J.ophthalmol.(Ukraine).2018;6:3-9.
|
http://doi.org/10.31288/oftalmolzh2018639 Received: 21 September 2018; Published on-line: 30 December 2018 Ocular surface changes in mild and moderate myopes differing in duration of soft contact lens wear T.A. Veliksar; T.B. Gaidamaka, Dr Sc (Med); G.I. Drozhzhina, Dr Sc (Med), Prof. Received: 21 September 2018 Published: 30 December 2018 Filatov Institute of Eye Diseases and Tissue Therapy, NAMS of Ukraine Odessa (Ukraine) E-mail: tveliksar@gmail.com TO CITE THIS ARTICLE: VeliksarTA, GaidamakaTB, DrozhzhinaGI. Ocular surface changes in mild and moderate myopes differing in duration of soft contact lens wear. J.ophthalmol.(Ukraine).2018;6:3-9. http://doi.org/10.31288/oftalmolzh2018639
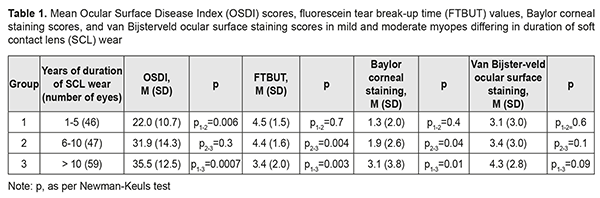
Background: Contact lenses (CL) are widely prescribed for various indications. A rather high incidence of severe complications in CL wearers necessitates a deeper and more detailed investigation of CL-associated ocular surface changes with duration of soft contact lens (SCL) wear. Purpose: To investigate ocular surface changes in mild and moderate myopes differing in duration of SCL wear. Materials and Methods: Seventy-nine mild and moderate myopes (152 eyes; mean age, 30.8±0.4 years; mean duration of lens wear, 10.2±0.6 years) wearing silicone hydrogel contact lenses were involved in the study. Patients were divided into groups based on duration of SCL wear (1-5 years, 6-10 years, and > 10 years). They completed an Ocular Surface Disease Index (OSDI) questionnaire and underwent visual acuity assessment, anterior biomicroscopy and the following tests: ocular surface fluorescein staining, lid-parallel conjunctival folds (LIPCOF), lid-wiper epitheliopathy (LWE), fluorescein tear break-up time (FTBUT), Schirmer I and Schirmer II tests, and corneal sensation by the method of Faulkner using a cotton swab applicator. The van Bijsterveld system and the Baylor scale were used to quantify ocular surface staining and corneal staining, respectively. Results: In mild and moderate myopes wearing soft contact lenses, overall OSDI score, LIPCOF score, LWE score, FTBUT, Baylor corneal staining score, van Bijsterveld ocular surface fluorescein staining score, corneal sensation loss, presence of corneal epithelial edema, presence of corneal fluorescein staining, conjunctival hyperemia, presence and degree of limbal vascularization, presence and degree of corneal vascularization, and presence of corneal opacity were found to statistically significantly depend on duration of SCL wear. Conclusion: An OSDI test found mild ocular surface disease in myopic patients wearing lenses for ≤ 5 years, and moderate ocular surface disease, in those wearing lenses for > 5 years. There was a high probability of a severe corneal sensation loss (80%) for overall OSDI score ≥32.5 (i.e., moderate ocular surface disease). The most apparent changes in the ocular surface developed in patients wearing SCL for > 10 years. Decreased tear production and quality, lid-wiper epitheliopathy as shown by fluorescein staining, conjunctival folds (LIPCOF test), conjunctival hyperemia, corneal opacities, limbal and corneal vascularization were observed in patients wearing SCL for at least a year. Corneal edema and presence of corneal and conjunctival fluorescein staining were found in patients wearing SCL for at least 6 years. Loss of central corneal sensitivity was noted in patients wearing SCL for > 10 years. Keywords: cornea, soft contact lenses, duration of lens wear, myopia Introduction Contact lenses (CL) are widely prescribed in patients with aphakia, keratoconus, high anisometropia, for the treatment of various ocular