J.ophthalmol.(Ukraine).2019;1:23-28.
|
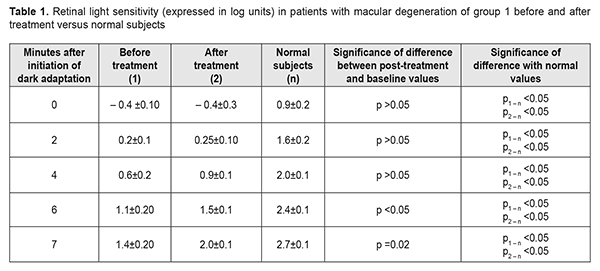
http://doi.org/10.31288/oftalmolzh201912328 Received: 14 November 2018; Published on-line: 28 February 2019 On the treatment of degeneration of the macula and posterior pole N.V. Konovalova, Dr Sc (Med); N.I. Khramenko, Cand Sc (Med); O.V. Guzun, Cand Sc (Med); T.M. Serebrina, Cand Sc (Med) Filatov Institute of Eye Disease and Tissue Therapy of NAMS of Ukraine Odessa (Ukraine) E-mail: kvnkonovalova@gmail.com TO CITE THIS ARTICLE: Konovalova NV, Khramenko NI, Guzun OV, Serebrina TM.On the treatment of degeneration of the macula and posterior pole. J.ophthalmol.(Ukraine).2019;1:23-8.http://doi.org/10.31288/oftalmolzh201912328 Background: The field of degeneration of the macula and posterior pole (DMPP) is of outstanding medical and social significance as the disease is of high prevalence and leads to loss of general working capacity. Purpose: To determine the efficacy of conservative treatment with endonasal iontophoresis of Omk2, and the degree of stabilization of visual functions after this treatment in patients with DMPP. Materials and Methods: Thirty-two patients (45 eyes; age, 51 to 75 years) with DMPP were examined and received treatment with endonasal iontophoresis of Omk2. The eye examination included visual acuity, retinal light sensitivity, threshold assessment with macula tester, perimetry and ophthalmoscopy, and was performed before and after treatment. Results: In all patients with DMPP, iontophoresis of Omk2 contributed to apparent improvement in functional activity of the retina, which was achieved due to antioxidative, neurotropic, anti-edema and anti-angiogenetic properties of the drug. In particular, mean uncorrected visual acuity (UCVA) in patients of group 1 improved by 25%, from 0.6 to 0.85, and UCVA in 49% of patients of group 2 improved by 0.01-0.02, which improved the level of social rehabilitation of these patients. In patients with DMPP, the treatment with iontophoresis of Omk2 resulted in improvements in the functional activity of the retinal photopic system and foveal afferent system (as assessed by the Haidinger’s brushes test), and retinal blood flow in the posterior pole (as assessed by the blue field technique) by 33-43%, 14%, and 40%, respectively. This demonstrates that the treatment strategy has the beneficial impact on the function of the visual system, and iontophoresis of Omk2 is a pathogenetically reasonable approach to the management of DMPP. Conclusion: Iontophoresis of Omk2 was found to be beneficial for the function of the visual system, and a pathogenetically reasonable approach to the management of DMPP. Keywords: degeneration of the macula and posterior pole, iontophoresis of Omk2 Introduction Degeneration of the macula and posterior pole (DMPP), a retinal disease characterized by progressive and irreversible damage to the central light-sensitive area of retina (fovea centralis), is a leading cause of blindness in developed countries. Visual impairment is a global epidemic. In addition, age-related macular degeneration (AMD) and cataracts are the leading causes of blindness in developed nations. The World Health Organization has instituted VISION 2020: "The Right to Sight" as a global mission to put an end to worldwide blindness [1, 2]. In recent years, there has been a trend towards rejuvenation of the disease, which is associated with environmental factors and increased burden on the eye induced by stress and evolving use of computers. The field of DMPP is of outstanding medical and social significance as the disease leads to rapid loss of central vision and loss of general working capacity. As we age, the Bruch’s membrane thickens, and its permeability to serum proteins decreases, with a decrease in choriocapillaris network density. Some macular changes are related to normal aging, and excessive buildup of lipofuscin (aging) pigment in the retinal pigment epithelium precedes the degeneration. Age Related Eye Disease Study 2 (AREDS2) has found that, controlling for baseline AMD status, none of the treatments were shown to significantly reduce risk of AMD progression relative to the group who received the “placebo” AREDS1 supplement (the combination of nutrients and vitamins proposed by the NIH) only [1-3]. Cardiovascular diseases play a role in the development of AMD. The risk of DMPP increases 3-fold in the presence of atherosclerosis, and 7-fold in the presence of hypertonic disease. In addition, most AMD patients have been found to exhibit decreased regional blood supply [3-5], which correlated with decreased choroidal thickness. Early and adequate treatment may stabilize visual functions and prevent the development of blindness in these patients. For decades, ophthalmologists have been searching for the methods to treat and prevent degeneration in the retinal tissue. Management of AMD is still a challenge for clinicians, and the development of advanced treatment approaches is of utmost importance. One may prevent the disease, accelerate rehabilitation and prevent irreversible retinal changes through the use of agents that reduce damaging factors (e.g., anti-hypoxia agents). Our attention was drawn to OMK2 agent that prevents apoptosis and generation of residual free-radicals, and promotes phospholipid synthesis in in neuronal membranes (which improves membrane function, including the function of ion exchange pumps and neuronal receptors). The drug contains citicoline, vitamin B12, and hyaluronic acid (a mucopolysaccharide that is a component of human ocular connective, nerve and epithelial tissues and the vitreous). Citicoline is a mononucleotide composed of ribose, cytosine, pyrophosphate, and choline whose chemical structure corresponds to 2-oxy-4-aminopyrimidine. It is a natural precursor of phosphatidylcholine (PDC), the main component of neuronal and mitochondrial membranes [6]. Citicoline, being an endogenous nucleotide, is available naturally, and activates biosynthesis of structural phospholipids of neuronal membranes, which improves membrane function (including the function of ion exchange pumps and neuronal receptors). In addition, it has anti-edema properties and inhibits phospholipase activity, reduces free radical release, and maintains antioxidant defense. Moreover, citicoline prevents cell death as it has been shown to be able to inhibit apoptotic mechanisms and enhance cholinergic transmission [7, 8]. Citicoline has been used as a topically administered neuroprotective drug. There have been very few reports on the use of citicoline in the medical treatment of glaucoma, as a complement to hypotensive therapy [6, 9], which resulted in improvements in visual fields and electrophysiologic indices of retinal function, although the effect was short term (approximately 30 days after washing off the medication). We aimed to maximize the therapeutic effect by forming a drug depot in ocular tissues, and to prolong the effect by using a new route (non-topical and non-injection) for delivery. Ocular iontophoresis with transdermal or transmucosal delivery seemed appropriate for this purpose. This approach provides direct delivery to the focus of disease, with a prolonged therapeutic effect achieved in 10-15 minutes, and with no side effects. Vitamin B12 (cyanocobalamin) is a biologically active substance that (1) activates the metabolism of carbohydrates, proteins, and lipids, (2) is involved in the formation of nucleic acids, methionine, choline, and creatine, (3) contributes to normal DNA methylation and (4) is a co-factor of DNA synthesis. In addition, it reduces blood cholesterol levels and improves the tissue’s capacity for regeneration. Given the above, the purpose of the study was to determine the efficacy of conservative treatment with endonasal iontophoresis of Omk2 for stabilization of visual functions in patients with DMPP. Materials and Methods Thirty-two patients (45 eyes; age, 51 to 75 years) with DMPP were examined and received inpatient treatment at the Department of Inflammatory Eye Disease. They were divided into two groups based on entry-level visual acuity: group 1 of 22 individuals (30 eyes) with a relatively high visual acuity of 0.5 to 1.0, and group 2 of 10 individuals (15 eyes) with a low visual acuity (≤ 0.3). All patients received a course of treatment with endonasal iontophoresis of Omk2 (Farmigea S.p.A., Pisa, Italy). The eye examination included visual acuity, retinal light sensitivity (RLS), threshold assessment with macula tester, perimetry and ophthalmoscopy, and was performed before and