J.ophthalmol.(Ukraine).2019;2:67-69.
|
http://doi.org/10.31288/oftalmolzh201926769 Received: 27 February 2019; Published-online: 24 April 2019 Proliferative diabetic retinopathy in unsuspected diabetes mellitus: a case report O.V. Zborovska1, Dr. Sc. (Med.); T.S. Pilkevich1, Cand. Sc. (Med.); N.B. Kuryltsiv2, Cand. Sc. (Med.); N.A. Samoluk1, MD 1 State Institution The Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine; Odessa (Ukraine) 2 Danylo Halytsky Lviv National Medical University; Lviv (Ukraine) E-mail: nsamoluk82@gmail.com TO CITE THIS ARTICLE: Zborovska OV, Pilkevich TS, Kuryltsiv NB, Samoluk NA. Proliferative diabetic retinopathy in unsuspected diabetes mellitus: a case report. J.ophthalmol.(Ukraine).2019;2:67-9. http://doi.org/10.31288/oftalmolzh201926769 Introduction. According to World Health Organization, nowadays, the amount of diabetic patients has exceeded 1,000 million people, equaling 3% of the Earth population. Unsuspected diabetes mellitus is a disease in a latent form without acute symptomatology. Purpose. To determine the etiology of retinopathy in the patients applied to the Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine. Material and Methods. Seven patients underwent the treatment at Department for Inflammatory Eye Diseases in the Filatov Institute of Eye Diseases and Tissue Therapy. The patients complained of both distance and near visual loss. All patients were diagnosed proliferative DRP with neovascularization, hemorrhage, and exudates. Blood glucose tests were within normal ranges and did not exceed 5.8 mmol/l. In the course of the treatment, visual acuity improved by three lines, at an average. Conclusion. As a result of ophthalmic examination, ophthalmic diagnosis, and, afterwards, endocrinological examination, all patients were diagnosed diabetes mellitus in a latent form. Keywords: diabetes mellitus, unsuspected diabetes, latent diabetes, diabetic retinopathy
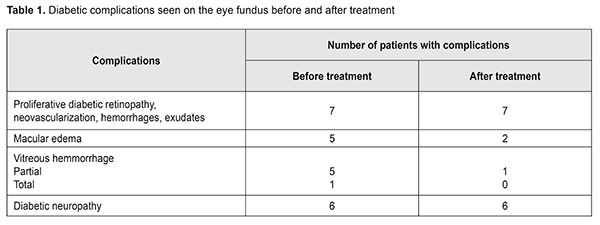
Introduction Diabetes mellitus (DM) and diabetic complications are one of the major medical and social problems today both in the developing and developed countries. According to World Health Organization, nowadays, the amount of diabetic patients has exceeded 1,000 million people, equaling 3% of the Earth population. The DM incidence increases by 5-7% every year and twice every 12-15 years. In Ukraine, this index equals 1 million people; however, the true DM rate is twice higher as it has been registered due to occurrence of a latent form of diabetes. Unsuspected diabetes mellitus is a disease in a latent form without acute symptomatology and with normal ranges of glycated hemoglobin and fasting plasma glucose [1, 2, 3, 4]. This pathology is more often diagnosed too late when the alterations in the body are irreversible [4, 5]. The danger of a latent disease lies in the fact that latent DM has no manifestations while the changes in the body are in process already. In unsuspected DM, the whole vascular system is damaged and there is an increased risk of a stroke and a heart attack [6, 1, 3]. The possibility of mortality due to a stroke and a heart attack is several times increased in people with unsuspected DM. Visual loss and neuropathy are also observed. Diabetic retinopathy (DRP) is one of the leading causes of vision-related disability among working age persons [7, 3]. Material and Methods Seven patients, 4 women and 3 men, aged 50-65 and 55-70, respectively, underwent the treatment at Department for Inflammatory Eye Diseases in the Filatov Institute of Eye Diseases and Tissue Therapy. The patients complained of both distance and near visual loss. All patients were performed the standard ophthalmological examination including visual acuity testing, intraocular pressure measurement, peripheral perimetry, and phosphene testing. Additionally, optic coherent tomography (OCT) and fluorescein angiography (FAG) of the retina were made. Results Ophthalmological examination showed visual acuity decreased in both eyes in all patients; in three patients, visual acuity was lower than 0.1. Fundus biomicroscopy and ophthalmoscopy showed that almost all patients had vitreous hemorrhage: partial vitreous hemorrhage in both eyes was in three patients; partial vitreous hemorrhage in one eye was in two patients; and one patient had total vitreous hemorrhage in one eye. Upon fundus examination, the patients were diagnosed proliferative DRP with neovascularization, hemorrhage, and exudates [6, 7]. Five of seven patients had macular edema in both eyes. Six of seven patients were diagnosed diabetic neuropathy (Table 1). At the same time, blood tests were within normal ranges and did not exceed 5.8 mmol/l. All patients complained of significant weight loss for last six months as well as of impaired extremity sensation; six of them had problems with teeth and gums.