surface diseases [1-8], after refractive surgical procedures [5, 9-12], in eyes with persistent epithelial defects [3, 13-14], and as an alternative to spectacle correction. In addition, cosmetic contact lenses are increasingly popular [15]. The ocular surface is a very important part of the eye. It consists of the conjunctiva, limbus, cornea, tear film, lacrimal glands, nasolacrimal drainage apparatus and associated eyelid structures. Long-term contact lens wear affects the ocular surface resulting in complications like contact lens discomfort (CLD), dry eye syndrome, corneal vascularization, mechanical microtrauma, corneal erosion, keratitis, infiltrates, corneal ulceration, and/or allergic reactions. The prevalence of CLD among CL wearers varies from 23% to 94% [16-20]. Contact lens wearers make up 10 to 30% of patients diagnosed with corneal vascularization [21, 22], and corneal vascularization develops in 1 to 20% of contact lens wearers [23]. Patients who use rigid gas permeable lenses have a lower rate of vascularization [24]. A higher prevalence has been reported in relation to soft contact lenses (SCL), especially in long-term wearers [21, 24]. Microbial keratitis (MK) is the most serious vision-threatening complication associated with incorrect use of the contact lenses. Risk factors for MK include dryness, corneal hypoxia, edema, or erosion, contact lens deposits, allergic reactions, microbial contamination of lens care solutions and their accessories, and improper hygiene practices [25-28]. The risk may increase as much as 20-fold with extended contact lens wear, leading to increased corneal hypoxia [29]. Mechanical microtrauma to the corneal epithelium, represented by punctuate epithelial erosions, has been associated with silicone hydrogel contact lenses despite their higher oxygen permeability. The broken epithelial barrier can be a serious risk factor for developing infectious keratitis [29-31]. The approximate yearly incidence of microbial keratitis ranges from 1.2 to 25.4% per 10,000 contact lens wearers depending on the type of lens and wearing program [20,32-34]. Approximately 85% of cases of Acanthamoeba keratitis are related to contact lenses [4]. Contact lens wear is a major risk factor for developing fungal keratitis, particularly those caused by yeast-like fungi, as demonstrated in 78 eyes of fungal keratitis collected from 1999 to 2008 [35]. Moreover, long-term CL wear increases this risk [36]. The incidence of contact lens-induced peripheral ulcer (CLPU) for daily wear silicone hydrogel lenses has been reported to be 2–3%, increasing to 2–6% with extended wear schedules [37, 38]. The incidence rate of contact lens-induced papillary conjunctivitis (CLPC) ranges from 1.5% [39] to 47.5% [40]. The prevalence of CLPC is higher in patients using silicone hydrogel lenses compared with those wearing hydrogel lenses [41], which is likely due to greater mechanical irritation caused by these lenses [42]. Changing the lens type to daily disposable has been associated with decreased prevalence of allergic reactions [43]. A rather high incidence of severe complications in contact lens wearers necessitates a deeper and more detailed investigation of CL-associated ocular surface changes in patients differing in duration of SCL wear. The purpose of the study was to investigate ocular surface changes in mild and moderate myopes differing in duration of SCL wear. Material and Methods This study was conducted at the Corneal Microsurgery Department of the Filatov Institute of Eye Diseases and Tissue Therapy. Seventy-nine mild and moderate myopes (152 eyes; 61 women (77.2%) and 18 men (22.8%); mean age, 30.8±0.4 years; duration of