J.ophthalmol.(Ukraine).2018;5:15-19.
|
https://doi.org/10.31288/oftalmolzh201851519 Received: 30 May 2018; Published on-line: 26 October 2018 Efficacy of bioflavonoid quercetin in treatment of herpetic keratitis patients with dry eye syndrome S. Ya. Rafalyuk1; T.B. Gaydamaka2, Dr. Sc. (Med.) 1 Danylo Halytsky Lviv National Medical University; Lviv (Ukraine) 2 Filatov Institute of Eye Diseases and Tissue Therapy, NAMS of Ukraine" Odesa (Ukraine) E-mail: sofiyaeye@ukr.net TO CITE THIS ARTICLE: Rafalyuk SYa, Gaydamaka TB. Efficacy of bioflavonoid quercetin in treatment of herpetic keratitis patients with dry eye syndrome. J.ophthalmol.(Ukraine).2018;5:15-19. https://doi.org/10.31288/oftalmolzh201851519 Introduction. Dry eye syndrome has drown a special attention of ophthalmologists not only because of its prevalence but also due to the increased frequency among patients with inflammatory processes in the cornea and conjunctiva. Purpose. To study the effect of bioflavonoid quercetin on the course of the inflammatory process in patients with herpetic keratitis (HK) and dry eye syndrome (DES). Material and Methods. Clinical study involved 40 patients (40 eyes) with HK (superficial keratitis) and DES; in addition, we followed up 17 patients (17 eyes) with HK-only. All patients involved in the clinical study were divided into two groups: Study Group, HK and DES patients receiving bioflavonoid quercetin, containing in Lipoflavon drug, in addition to traditional treatment, 15 patients; Control Group, HK and DES patients receiving only traditional treatment, 25 patients. Results. Clinical study findings showed that the inclusion of bioflavonoid quercetin (Lipoflavon) in the complex treatment of HK patients with DES significantly decreased the intensity of clinical signs and made it possible to decrease the treatment duration. Corneal dendritic ulceration epithelization was observed significantly earlier in patients with HK and SED receiving Lipoflafon as compared to controls, at Day (4.7±0.4) vs. Day (6.8±0.6), respectively; no corneal infiltration was observed at Days (5.5±0.5) and (7.8±0.7) in Study and Control groups, respectively. Schirmer test II values were (10.47±0.83) mm/5 min and (7.36±0.28) mm/5 min in Study and Control groups, respectively. Tear break-up time equaled (6.13±0.32) and (5.24±0.19) s, in Study and Control groups, respectively. Conclusions. Inclusion of bioflavonoid quercetin in the complex treatment of patients with herpetic keratitis and dry eye syndrome significantly increases the therapy efficacy, which is evidenced by accelerated corneal epithelization and infiltrate dispersion and significantly improved qualitative and quantitative characteristics of tear production. Keywords: herpetic keratitis, dry eye syndrome, Lipoflavon
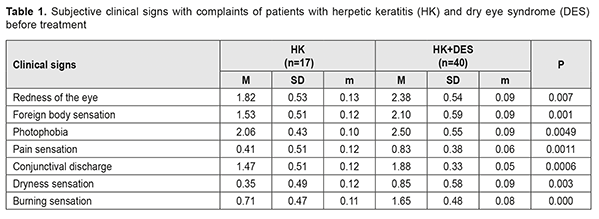
Introduction Over the last years, the problem of dry eye syndrome has been of a great importance due to its significant prevalence rate. Today, dry eye syndrome is rightfully considered a disease of civilization. According to the literature, dry eye syndrome is observed in 9-18% of population [2, 5, 10, 15]. Dry eye syndrome has drown so much attention of ophthalmologists not only because of its prevalence but also due to increased frequency among patients with inflammatory processes in the cornea and conjunctiva. The incidence rate of dry eye syndrome among patients with corneal and conjunctival diseases, according to different authors, varies within 25-96% [1, 4]. Using traditional medications for keratitis treatment does not always