after treatment. A semi-automatic adaptometer was used to determine RLS during 10 minutes: after 3 minutes of light adaptation at 1200 cd/m2, the subject was seated in the dark. The dark adaptation period of 7 minutes was characterized by the test object luminance being increased from 2х10–8 cd/m2 to 7.0 cd/m2, with patient’s RLS determined at baseline and at 2-, 4-, 6-, and 7-min time points. Haidinger’s brushes perception was assessed in patients with the use of macula tester (type MTP-1, Tochmedpribor, Kharkiv, Ukraine). Patients were asked to report if they saw Haidinger's brushes using the macula tester under standard illuminance conditions (55-65 lux). The ability to see Haidinger's brushes using the macula tester and to identify their colors and sense of rotation was considered evidence of normal foveal function. Our modification of the method consists in determining the individual’s threshold for perceiving Haidinger's brushes (TPHB) by changing the illuminance of the eyepiece with gentle rotation of the knob. The TPHB is the minimum field illuminance at which the patient can see Haidinger's brushes (Certificate of Efficiency Suggestion No.711 dated 10.07.96, from V.S. Ponomarchuk and N.I. Khramenko). The blue field technique (related to Scheerer's phenomenon) was used to assess ocular hemodynamics. The blue field entoptic phenomenon or Scheerer's phenomenon is the perception of entoptic images (tiny whitish dots) observed against a bright blue illumination and is caused by the movement of leukocytes in the perifoveal capillaries [10]. Routine iontophoretic techniques were used. Transorbital iontophoreric procedure Two to three ml of 2% CaCl2 solution and 1 ml of Omk2 are pipetted onto the bottom of a funnel-shaped active electrode (anode). The current is increased in a stepwise manner to 0.3 mA, 0.5 mA, 0.8 mА and 1 mА at 3 min, 5 min, 8 min and 10 min, respectively. The dispersive electrode is supplied with a hydrophilic spacer and placed at the shoulder and neck region. Endodasal iontophoretic procedure The nasal cavity is packed with a gauze piece soaked in 2-3 ml of calcium chloride 2% and 1 ml of Omk2 and used as the active electrode. The current is increased in a stepwise manner to 0.3 mA, 0.5 mA, 0.8 mА and 1 mА at 3 min, 5 min, 8 min and 10 min, respectively. Data were tested for normal before further statistical analysis. When two groups were compared, significance was tested either with Student’s test (in case of normal distribution), or with Mann-Whitney test (in case of non-normal distribution). Results and Discussion Mean uncorrected visual acuity (UCVA) and mean best-corrected visual acuity (BCVA; correction for hypermetropia or mild myopia) in dry AMD patients of group 1 were 0.60±0.09 and 0.80±0.07, respectively, at baseline, and improved to 0.85±0.07 (p < 0.05) and 0.90±0.09 (the improvement was statistically non significant), respectively, after treatment. Photopic light sensitivity in patients of group 1 was assessed through the determination of light sensitivity thresholds. Low-threshold photic stimulation (or the absolute light threshold) is the weakest photic stimulation that causes light perception. The reciprocal of the absolute light threshold characterizes the light sensitivity. Before treatment, mean light sensitivity patients of group 1 was 3 to 4 times lower than the norm (Table 1), and varied widely during the dark adaptation period, from 137% at the beginning to 78% at the end of the period. The variability indicates a substantial lack of balance in the photopic afferent system. After treatment with a course of Omk2 iontophoresis, mean light sensitivity in patients of group 1 improved insignificantly during the first minutes, and significantly (p < 0.05), by 36.3% and 42.9% (to 2.0±0.1 log units), at minute 6 and 7, respectively, of the dark adaptation period. The course of treatment contributed to stabilization of the photopic afferent system, with a decrease in the variability in characteristics to 27.5%. It is noteworthy that, in spite of a substantial improvement in light sensitivity in these patients, their light sensitivity values were 111% and 26% lower than the norm (2.7±0.1 log units) at the first minutes, and at minute 7, respectively, of the dark adaptation period (Table 1).