lens wear, 1 year to 41 year; mean duration of lens wear, 10.2±0.6 years) wearing silicone hydrogel contact lenses were involved in the study. The mean refraction, mean uncorrected visual acuity (UCVA) and mean best-corrected visual acuity (BCVA) were -4.12±0.11 D, 0.12±0.01, and 0.86±0.02, respectively. Patients were divided into groups based on duration of SCL wear (1-5 years, 6-10 years, and > 10 years). They completed an Ocular Surface Disease Index (OSDI) questionnaire and underwent visual acuity assessment using the Shevaliov chart, anterior biomicroscopy, and the following tests: ocular surface fluorescein staining, lid-parallel conjunctival folds (LIPCOF), lid-wiper epitheliopathy (LWE), fluorescein tear break-up time (FTBUT), and lid-parallel conjunctival folds (LIPCOF). Corneal staining was quantified using Baylor scoring (with a 0-to-15 scale), and ocular surface staining, using van Bijsterveld scoring (with a 0-to-9 scale). Total tear production was assessed with Schirmer I test, and basal tear secretion, with Schirmer II test or Schirmer-Jones test. A cotton swab applicator was used to assess corneal sensation by the method of Faulkner. Statistical analyses were conducted using Statistica 10.0 (StatSoft, Tulsa, OK, USA) software. Data are presented as mean (with standard deviation (SD) in parentheses). Results Mean overall OSDI scores were 22.0 (10.7) for 1-5 years, 31.9 (14.3) for 6-10 years, and 35.5 (12.5) for > 10 years duration of SCL wear (Table 1), corresponding to mild ocular surface disease (OSD), moderate OSD, and moderate OSD, respectively. The difference in overall OSDI scores between patients with 1-5 years, and those with > 10 years duration of SCL wear was statistically significant (р=0.006, Fig. 1, Table 1).
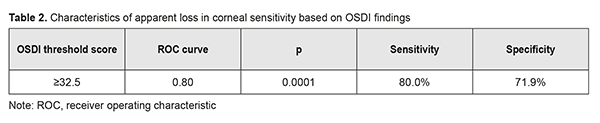
We found that OSDI scores were directly correlated with combined LIPCOF scores, LWE scores, degree of loss of central corneal sensation, presence of conjunctival hyperemia, presence of limbal vascularization and degree of limbal vascularization. The greatest correlation coefficient was with the degree of loss of central corneal sensation. The mean overall OSDI score 41.8 (11.8) for severe corneal sensation loss was statistically significant. It was demonstrated that there was a high probability of a severe corneal sensation loss (80%) for overall OSDI score ≥32.5 (Table 2 and Fig. 2).
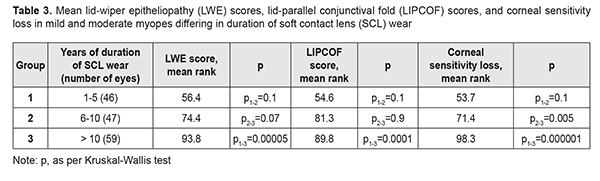
Mean FTBUT values were 4.5 (1.5) s for 1-5 years, 4.4 (1.6) s for 6-10 years, and 3.4 (2.0) s for > 10 years duration of SCL wear (Table 1). Mean Baylor corneal staining scores were 1.3 (2.0) for 1-5 years, 1.9 (2.6) for 6-10 years, and 3.1 (3.8) for > 10 years duration of SCL wear. The Baylor corneal staining score for > 10 years duration of SCL wear was statistically significantly greater than those for 1-5 years and 6-10 years (Table 2). Baylor corneal fluorescein staining was positive for ≥ 3 years (mean value, 11.1 (6.8) years) duration of SCL wear. Mean van Bijsterveld ocular surface fluorescein staining scores were 3.1 (3.0) for 1-5 years, 3.4 (3.0) for 6-10 years, and 4.3 (2.8) for > 10 years duration of SCL wear. The van Bijsterveld ocular surface fluorescein staining score for > 10 years duration of SCL wear was statistically significantly greater than those for 1-5 years and 6-10 years (Table 2). Van Bijsterveld ocular surface fluorescein staining was positive for ≥ 2 years (mean value, 11.4 (6.6) years) duration of SCL wear. We found that LWE scores and LIPCOF scores for myopic patients wearing SCL for 1-5 years were significantly lower than for those wearing SCL for > 10 years (p = 0.00005 and p = 0.0001, respectively, Table 3).
