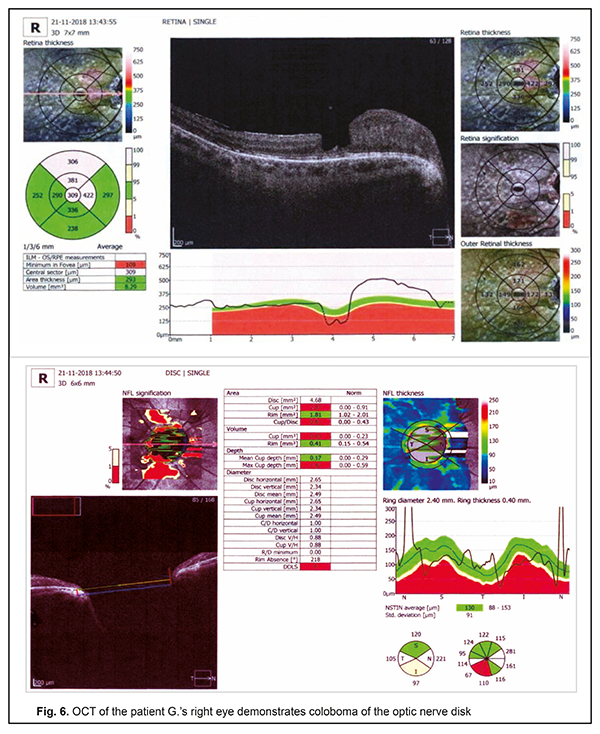
Ultrasound B-scanning revealed a deep defect in the anterior pole. Thus, the anterior pole was protruded by optic nerve structures and a proximal portion of the optic nerve was insignificantly enlarged in the site of its contact to the sclera. Magnetic resonance imaging showed the presence of ipsilateral hypoplasia of the intracranial optic nerve. Electrophysiology studies showed that ERG wave amplitudes were within normal ranges; the Р100 amplitude of pattern visually evoked potential was decreased; the implicit time was prolonged. OCT findings made it possible to reveal the presence of optic disc coloboma in the excavation deepening in the shape of a vertical oval with sharply reflecting walls and surrounded by a pigmented rim. The size of this deepening greatly exceeded a cross-section of the optic papilla. The bottom of the excavation was multi-levelled. It was the deepest in the inferior aspect. Neuroepithelium was thinned in the posterior pole along the vascular arcades (Fig. 6).
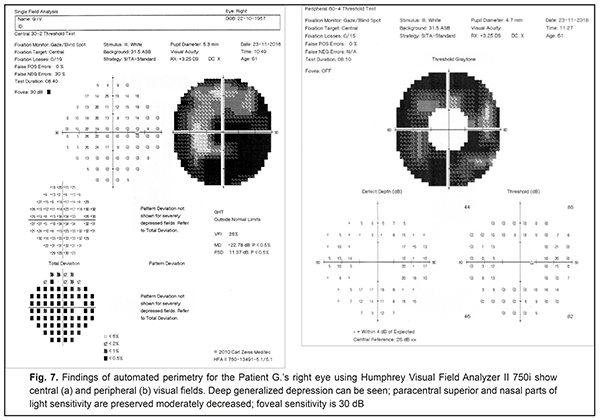
Deep generalized depression was noted in the visual field of the right eye; paracentral superior and nasal parts of light sensitivity were preserved moderately decreased (Fig. 7). MD was 22.78 dB; PSD equalled 11.37 dB; and VFI was 25%. Foveal sensitivity was preserved at the level of 30 dB. The visual field of the left eye was within normal ranges.