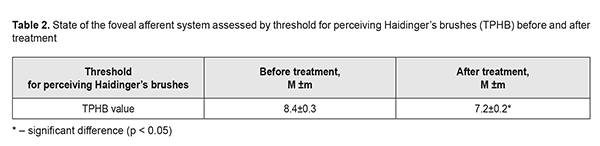
Light perception develops initially in the photosensory retina. Visual pigment molecules in the outer segments of photoreceptors decompose after absorbing light quanta, thus enabling a sequence of photochemical, electrical, ionic and enzymatic processes. Light sensitivity is the function of the visual system which is the most sensitive to changes in retinal blood supply, and thus is the first function to suffer from retinal architectural alterations, ischemia and decreased retinal metabolism. The determination of Haidinger’s phenomenon based on polarization features of the macula lutea is widely used by clinicians to diagnose an injury of the foveal afferent system. The capacity of the human eye to perceive the polarization of light as an entoptic visual phenomenon was described by Wilhelm Karl von Haidinger in 1844; this phenomenon is a consequence of the dichroism of the retinal layers in the macular lutea. Linearly polarised light induces the perception of a brushes-shaped yellowish structure against a whitish background. The phenomenon vanishes after a few seconds of observation. The axis of the brushes is perpendicular to the direction of polarization. The contrast of Haidinger brushes increases when the field is illuminated with blue light. Helmholtz hypothesized that the phenomenon is a consequence of the dichroism of radial fibers located close to the macula lutea and colored with the yellow pigment, lutein. It is currently believed that the dichroism results from the highly regular, but not chaotic arrangement of anisotropic molecules of carotenoids, lutein, zeaxanthin and meso-zeaxanthin. If these molecules are arranged perpendicularly to the fibers radiating from the fovea, they exert a filtering action on portions of polarized light, and, with blue light illumination, the eye sees two dark sectors, Haidinger's brushes, in the central portion of the visual field. The maximum of the rerinal dichroism has been found at 460 nm. It is much polarized light around us, and the ability to perceive it contributes to reflection of a multidimensional world by a two-dimensional retina [11]. Disruption of retinal structure in the macula lutea results not only in disarrangement of carotenoid molecules, but in metabolic shifts, lipid peroxidation alterations, and oxidative stress, with a loss of the ability to see Haidinger's brushes. Metabolic alterations in the RPE and choroid result in retardation of retinal processes, with increased time and illuminance required for Haidinger’s brushes perception. In group 1, all patients were found to see Haidinger’s brushes, and, therefore, individual’s TPHB was determined by changing the illuminance of the field. In these patients, mean TPHB was 8.4±0.3 units, which was 29% higher than the norm (6.5±0.2 units; p < 0.05). We found an improvement in the state of the foveal afferent system, with a 14.2% decrease in TPHB (p < 0.05), after the treatment course, although the mean TPHB did not achieve the normal level (Table 2), and was 10.7% higher than the norm.