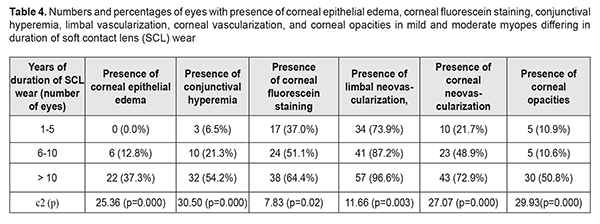
LWE and Lipcof tests were positive for myopic patients wearing SCL for ≥1 year (mean values, 12.3 (7.9) years and 10.6 (7.4) years, respectively). Corneal sensitivity loss was statistically more significant for > 10 years duration of SCL wear. A moderate corneal sensitivity loss was found for a mean SCL wear duration of 10.8 (6.8) years (range, 1 to 34 years), and severe corneal sensitivity loss, for a mean SCL wear duration of 16.4 (9.0) years (range, 5 to 41 years). Corneal epithelial edema was found in some myopic patients wearing SCL for 6-10 years, and in as much as 37.5% of those wearing SCL for >10 years (Table 4). The mean duration of SCL wear for which corneal epithelial edema was found was 12.4 (3.5) years.
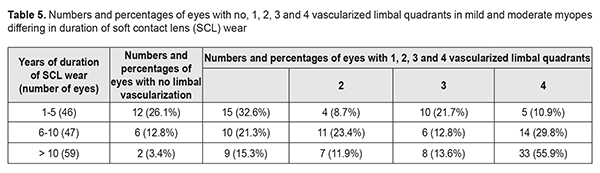
Corneal hyperemia was found in some myopic patients wearing SCL for 1-5 years, and in more than 50% of those wearing SCL for >10 years. The mean duration of SCL wear for which corneal hyperemia was found was 12.4 (3.5) years. Corneal fluorescsin staining was positive in 37.0%, 51.1%, and 64.4% of patients wearing SCL for 1-5 years, 6-10 years, and >10 years, respectively. The mean duration of SCL wear for which corneal fluorescsin staining was positive was 10.9 (6.5) years (Table 4), with the minimum duration of 3 years. Limbal vascularization was seen in 73.9%, 87.2%, and almost all eyes (96.6%) of patients wearing SCL for 1-5 years, 6-10 years, and >10 years, respectively (Table 4), and patients with greater duration of SCL wear had an increased number of quadrants involved (Table 5). The mean duration of SCL wear for which limbal vascularization was found was 10.8 (7.4) years, with the minimum duration of 1 year.
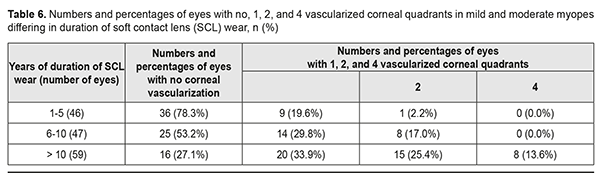
Corneal vascularization was found in myopic patients with any duration of SCL wear: in 21.7%, 48.9%, and 72.9% of patients wearing SCL for 1-5 years, 6-10 years, and >10 years, respectively (Table 3). The mean duration of SCL wear for which corneal vascularization was found was 12.9 (8.3) years, with the minimum duration of more than 2 years. Table 6 shows numbers and percentages of patients with different numbers of corneal quadrants affected by vascularization for each category of duration of SCL wear. All the four corneal quadrants were affected by vascularization only in some patients wearing SCL for > 10 years. Corneal opacities were found in 10.0-110% of patients wearing SCL for ≤10 years, and in as much as half of those wearing SCL for >10 years (Table 4). The mean duration of SCL wear for which corneal opacity was found was 13.9 (7.6) years, with the minimum duration of more than 4 years. Pearson’s chi-square test found that presence of corneal epithelial edema, conjunctival hyperemia, corneal fluorescein staining, limbal vascularization, corneal vascularization, and corneal opacities were associated with duration of SCL wear.