lead to patient’s cure and recurrence prevention [3, 9, 14, 17]. In this regard, a search for a reasonable etiopathogenic therapy for keratitis and dry eye syndrome is of relevance [11, 12, 13, 16]. In our previous experimental works, bioflavonoid quercetin was found to have a significant therapeutic effect on the inflammatory process in the cornea in the presence of dry eye syndrome in correction of the metabolic state of anterior eye tissues [8]. Experimental data give the rationale for using bioflavonoid quercetin in the clinical practice for herpetic keratitis patients with dry eye syndrome. In addition, our previous studies have revealed that bioflavonoid quercetin, a natural anti-oxidant containing in Lipoflavon drug, decreases the degree of disorders in biochemical characteristics in the tear fluid of patients with herpetic keratitis (HK) and dry eye syndrome (DES). Therefore, it decreases a destabilizing effect of DES on the corneal epithelium in keratitis [7]. The purpose of the present paper was to study the effect of bioflavonoid quercetin on the course of the inflammatory process in HK patients with DES. Material and Methods Clinical study involved 40 patients (40 eyes) with HK (superficial keratitis) and DES; in addition, we followed up 17 patients (17 eyes) with HK-only. All patients involved in the clinical study were divided into two groups: Study Group, HK and DES patients receiving bioflavonoid quercetin, containing in Lipoflavon drug, in addition to traditional treatment, 15 patients; Control Group, HK and DES patients receiving only traditional treatment, 25 patients. The state of the anterior eye tissues was scored by criteria that follow: corneal and conjuctival fluorescein staining, tear meniscus, conjunctival injection score, conjunctival discharge, conjunctival folds, corneal edema, corneal infiltration, Schirmer test II, and tear break-up time. Traditional therapy included anti-herpetic drugs locally and parenterally (aciclovir, valaciclovir, ganciclovir), antiseptics and antibiotics (if indicated), non-steroid anti-inflammatory drugs, mydriatics, tear substitutes, and corticosteroids at a proper stage of the disease. The SPSS 11.0 package was used to statistically process the data obtained [6]. Results A comparative analysis of objective and subjective clinical characteristics in HK-only and HK patients with DES showed that all inflammatory signs were more expressed in HK patients with DES as compared to those in HK patients without DES. Based on the Table 1 data, all inflammatory signs were lower in HK patients than in HK patients with DES. The difference was significant for such signs studied as: foreign body sensation (р=0.001); photophobia (р=0.0049); pain sensation (р=0.0011); conjunctival discharge (р=0.0006); dryness (р=0.003) and burning (р=0.000) sensation.
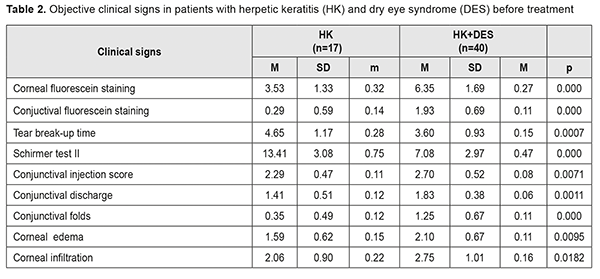
Based on the Table 2 data, all clinical signs of the inflammatory process were higher in HK patients with DES. The difference was significant for such signs studied as: conjuctival fluorescein staining (р=0.000); conjunctival discharge (р=0.0011). Also, qualitative and quantitative characteristics of tear production were significantly decreased in HK patients with DES as compared to those in HK-only patients.
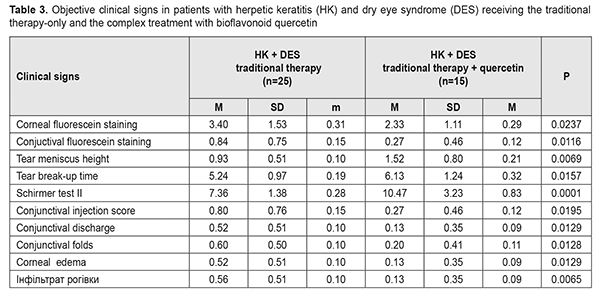
The next stage of our study was to compare the effect of treatment on these signs in HK patients with DES receiving a traditional therapy and in HK patients with DES receiving a complex therapy with bioflavonoid quercetin (Lipoflavon).