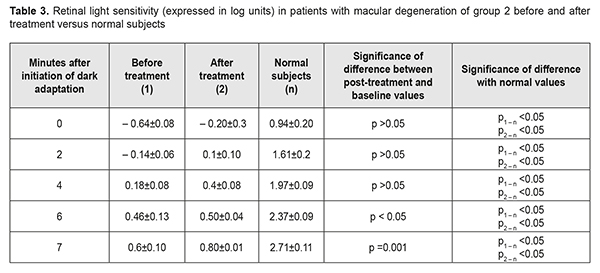
The blue field entoptic phenomenon or Scheerer's phenomenon was described by the German ophthalmologist Richard Scheerer in 1924. It is characterized by tiny bright dots moving quickly and semi-randomly across the visual field, especially when viewed against a background of bright blue light. Scheerer's phenomenon test is subjective, but can provide information on the blood supply to the posterior eye. The patient reports the number of whitish flickering corpuscles. Since, unlike red blood cells, white blood cells (WBC) do not absorb blue light, they are perceived as whitish corpuscles in the columns of blood contained within retinal blood vessels. In addition, unlike dissociated collagen fibers in the vitreous, they are of the same size and shape (round), in constant motion, and move along trajectories that do not depend on eye movements. In a normal subject, 50 or more moving whitish flickering corpuscles are seen. In group 1, the mean number of seen whitish flickering corpuscles was 25.0±0.1 before treatment (which was 50% lower than the norm), and increased by 40% to 35.5±0.2 after treatment, thus indicating increased retinal blood flow. Mean UCVA and mean BCVA (correction for hypermetropia or mild myopia) in dry AMD patients of group 2 were 0.1±0.02 and 0.19±0.06, respectively, at baseline, and did not change after treatment. However, 49% of patients exhibited improvement in visual acuity by 0.01-0.02. Before treatment, mean light sensitivity in patients of group 2 also varied widely within the dark adaptation period, from 146% at the beginning to 65% at the end of the period, and, at minute 7, was 0.6±0.10 log units, which was 4.5 times lower than the norm. After treatment with a course of Omk2 iontophoresis, mean light sensitivity in patients of group 2 improved significantly (p < 0.05), by 33% (to 0.80±0.01 log units; Table 3), at minute 7 of the dark adaptation period, but this was still 33.7% lower than the norm (p < 0.05).
Haidinger’s brushes were not recognized in AMD patients of group 2, which confirmed the presence of severe retinal changes at the fovea in the eyes of these patients. No substantial changes in the function of the foveal afferent system were found in these patients after treatment. Regarding the Scheerer's phenomenon, the mean number of WBC seen by patients of group 2 was 4.7 ±1.1 (i.e., 10 times lower than the norm) before treatment, and increased to 13.5±3.2 (p < 0.05) after treatment. This indicates that even after treatment, the retinal blood flow in these patients was still significantly decreased. Therefore, in AMD, functions of foveal and photopic afferent systems undergo a substantial change, with the degree of change depending on the severity of both damage to retinal structure and alterations in retinal blood supply. The physical effect of iontophoresis in combination with the effect of pharmaceuticals containing vitamins, citicoline, and hyaluronic acid, exerted metabolic and antioxidant actions, improved blood rheology, thus enhancing visual functions through an influence not only on the internal retinal layers and optic nerve axons, but also on retinal photoreceptors (i.e., the first visual pathway neuron). Until today, there have been no neuroprotectors among eye drops, since their molecules are large and lipophilic, and thus do not readily penetrate the ocular tissues [9, 12]. The experimental study [12] has demonstrated that the ophthalmic solution OMK1 based on citicoline 2% in combination with high molecular weight hyaluronic acid and benzalkonium chloride at low concentration, 0.01%, guarantees the passage of the molecule in the posterior segment, reaching the retina and the optic nerve head. Once in the anterior chamber, the molecule diffuses in the vitreous through the zonula and through the uveoscleral route. Hyaluronic acid facilitates the process [12]. We believe that Omk2 iontophoresis enhances the penetration of the drug into the ocular tissues, with the molecule more readily diffusing in the vitreous and reaching the retina. In the current study, iontophoresis with the combination drug composed of citicoline 2%, hyaluronic acid and vitamin B12, demonstrated improved foveal afferent function which was assessed through Haidinger’s