Overall OSDI score, LIPCOF score, LWE score, FTBUT, Baylor corneal staining score, van Bijsterveld ocular surface fluorescein staining score, corneal sensation, presence of corneal epithelial edema, positive corneal fluorescein staining, conjunctival hyperemia, presence and degree of limbal vascularization, presence and degree of corneal vascularization and presence of corneal opacity, but not Schirmer I score, Schirmer II score and corneal central thickness significantly depended on duration of SCL wear. Mean durations of SCL wear for which Schirmer I and Schirmer II scores were below normal were 10.3 (7.3) years and 10.6 (7.4) years, respectively, with the minimum duration of 1 year. Mean duration of SCL wear for which corneal thickness was ≤ 490 nm was 10.2 (5.0) years, with the minimum duration of 2 years. Conclusion In mild and moderate myopes wearing soft contact lenses, overall OSDI score, LIPCOF score, LWE score, FTBUT, Baylor corneal staining score, van Bijsterveld ocular surface fluorescein staining score, low corneal sensitivity, presence of corneal epithelial edema, corneal fluorescein staining, conjunctival hyperemia, presence and degree of limbal vascularization, presence and degree of corneal vascularization, and presence of corneal opacity were found to statistically significantly depend on duration of SCL wear. Silicone hydrogel contact lens wearers began feeling ocular discomfort as early as 1-5 years after they began using these lenses. An OSDI test found mild ocular surface disease in myopic patients wearing lenses for ≤ 5 years, and moderate ocular surface disease, in those wearing lenses for > 5 years. There was a high probability of a severe corneal sensation loss (80%) for overall OSDI score ≥32.5 (i.e., moderate ocular surface disease). Early pathological changes in the ocular surface were usually found in patients wearing SCL for 1-5 years, and severe changes, in those wearing SCL for > 10 years. Decreased tear production and quality, lid-wiper epitheliopathy as shown by fluorescein staining (LWE test), conjunctival folds (LIPCOF test), conjunctival hyperemia, corneal opacities, limbal and corneal vascularization were observed in patients wearing SCL for at least a year. Corneal edema and presence of corneal and conjunctival fluorescein staining were found in patients wearing SCL for at least 6 years. Loss of central corneal sensitivity was noted in patients wearing SCL for > 10 years.
The obtained data complement the knowledge on the pathological changes in the ocular surface with duration of SCL wear, and will contribute to understanding of the causes of severe complications associated with contact lens correction. References 1.Alipour F, Kheirkhah A, Jabarvand Behrouz M. Use of mini scleral contact lenses in moderate to severe dry eye. Cont Lens Anterior Eye. 2012 Dec;35(6):272-6. 2.Dimit R, Gire A, Pflugfelder SC, Bergmanson JP. Patient ocular conditions and clinical outcomes using a PROSE scleral device. Cont Lens Anterior Eye. 2013 Aug;36(4):159-63. 3.Ling JD, Gire A, Pflugfelder SC. PROSE therapy used to minimize corneal trauma in patients with corneal epithelial defects. 2013 Apr;155(4):615-619, 619.e1-2. 4.Lorenzo-Morales J, Khan NA, Walochnik J. An update on Acanthamoeba keratitis: Diagnosis, pathogenesis and treatment. Parasite. 2015;22:10. 