J.ophthalmol.(Ukraine).2019;1:29-32.
|
http://doi.org/10.31288/oftalmolzh201912932 Received: 19 October 2018; Published on-line: 28 February 2019 SD OCT retinal thickness in the macula area in premature children who received laser photocoagulation of avascular retina for severe ROP K.S. Zaichko, Post-graduate Student; S.V. Katsan, Cand Sc (Med); O.V. Ivanytska, Cand Sc (Med) Filatov Institute of Eye Disease and Tissue Therapy of NAMS of Ukraine Odessa (Ukraine) E-mail: k.s.zaichko@gmail.com TO CITE THIS ARTICLE: Zaichko KS, Katsan SV, Ivanytska OV.SD OCT retinal thickness in the macula area in premature children who received laser photocoagulation of avascular retina for severe ROP. J.ophthalmol.(Ukraine).2019;1:29-32.http://doi.org/10.31288/oftalmolzh201912932 Background: Immature ocular optics at birth and severe retinopathy of prematurity (ROP) may affect normal development of the retina and lead to late impairment of visual functions. Purpose: To compare spectral-domain optical coherence tomography (SD OCT) retinal thickness in the macular area between premature children who received laser photocoagulation of avascular retina (LPCAR) and full-term children aged 4-6 years. Materials and Methods: Twenty-five premature children (50 eyes) and 38 full-term control children (69 eyes without eye disease) aged 4-6 years received observation care at the Filatov institute between 2011 and 2017. The inclusion criterion for premature children was receiving LPCAR for severe (type 1 subthreshold, or threshold) ROP diagnosed during screening. Patients with grade 4 or 5 ROP or other ocular pathology (history of cataract, glaucoma, trauma or eye surgery) were excluded. Results: There was a significant difference in retinal thickness in the macular area between premature and full-term children; the magnitude of the difference depended on the severity of ROP. The foveal-to-central thickness ratio was found to be increased compared to controls by at least 0.1 in 18 premature children (36 eyes, 72%) who received LPCAR (p <0.05). Conclusion: Mean SD OCT retinal thicknesses in all macular sectors in premature children who received LPCAR for ROP were greater than in full-term children. Keywords: retinopathy of prematurity, retinal thickness, SD OCT, smooth foveal depression
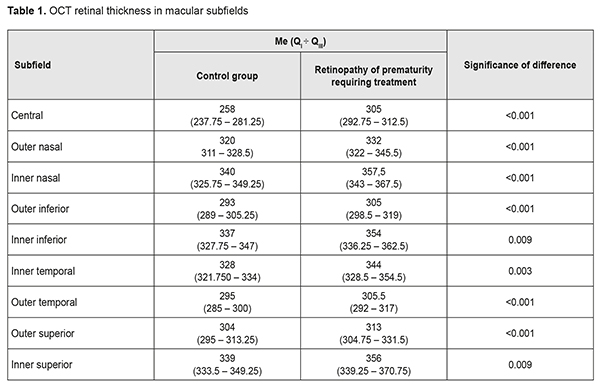
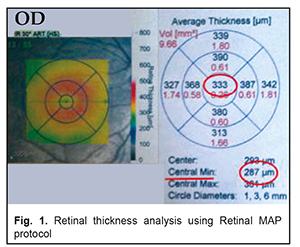
Introduction Preterm delivery may lead to neonatal complications including those related to the eye. Retinopathy of prematurity (ROP) is a severe vasoprolliferative retinal disorder that may cause blindness or visual impairment [1]. Immature ocular optics at birth and severe ROP may affect normal development of the retina, and lead to late impairment of visual functions [2]. Optical coherence tomography (OCT) is a commonly used objective non-contact imaging technology for examination of the retina. Of the methods used for diagnosis of retinal pathological conditions, it provides one of the greatest amounts of valuable information. In addition, it produces images approaching the resolution of histology [3]. The absence of tissue contact during OCT session and short-time scanning process make it possible to employ the method in children of 3 years and older [4]. The purpose of the study was to compare spectral-domain optical coherence tomography (SD OCT) retinal thicknesses in the macular area between preterm children who received laser photocoagulation of avascular retina for severe ROP and full-term children aged 4-6 years. Materials and Methods Twenty-five premature children (50 eyes) and 38 full-term children (69 eyes) aged 4-6 years received outpatient observation care at the Filatov institute between 2011 and 2017. The inclusion criterion for premature children was severe ROP (subthreshold ROP, type 1 or threshold ROP) diagnosed during screening. The children diagnosed with severe ROP underwent laser photocoagulation of avascular retina before the age of 3 months. Patients with grade 4 or 5 ROP or other ocular pathology (history of cataract, glaucoma, trauma or eye surgery) were excluded. Premature patients were compared with 38 conventionally healthy full-term age-matched controls (69 eyes). Inclusion criteria for full-term children were normal weight at birth and absence of ocular pathology. Mean gestation age at birth and mean weight at birth of the included premature children (15 boys and 10 girls) were 1407 ± 753 g and 30 ± 3.5 weeks, respectively. The Spectralis™ platform (Heidelberg Engineering GmbH, Heidelberg, Germany; imaging speed, 40,000 A-scans/s; optical resolution, 7.5 μm; axial digital resolution, 3.5 μm) was used for retinal SD OCT imaging. If the data followed normal distribution, ANOVA was used for statistical analyses (Scheffe test was used for paired comparisons). Otherwise, a Kruskal-Wallis test, followed by a Dunn’s test, was performed. Microsoft Excel was used for statistical analyses. Results Mean SD OCT retinal thicknesses in all macular quadrants in the group of patients who received laser treatment were significantly greater (p < 0.05) than in controls (Table 1). Therefore, there were statistically significant differences in retinal macular thickness between premature and full-term children (Fig. 1).