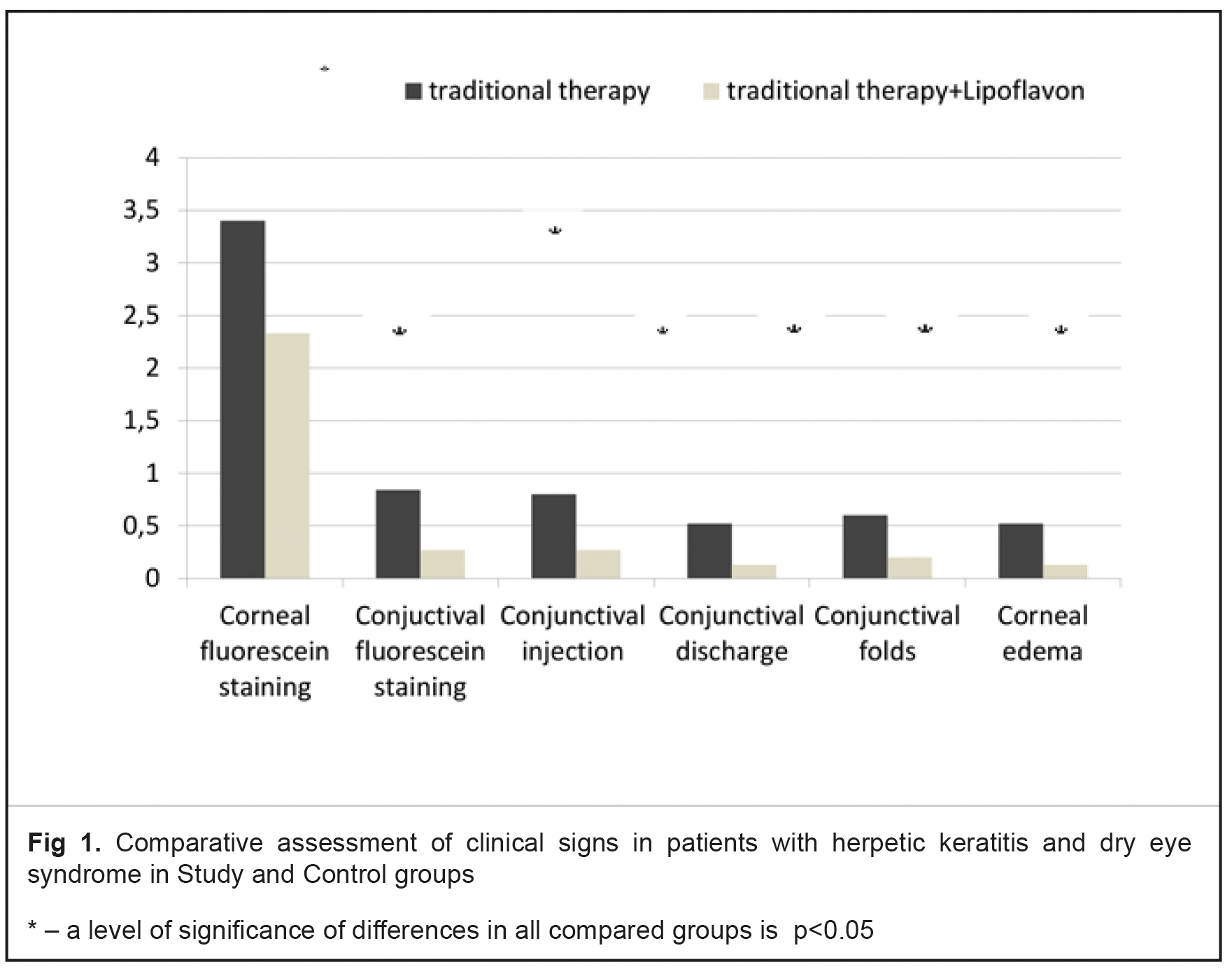
The Graph 1 demonstrates the findings of clinical sign analysis in HK patients with DES receiving a traditional therapy in comparison with those receiving a complex therapy with Lipoflavon (Fig. 1).
At Day 7 of treatment, the corneal fluorescein staining score in patients with HK and SED receiving Lipoflafon was less expressed as compared to control, (2.33±0.29) vs. (3.40±0.31), respectively; punctate conjuctival fluorescein staining score in Study and Control groups was (0.27±0.12) and (0.84±0.15), respectively; the height of tear meniscus in Study and Control groups was equal to (1.52±0.10) and (0.93±0.21) mm, respectively; tear break-up time equaled (6.13±0.32) and (5.24±0.19) s, in Study and Control groups, respectively; Schirmer test II values were (10.47±0.83) mm/5 min and (7.36±0.28) mm/5 min in Study and Control groups, respectively; conjunctival injection in HK and SED decreased to (0.27±0.12) scores after quercetin treatment compared to (0.80±0.15) scores in Control group; conjuncival discharge intensity score in Study and Control groups was (0.13±0.09) and (0.52±0.10), respectively; the presence of conjunctival folds in HK and DES and Lipoflavon treatment was (0.20±0.11) scores vs. (0.60±0.10) scores in Control group; corneal edema was less apparent in Study group as compared to controls, (0.13±0.09) and (0.52±0.10), respectively. Corneal dendritic ulceration epithelization was observed significantly earlier in patients with HK and SED receiving Lipoflafon as compared to controls, at Day (4.7±0.4) vs. Day (6.8±0.6), respectively; no corneal infiltration was observed at Day (5.5±0.5) and (7.8±0.7) in Study and Control groups, respectively. Conclusions Clinical study findings showed that inclusion of bioflavonoid quercetin (Lipoflavon) in the complex treatment of HK patients with DES significantly decreased the intensity of clinical signs and made it possible to decrease the treatment duration. 1.Inclusion of bioflavonoid quercetin in the complex treatment of patients with herpetic keratitis and dry eye syndrome significantly increases the therapy efficacy, which is evidenced by the time of corneal epithelization and infiltrate dispersion accelerated by 30.8% and 29.5%, respectively, as compared to controls. In addition, corneal edema, epitheliopathy of the cornea and conjunctiva decreased significantly by 25%. 2.Bioflavonoid quercetin has a positive effect on the qualitative and quantitative characteristics of tear production, which is evidenced by increased Schirmer test values, increased tear break-up time, decreased conjunctival folds, increased tear meniscus height, by 29.7%, 14.5%, 66%, and 38.8%, respectively, as compared to those in patients receiving the traditional treatment without bioflavonoid quercetin