5.Pecego M, Barnett M, Mannis MJ, Durbin-Johnson B. Jupiter scleral lenses: The UC Davis Eye Center experience. Eye Contact Lens. 2012 May;38(3):179-82. 6.Pullum K, Buckley R. Therapeutic and ocular surface indications for scleral contact lenses. Ocul Surf. 2007 Jan;5(1):40-8. 7.Romero-Jiménez M, Flores-Rodríguez P. Utility of a semi-scleral contact lens design in the management of the irregular cornea. Cont Lens Anterior Eye. 2013 Jun;36(3):146-50. 8.Rosenthal P, Croteau A. Fluid-ventilated, gas-permeable scleral contact lens is an effective option for managing severe ocular surface disease and many corneal disorders that would otherwise require penetrating keratoplasty. Eye Contact Lens. 2005 May;31(3):130-4. 9.Ahmed II, Breslin CW. Role of the bandage soft contact lens in the postoperative laser in situ keratomileusis patient. Cataract Refract Surg. 2001 Dec;27(12):1932-6. 10.Baran I, Bradley JA, Alipour F, et al. PROSE treatment of corneal ectasia. Cont Lens Anterior Eye. 2012 Oct;35(5):222-7. 11.Lee JC, Chiu GB, Bach D, et al. Functional and visual improvement with prosthetic replacement of the ocular surface ecosystem scleral lenses for irregular corneas. Cornea. 2013 Dec;32(12):1540-3. 12.Segal O, Barkana Y, Hourovitz D, et al. Scleral contact lenses may help where other modalities fail. Cornea. 2003 May;22(4):308-10. 13.Ciralsky JB, Chapman O, Rosenblatt MI, et al. Treatment of Refractory persistent corneal epithelial defects: A standardized approach using continuous wear PROSE therapy. Ocul Immunol Inflamm. 2015 Jun;23(3):219-24. doi: 10.3109/09273948.2014.894084. 14.Lim P, Ridges R, Jacobs DS, Rosenthal P. Treatment of persistent corneal epithelial defect with overnight wear of a prosthetic device for the ocular surface. Am J Ophthalmol. 2013 Dec;156(6):1095-101. doi: 10.1016/j.ajo.2013.06.006. 15.Abdelkader A. Cosmetic soft contact lens associated ulcerative keratitis in Southern Saudi Arabia. Middle East Afr J Ophthalmol. 2014. 2014 Jul-Sep;21(3):232-5. doi: 10.4103/0974-9233.134677. 16.Dumbleton K, Caffery B, Dogru M. The TFOS International Workshop on Contact Lens Discomfort: Report of the subcommittee on epidemiology. Invest Ophthalmol Vis Sci. 2013 Oct 18;54(11):TFOS20-36. doi: 10.1167/iovs.13-13125. 17.Alipour F, Khaheshi S, Soleimanzadeh M, et al. Contact Lens-related Complications: A Review. J Ophthalmic Vis Res. 2017 Apr-Jun;12(2):193-204. doi: 10.4103/jovr.jovr_159_16. 18.McMonnies CW. How contact lens comfort may be influenced by psychiatric and psychological conditions and mechanisms. Clin Exp Optom. 2014 Jul;97(4):308-10. doi: 10.1111/cxo.12122. 19.Stapleton F, Keay L, Edwards K, et al. The incidence of contact lens-related microbial keratitis in Australia. Ophthalmology. 2008 Oct;115(10):1655-62. doi: 10.1016/j.ophtha.2008.04.002. 20.Willcox MD, Naduvilath TJ, Vaddavalli PK, et al. Corneal erosions, bacterial contamination of contact lenses, and microbial keratitis. Eye Contact Lens. 2010 Nov;36(6):340-5. doi: 10.1097/ICL.0b013e3181f57b05. 21.Abdelfattah NS, Amgad M, Zayed AA, et al. Clinical correlates of common corneal neovascular diseases: A literature review. Int J Ophthalmol. 2015 Feb 18;8(1):182-93. doi: 10.3980/j.issn.2222-3959.2015.01.32. 22.Papas E. Corneal vascularisation and contact lenses. Arch Soc Esp Oftalmol. Arch Soc Esp Oftalmol. 2006 Jun;81(6):309-12. 23.Shah SS, Yeung KK, Weissman BA. Contact lens-related deep stromal vascularization. Int Contact Lens Clin. 1998;25:128–36. 