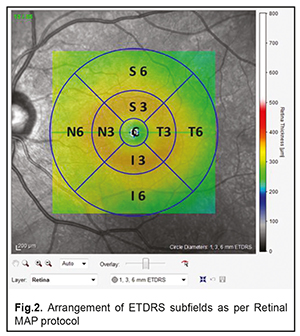
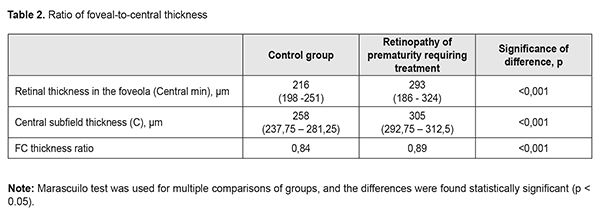
The ratio of foveal-to-central thickness (ratio of foveal thickness to central segment thickness, or FC thickness ratio) (Fig.2) [5] reflects the degree of differentiation and development of the macular region [6].
There were statistical significant differences in FC thickness ratio among premature and full-term children (Table 2). Of the 25 premature children (50 eyes), 18 (36 eyes; 72%) and 7 (14 eyes; 28%) had an increase in the FC thickness ratio of ≥ 0.1 and < 0.1, respectively, compared to controls.
Discussion Of the methods used for lifetime layer-by-layer examination of the chorioretinal complex, OCT provides the greatest amount of valuable information. SD OCT can detect retinal structural changes much earlier than the ophthalmoscopic signs can be detected or functional impairment can be detected with ophthalmoscopy or ultrasound scanning of the eye [7]. Macular morphological parameters of healthy full-term children should be used as normative values in the diagnosis of pediatric macular disorders. In the study by Samarawickrama et al [8], TD OCT-derived retinal thickness in the centre of the macula for children aged 6 years and 12 years was 192.5 μm and 197.5 μm, respectively. El-Dairi and co-authors [9] reported that mean foveal thickness for healthy full-term children aged 3 to 17 years (mean (SD) age, 8.59 (3.11) years) was 189 μm. In the study by Eriksson et al [3], mean central macular thickness for full-term children aged 5 to 16 years (mean age, 10.1 years) was 204 μm. Adem Turk and co-authors reported that central macular thickness for healthy children was 211.39 μm.. Since studies vary widely in their estimates of retinal thicknesseses in the macular area for healthy full-term children, we used our estimates of mean retinal thicknesses in the macular area for full-term children aged 4-6 years as the norm. Chen et al [7] found in the study of children aged 4-16 years that the full retinal thickness (μm) over the fovea was 284.7 ± 23.3 mm and 244.4 ± 17.0 in the group treated with laser photocoagulation for ROP and full-term group, respectively (p < .001). Stoica et al [10] reported that central fovea thickness was significantly higher in 3-8 year old children born preterm and with laser-treated ROP as compared to aged-matched controls (275 ± 34.8 μm versus 224 ± 27.2 μm; p < 0.001). A number of other studies [2, 4, 11] have also demonstrated that, compared to full-term children, retinal thickness at the macula was thickened in premature children. The current study found that laser-treated premature children showed significantly greater (p < 0.05) retinal thicknesses in all macular sectors compared to controls. Our analysis of retinal SD OCT images and SD OCT-derived retinal thicknesses in the macular region demonstrated that patients differed in foveal contour, with OCT showing a smooth foveal depression in some eyes. In the opinion of Anand and co-authors [12], the presence of a smooth foveal depression and the presence of maintained inner retinal layers (including inner plexiform and nuclear layers) in the foveal center are the signs of “inner retinal immaturity”. As preterm neonate studies have demonstrated that no foveal depression was seen in most extremely premature infants with zone I ROP, changes secondary to ROP in immature retina might be capable of arresting the development of the retina [2, 4, 6, 11]. Previously, Pasyechnikova et al [5] have proposed a FC thickness ratio as an early sign of macular edema in diabetic maculopathy, and we utilized this ratio for quantitative assessment of retinal changes in the current study. An increase in the FC ratio compared to controls indicates a change in the configuration of macular contour due to decreased foveal depression. Decreased foveal depression can be explained by the presence of not only the outer nuclear layer, but