brushes, a phenomenon that is associated with the dichroism [11], the levels and arrangement of lutein and meso-zeaxanthin in the retina. The improvement and stabilization of visual acuity were attributed to a treatment-induced improvement in the function of the visual system. In AMD, functions of foveal and photopic afferent systems undergo a substantial change, with the degree of change depending on the severity of both damage to retinal structure and alterations in retinal blood supply. It is noteworthy that Omk2 iontophoresis contributed to apparent improvement in functional activity of the retina in all patients with dry AMD, with a 25% improvement (from 0.6 to 0.85) in UCVA in patients of group 1. In 49% of patients of group 2, UCVA improved insubstantially, by 0.01 to 0.02, which nevertheless improved the level of social rehabilitation of these patients. In addition, the combination drug composed of citicoline 2%, hyaluronic acid and vitamin B12, was noted to improve retinal blood flow (which was assessed by the blue field technique) in all patients of the study. This might extend the list of indications for the drug, but the subject warrants further research. The AMD treatment and prevention strategy involving iontophoresis with citicoline is based on the following fact: antioxidant, neuroprotective, anti-edema and anti-angiogenesis processes play the major role in the targeted medicamentous influence on the retina and choroid [4]. Therefore, introducing the drug with antioxidative and neuroprotective effect into the management of DMPP is a pathogenetically targeted and reasonable approach [7, 8]. Conclusion Iontophoresis with Omk2 was found to be beneficial for the function of the visual system, and is a pathogenetically reasonable approach to the management of DMPP. In addition, in patients with DMPP, the treatment with iontophoresis with Omk2 resulted in improvements in the functional activity of the retinal photopic system and foveal afferent system (assessed by the Haidinger’s brushes test), and retinal blood flow in the posterior pole (assessed by the blue field technique) by 33-43%, 14%, and 40%, respectively. References 1.Karuppagounder SS, Pinto JT, Xu H, Chen HL, Beal MF, Gibson GE. Dietary supplementation with resveratrol reduces plaque pathology in a transgenic model of Alzheimer's disease. Neurochem Int. 2009 Feb;54(2):111-8. 2.Weiser MJ, Butt СM, Mohajeri МН. Docosahexaenoic Acid and Cognition throughout the Lifespan. Nutrients. 2016 Feb;8(2): 99. 3.Duffy SJ, Vita JA. Effects of phenolics on vascular endothelial function. Curr Opin Lipidol. 2003 Feb;14(1):21-7. 4.Korol AR, Khramenko NI, Zadorozhnyy OS, Kustryn TB. [Interrelationship of choroidal morphometric characteristics and ocular blood volume in patients with age-related macular degeneration]. Ophthalmol Zh. 2013;(3):23-7. Russian. 5.McCusker MM, Durrani K, Payette MJ, Suchecki J. An eye on nutrition: The role of vitamins, essential fatty acids, and antioxidants in age-related macular degeneration, dry eye syndrome, and cataract. Clin Dermatol. 2016 Mar-Apr;34(2):276-85. 6.Parisi V, Centofanti M, Ziccardi L, Tanga L, Michelessi M, Roberti G, Manni G. Treatment with citicoline eye drops enhances retinal function and neural conduction along the visual pathways in open angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 2015 Aug;253(8):1327-40. 7.Kliushnikov SA. [Neuroprotective and neuroreparative effects of Ceraxon (Citicoline): A review of experimental and clinical studies]. Nervnyie bolezni. 2012; (3):14-8. Russian. 8.Sekades JJ. Citicoline: pharmacological and clinical review. Rev Neurol. 2016 Dec 23;63(S03):S1-S73. 9.A preliminary study of the neuroprotective role of citicoline eye drops in glaucomatous optic neuropathy. Indian J Ophthalmol. 2014 May;62(5):549-53. 10.Scheerer R. Die entoptische Sichtbarkeit der Blutbewegungen im Auge und ihre klinische Bedeutung. Klinisches Monatsblatt Augenheilkunde. 1924;73:67-107. 11.Horváth G, Varju D. Polarized light in animal vision: polarization patterns in nature. Springer; Berlin; New York: 2004. 12.Ashton P, Podder SK, Lee VH. Formulation influence on conjunctival penetration of four beta blockers in the pigmented rabbit: A comparison with corneal penetration. Pharm Res. 1991 Sep;8(9):1166-74.
|