24.Liesegang TJ. Physiologic changes of the cornea with contact lens wear. CLAO J. 2002 Jan;28(1):12-27. 25.Su SB, Lu CW, Sheen JW, et al. Tear secretion dysfunction among women workers engaged in light-on tests in the TFT-LCD industry. BMC Public Health. 2006 Dec 16;6:303. 26.Szczotka-Flynn L, Chalmers R. Incidence and epidemiologic associations of corneal infiltrates with silicone hydrogel contact lenses. Eye Contact Lens. 2013 Jan;39(1):49-52. doi: 10.1097/ICL.0b013e318271d3dc. 27.Szczotka-Flynn LB, Pearlman E, Ghannoum M.. Microbial contamination of contact lenses, lens care solutions, and their accessories: a literature review. Eye Contact Lens. 2010 Mar;36(2):116-29. doi: 10.1097/ICL.0b013e3181d20cae. 28.Thomas PA, Kaliamurthy J. Mycotic keratitis: Epidemiology, diagnosis and management. Clin Microbiol Infect. 2013 Mar;19(3):210-20. doi: 10.1111/1469-0691.12126. 29.Zaidi T, Mowrey-Mckee M, Pier GB. Hypoxia increases corneal cell expression of CFTR leading to increased Pseudomonas aeruginosa binding, internalization, and initiation of inflammation. Invest Ophthalmol Vis Sci. 2004 Nov;45(11):4066-74. 30.Alarcon I, Tam C, Mun JJ, et al. Factors impacting corneal epithelial barrier function against Pseudomonas aeruginosa traversal. Invest Ophthalmol Vis Sci. 2011 Mar 14;52(3):1368-77. doi: 10.1167/iovs.10-6125. 31.Fleiszig SMJ. The Glenn A. Fry award lecture 2005. The pathogenesis of contact lens-related keratitis. Optom Vis Sci. 2006 Dec;83(12):866-73. 32.Cheng KH, Leung SL, Hoekman HW. Incidence of contact-lens-associated microbial keratitis and its related morbidity. Lancet. 1999 Jul 17;354(9174):181-5. 33.Schein OD, McNally JJ, Katz J, et al. The incidence of microbial keratitis among wearers of a 30-day silicone hydrogel extended-wear contact lens. Ophthalmology. 2005 Dec;112(12):2172-9. 34.Seal DV, Kirkness CM, Bennett HG, et al. Population-based cohort study of microbial keratitis in Scotland: Incidence and features. Cont Lens Anterior Eye. 1999;22(2):49-57. 35.Yildiz EH, Abdalla YF, Elsahn AF, et al. Update on fungal keratitis from 1999 to 2008. Cornea. 2010 Dec;29(12):1406-11. doi: 10.1097/ICO.0b013e3181da571b. 36.Alfonso EC, Miller D, Cantu-Dibildox J, et al. Fungal keratitis associated with non-therapeutic soft contact lenses. Am J Ophthalmol. 2006 Jul;142(1):154-5. 37.Suvajac G. [Soft-contact-lenses-induced complications]. Vojnosanit Pregl. 2008 Jan;65(1):15-20. Serbian. 38.Wolkoff P, Kärcher T, Mayer H. Problems of the “outer eyes” in the office environment: An ergophthalmologic approach. J Occup Environ Med. 2012 May;54(5):621-31. doi: 10.1097/JOM.0b013e31824d2e04. 39.Lamer L. Extended wear contact lenses for myopes: A follow-up study of 400 cases. Ophthalmology. 1983 Feb;90(2):156-61. 40.Alemany A, Redal P. Giant papillary conjunctivitis in soft and rigid lens wear. Contactologica. 1991;13:14–7. 41.Donshik PC. Contact lens chemistry and giant papillary conjunctivitis. Eye Contact Lens. 2003 Jan;29(1 Suppl):S37-9. 42.Sorbara L, Jones L, Williams-Lyn D. Contact lens induced papillary conjunctivitis with silicone hydrogel lenses. Cont Lens Anterior Eye. 2009 Apr;32(2):93-6. doi: 10.1016/j.clae.2008.07.005. 43.Porazinski AD, Donshik PC. Giant papillary conjunctivitis in frequent replacement contact lens wearers a retrospective study. CLAO J. 1999 Jul;25(3):142-7.
|