Conclusion Based on the findings of ophthalmoscopy, OCT, FAG, visual field testing, the patient had secondary macular degeneration, thinning of the neuroepithelium, pigment epithelium defects. In this regard, the patient was prescribed Ocuvite Complete, 1 capsule a day for 6 months. A capsule of Ocuvite Complete contains: fish oil, 421.5 mg, including that which contains Omega-3 fatty acids (250 mg): fish oil containing docosahexaenoic (175 mg) and eicosapentaenoic (24 mg) acid; vitamin E, 15 mg; zinc, 7.5 mg; vitamin C, 90 mg; zeaxanthin, 1 mg; and lutein, 5 mg. Some investigations have demonstrated that the low optical density of the macular pigment in the retina correlates with development of age-related macular degeneration (AMD). This fact has been confirmed by the National Eye Institute (the USA) in the Age-Related Eye Disease Study (AREDS II), which aimed to study the efficacy of using lutein, zeaxanthin, and polyunsaturated fatty acids in ophthalmology. The mechanism by which lutein and zeaxanthin are involved in the prevention of dystrophic eye disorders can be associated with their physical blue light filtration properties and local antioxidant activity [13]. Our previous papers have shown that using lutein and zeaxanthin-containing drugs for AMD patients resulted in increased and stabled visual acuity and the improved functional activity of the visual system. Thus, photopic light sensitivity increased to 86%; the afferent system of the fovea, based on the Haidinger's brush threshold, improved by 10.9% [14]. Docosahexaenoic acid (DHA) is the predominant omega-3 polyunsaturated fatty acid which is a component of the brain structure and can affect neurological function by modulating signal transduction pathways, neurotransmission, neurogenesis, myelination, synaptic plasticity, membrane integrity, and membrane organization. [15]. DHA improves the afferentation of visual processes. Dystrophic retinal changes in our patient were, apparently, due to fluid penetration, macular and paramacular edema, and, consequently, secondary macular degeneration. The pathway of the fluid leakage into the subretinal space has not yet been clearly identified. According to the literature, it can be from the vitreous body, from the subarachnoid cavity of the optic nerve, and from abnormal vessels in the coloboma basement [11, 7, 12]. Analyzing our clinical case, the source of fluid leakage can be the subarachnoid cavity. Due to the great variability of clinical manifestations, it is necessary to be aware of this rare pathology, and consider the possible presence of coloboma or a pit of the optic nerve disk in case of central serous retinal detachment occurred spontaneously or against the surgical treatment. Coloboma complications are unremovable defects. And in advanced coloboma, they can cause severe complications, including rhegmatogenous and serous retinal detachment and increased optic disc excavation. So, it should be remembered that permanent monitoring of the disease by an ophthalmologist can prevent complications. To prevent particular complications associated with optic nerve coloboma and secondary macular degeneration, it is reasonable to prescribe a six-month supplement using Ocuvite Complete, 1 capsule a day. References 1.Apple DJ, Rabb MF, Walsh PM. Congenitial anomalies of the optic disc. Surv. Ophthamol. 1982;27(1):3-41. 2.Bateman BJ, Maumenee IH. Colobomatous macrophthalmia with microcornea. Ophthalmic Genetics. 1984;4(2):59-66. 3.Tron EZh. [Visual pathway disorders]. L.;1968. Chapter 13.4:313-322. In Russian. 4.Duke-Elder S. System of ophthalmology. Vol. 3, Pt. 2. London: Kimpton;1958. 503 p. 5.Baibarodov IaV, Rudnik AIu. [Minimally invasive removal of ILM in the treatment of optic disc pits]. [Modern treatment technologies for vitreoretinal pathology: the conference proceedings]. M.;2012:27-30. In Russian. 6.Akiba J, Kakehashi A et al. Vitreous finding in cases of optic nerve pits and serous macular detachment. Am. J. Ophthalmol. 1993; 116(1):38-41. 7.Toker E, Elcioglu N, Ozcan E, Yenice O, Ogut M. Colobomatous macrophthalmia with microcornea syndrome: Report of a new pedigree. American J. of Medical Genetics. 2003;121A (1):25-30. 8.Lincoff H, Schiff W, Krivy D, Ritch R. Optic coherence tomography of optic disc pit maculopathy. Am. J. Ophthalmol. 1996;122(2):264-6. 9.Gass JD. Serous detachment of the macula. Secondary to congenitial pit of the optic nervehead. Am. J. Ophthalmol. 1969;67(6):821-41. 10.Shamshinova AM. [Inherited and congenital diseases of the retina and optic nerve]. M.;2001:487-9. In Russian. 11.Gordon R, Chatfield RK. Pits in the optic disc associated with macular degeneration. Br. J. Ophthalmol. 1969;53(7):481-9. 12.Yanyali A, Bonnet M. Treatment of macular detachment complicating optic disc coloboma pits. Long-term results of the photocoagulation-gas combination. J. Fr. Ophtalmol. 1993;16(10):523-31. 13.Jia YP, Sun L, Yu HS, Liang LP, Li W, Ding H, Song XB, Zhang LJ. The Pharmacological Effects of Lutein and Zeaxanthin on Visual Disorders and Cognition Diseases. Molecules. 2017; 22(4): 610; 14.Konovalova N, Khramenko N, Guzun O. [Conservative treatment efficiency in patients with age-related degeneration of the macula]. Oftalmologiia. Vostochnaia Evropa. 2016;6(2):240-9. In Russian. 15.Weiser MJ, Butt CM, Mohajeri MH. Docosahexaenoic Acid and Cognition throughout the Lifespan. Nutrients. 2016;17; 8(2):99.
This paper has been supported by Bausch Health.
|