References 1.Anina EI. [The prevalence of the cornea diseases among the population of Ukraine. Abstracts of II Black Sea International scientific conference ophthalmologists]. Odessa, 2004:14. Ukrainian 2.Brzheskij VV. [Diseases of the lacrimal apparatus: a manual for practicing doctors. 2nd ed. St. Petersburg].: Izdatelstvo N.-L .; 2009.106 p. Russian 3.Drozhzhina GI. [Modern methods of treatment of the dry eye syndrome]. Ophthal Zh. 2013; 5: 89-95. Ukrainian 4.Drozhzhina GI. [Viral diseases of the cornea and conjunctiva]. Zdorovya Ukrainy. 2002;5:35-36. Ukrainian 5.Zhaboedov DG, Kireev VV. [Dry eye syndrome: clinical picture, diagnosis and treatment. Guidelines for medical students and practitioners]. Kyiv, 2006. 24 p. Ukrainian 6.Nasledov A. [SPSS computer analysis of data analysis in psychology and social sciences].Spb.: Piter; 2005.416 p. Russian 7.Gaydamaka TB, Rafalyuk SY. [Effect of Lipoflavone on the activity of oxidation-reduction enzymes in tear fluid in keratitis in patients with dry eye syndrome]. Oftalmologiia. 2016.2:54-7. Ukrainian 8.Rafalyuk SY. [The possibility of metabolic correction of pathological disorders of the cornea in induced keratitis in animals with dry eye syndrome]. Oftalmologiia. 2015.2:211-20. Ukrainian 9.Skripnik RL, Skripnichenko RL. [New in the treatment of dry eye syndrome]. Ukr. Med. Chasopys.2011.1 (81): 79-80. Ukrainian 10.Somov EE. [Tear dysfunction syndrome: anatomic and physiological basis, diagnosis, clinical picture and treatment]. St. Petersburg: Chelovek; 2011.160 p. Russian 11.Somov EE. [Etiopathogenetic basis of the "dry eye" syndrome and principles of approach to its treatment. In: Materials of the jubilee scientific conference dedicated to the 75th anniversary of the foundation of the first in Russia Department of Children's Ophthalmology "Nevskie Horizonty-2010"].St. Petersburg, 2010.Oct.2:482-487. Russian 12.Baudouin C. The pathology of dry eye. Surv Ophthalmol. 2001 Mar;45 Suppl 2:S211-20. 13.Begley CG, Chalmers RL, Abetz L, Venkataraman K, Mertzanis P, Caffery BA, Snyder C, Edrington T, Nelson D, Simpson T. The relationship between habitual patient-reported symptoms and clinical signs among patients with dry eye of varying severity. Invest Ophthalmol Vis Sci. 2003 Nov;44(11):4753-61. PMid:14578396 14.Bourcier T, Acosta MC, Borderie V, Borrás F, Gallar J, Bury T, Laroche L, Belmonte C. Decreased corneal sensitivity in patients with dry eye. Invest Ophthalmol Vis Sci. 2005 Jul;46(7):2341-5. PMid:15980220 15.Brewitt H, Sistani F. Dry eye disease: the scale of the problem. Surv Ophthalmol. 2001 Mar;45 Suppl 2:S199-202. 16.Javadi MA, Feizi S. Dry eye syndrome. J Ophthalmic Vis Res. 2011 Jul;6(3):192-8. PMid:22454735 PMCid:PMC3306104 17.Wilson SE, Netto M, Ambrósio R Jr. Corneal cells: chatty in development, homeostasis, wound healing, and disease. Am J Ophthalmol. 2003 Sep;136(3):530-6.
|