also deeper retinal layers in eyes of premature children, which might evidence the anatomical immaturity of the retina. Increased FC thickness ratio and statistically significantly increased SD OCT-derived retinal thicknesses in all macula quadrants were common in patients treated for severe ROP. This may reflect features of differentiation and development of the macular region in children differing in degree of manifestations of residual fundus changes due to history of the disease and possible influence of laser treatment. Therefore, preterm delivery, immature ocular optics at birth, and history of ROP may affect normal development of the retina and lead to late impairment of visual functions. It has been demonstrated that, when combined with adequate image processing, the capabilities of SD OCT provide a vast amount of valuable data regarding the retinal state in children and the features of retinal structure in premature children. This contributes to better understanding of the process of retinal development. The identification of retinal macular changes in children before the latter reach school age is important for early detection, treatment and prevention of visual dysfunction. Conclusion First, in 4-6 year old premature children who received laser photocoagulation of avascular retina for severe ROP, SD OCT-derived retinal thicknesses in all macula quadrants were statistically significantly greater than in age-matched full-term controls. Second, of the 25 premature children (50 eyes) who received laser photocoagulation of avascular retina for severe ROP, 18 (36 eyes; 72%) had an increase in the foveal-to-central thickness ratio of ≥ 0.1, compared to controls. References
1.Larsson E, Rydberg A, Holmstrom G. Contrast sensitivity in 10 year old preterm and full term children: a population based study. Br J Ophthalmol. 2006 Jan; 90(1): 87–90. 2.Wang J, Spencer R, Leffler JN, Birch EE. Critical period for foveal fine structure in children with regressed retinopathy of prematurity. Retina. 2012 Feb;32(2):330-9. 3.Eriksson U, Holmström G, Alm A, Larsson E. A population-based study of macular thickness in full-term children assessed with Stratus OCT: normative data and repeatability. Acta Ophthalmol. 2009 Nov;87(7):741-5. 4.Akerblom H, Larsson E, Eriksson U, Holmstrom G. Central macular thickness is correlated with gestational age at birth in prematurely born children. Br J Ophthalmol. 2011 Jun;95(6):799-803. 5.Pasyechnikova NV, Naumenko VA, Zborovska OV. [Foveal to central thickness ratio as an early sign of retinal macular edema]. Oftalmol Zh. 2004;5:4-6. Russian. 6.Ecsedy M, Szamosi A, Karkó C, et al. A comparison of macular structure imaged by optical coherence tomography in preterm and full-term children. Invest Ophthalmol Vis Sci. 2007 Nov;48(11):5207-11. 7.Chen YH, Lien R, Chiang MF, et al. Outer Retinal Structural Alternation and Segmentation Errors in Optical Coherence Tomography Imaging in Patients With a History of Retinopathy of Prematurity. Am J Ophthalmol. 2016 Jun;166:169-180. 8.Samarawickrama C, Wang JJ, Huynh SC, et al. Macular thickness, retinal thickness, and optic disk parameters in dominant compared with nondominant eyes. AAPOS. 2009 Apr;13(2):142-7. 9.El-Dairi MA, Asrani SG, Enyedi LB, Freedman SF. Optical coherence tomography in the eyes of normal children. Arch Ophthalmol. 2009 Jan;127(1):50-8. 10.Stoica F, Chirita-Ermandi A, Andreescu N, Stanciu A, Zimbru CG, Puiu M. Clinical relevance of retinal structure in children with laser-treated retinopathy of prematurity versus controls – using optical coherence tomography. Acta Ophthalmol. 2018 Mar;96(2):e222-e228. Epub 2017 Sep 19. 11.Yanni SE, Wang J, Chan M, et al. Foveal avascular zone and foveal pit formation after preterm birth. Br J Ophthalmol. 2012 Jul;96(7):961-6. 12.Yuodelis C, Hendrickson A. A qualitative and quantitative analysis of the human fovea during development. Vision Res. 1986;26(6):847-55.
|