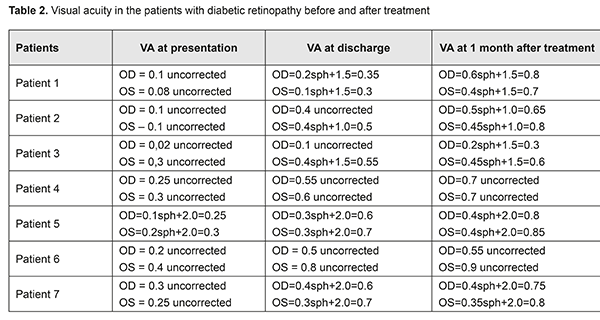
A clinical picture of the fundus corresponded to DRP, which was confirmed by the findings of FAG and OCT of the retina, peripheral perimetry, and phosphene tests. In this regard, the patients were referred to an endocrinologist. Endocrine examination included glycated hemoglobin and C-Peptide testing, exercise ECG testing, which made it possible to reveal a latent form of diabetes mellitus. After DM was confirmed, all patients were prescribed antihyperglycemic drugs and treated for DRP, conservatively and surgically. Conservative treatment included vasodilating, antioxidant, and nootropic drugs. Against the background of conservative treatment, the patients underwent panretinal laser retinal photocoagulation [8]. To resolve vitreous hemorrhage, an intravitreal injection of prourokinase was made. Five patients were performed intravitreal anti-VEGF injections. Changes in best corrected visual acuity (BCVA) after treatment are demonstrated in Table 2. Thus, BVCA increased after treatment in all patients. In the patient with the minimal BVCA value, BVCA increased from 0.02 at presentation to 0.1 at discharge and to 0.3 at 1 month after treatment. The patients with pre-treatment BVCA of 0.1-0.3, BVCA increased to 0.5-0.7 at discharge and to 0.6-08.8 at 1 month after treatment. Macular edema remained in two patients; partial vitreous hemorrhage was observed only in one patient.
Conclusion. Type 2 diabetes mellitus is often diagnosed by an ophthalmologist, which is more common for latent forms of diabetes. When retinopathy is revealed on the eye fundus, additional examination, including OCT and FAG of the retina, is required in order to determine the etiology of the disease. When diabetes mellitus is suspected, even if fasting plasma glucose and glycated hemoglobin are within the normal ranges, a patient must be referred to endocrinologist’s consultation with exercise ECG testing. When latent autoimmune diabetes in adults is confirmed, the patient must be treated by both an endocrinologist and an ophthalmologist. Our clinical findings showed that early diagnosis of retinopathy enabled to avoid developing fundus complications and to have a good response to treatment. References 1.Appel Sj, Wadas TM, Rosenthal RS, Ovalle F. Latent diabetes of adulthood: an often misdiagnosed type of diabetes mellitus. J Am Acad Nurse Pract. 2009;21:156-9. 2.Lutgens M, Meiger M, Peeters B et al. Easily obtainable clinical features increase the diagnostic accurancy for latent diabetes in adults: an evidance-based report. Prim care Diabetes. 2008; 2:207-11. 3.Naik RG, Brooks-Worrell BM, Palmer JP. Latent diabetes in adults. Clin Endocrinol Metab. 2009;94:4635-44. 4.Pipi E, Marketou M, Tsirogianni A. Distinct clinical and laboratory characteristics of latent diabetes in adults in relation to type 1 and type 2 diabetes mellitus. World J Diabetes. 2014;5:505-10. 5.Tuomi T, Groop LC, Zimmet PZ et al. Antibodies to glutamic acid decarboxylase reveal latent diabetes mellitus in adults with a non-insulin-dependent onset of disease. Diabetes. 1993;42:359-62. 6.Starkova N.T. [Clinical endocrinology. Guidance. 3rd Edition]. Saint Petersburg:Piter;2012. 576. Russian. 7.Kohner EM. Diabetic retinopathy. Brit. Med. Bull. 2004;5(1):148-73. 8.Pasyechnikova NV. [Laser treatment in pathology of the eye fundus]. K.: Naukova dumka; 2007. 206 p. Russian.
The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|