J.ophthalmol.(Ukraine).2018;5:72-74.
|
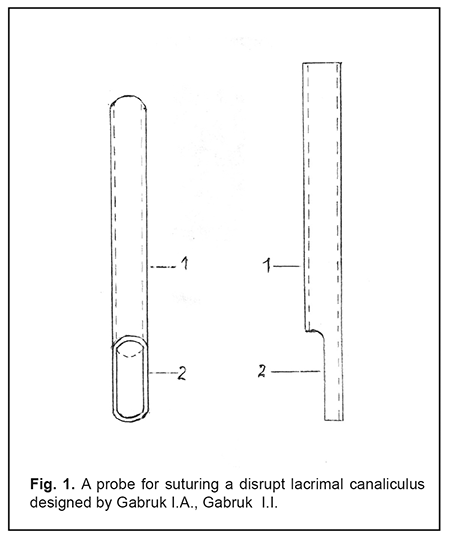
https://doi.org/10.31288/oftalmolzh201857274 Received: 15 June 2018; Published on-line: 26 October 2018 A method of primary microsurgical debridement of lacrimal canaliculus ruptures in eyelid injuries I.A. Gabruk, Ohthalmologist; I.I. Gabruk Vinnitsa Regional Clinical Hospital named after N.I.Pirogov National Pirogov Memorial Medical University, Vinnytsya Vinnitsa (Ukraine) TO CITE THIS ARTICLE: Gabruk IA, Gabruk II. A method of primary microsurgical debridement of lacrimal canaliculus ruptures in eyelid injuries. J.ophthalmol.(Ukraine).2018;5:72-74. https://doi.org/10.31288/oftalmolzh201857274 Background Eyelid injuries with the rupture of lacrimal canaliculi are most common for injuries to the lacrimal drainage system and make up approximately 47-48 % of all eyelid injuries. In the absence of correctly-performed primary microsurgical debridement (PMCD) of such injuries there can be formed coloboma and deformation of the eyelid, irreversible strictures and obliteration of canaliculi. Permanent unbearable tears, sour eyes, and limitation of capability for work-related activity require performing reconstructive surgery. PMCD of fresh injuries is much more effective than reconstructive surgery in the period of scarring when it is difficult to find and suture ends of a disrupted canaliculus. Such patients make up a considerable part of incurable watery eye. That is why, the development of PMCD of the eyelid injuries with lacrimal canaliculus ruptures is of relevance. In PMCD of such wounds, the ends of a disrupted lacrimal canaliculus are sutured “end to end” on a special probe carrier. Different variants have been proposed for their matching, suturing and keeping immobilized, including metal and synthetic rods or tubes, catgut, veins, polymer tubes etc. Coming out of a lacrimal canaliculus, such canaliculus probes are glued or sutured to the eyelids, cheeks, or forehead and they are easy to accidently catch, replace, and even to remove. Hard probes cause pressure injuries so they contribute to stricture formation. A tube or a vein, coming out of the lacrimal canaliculus to the eyelid, pulls out a lacrimal punctum and the eyelid wound is closed with an everted lacrimal punctum. The probes sutured to the facial skin are kept from three weeks to three months, which creates an aesthetic defect. Bringing the silicone threads or tubes, including prostheses manufactured by Eagle Vision, FCI, and others, through the ruptured lacrimal canaliculus, lacrimal sac, nasolacrimal duct into the nasal cavity is a quite challenging and rather traumatic procedure. Suturing the lacrimal canaliculus using a silicone or polyethylene tube is considered to be the best method. The silicone or polyethylene tube-carrier with an external diameter of 1.2 mm is inserted through the lacrimal punctum, lateral and medial parts of the ruptured canaliculus to the lacrimal sac; on this tube, the ruptured canaliculus is secured “end to end” with interrupted 10/00 nylon, silk, or other sutures, which is followed by suturing the ruptured eyelid. The tube is firmly secured with 7-8/00 silk sutures to the eyelid margin (the sutures can be easily cut) and the rest of the tube is cut off at 0.5 mm above the lacrimal punctum. The sutures fixating the silicone tube to the eyelid can be easily cut through, which is confirmed by the authors. Thanks to its flexibility, the tube constantly streatches the securing sutures and pulls them while blinking. When these sutures are cut through, the tube gets shifted and even fallen out from the lacrimal canaliculus, disturbing, thus, immobilization of both its parts. This leads to the formation of the canaliculus structure. The incubation of the canaliculus by a silicone and polyethylene tube performs a temporary framework function and does not create conditions for simultaneous tear lead, which contributes to watery and sour eyes, cut sutures, and, thus, empedes healing. Purpose. To improve the efficacy of surgery and to avoid the stricture of the lacrimal canaliculus through providing correct matching, suturing, and secure stable immobilization of the connection of both ends of the ruptured lacrimal canaliculus for a required period of time with simultaneous elimination of the tear. Material To meet the purpose, we proposed a canalicular probe of our own design (patent No 124617 from 10 April 2018). It is designed as a silicone or polyethylene tube, 1-1.2 mm in diameter and 12 mm in length. The length of the tube must be equal to the horizontal size of the lacrimal canaliculus with addition of 2 mm for the depth of the lacrimal sac. If necessary, the tube can be shortened by cutting off its medial end. The Figure 1 demonstrates the proposed canalicular probe. From the lateral end, a half of the tube (1) is cut off for 2.5-3 mm, and another half (2) is secured with interrupted U-shaped 6/00 sutures with 2 mm interval at 1-1.5 mm from the tube’s end. The suture ends go out from the tube and are not tied. A method of PMCD of the lacrimal canaliculus rupture in eyelid injuries consists in performing an operation as follows. Surgical revision of the wound. Both ends of the ruptured lacrimal canaliculus are found. The interior wall of the lacrimal canaliculus is deleted along 2.5-3.0 mm from the lacrimal punctum. The canalicular probe (a silicon tube) is inserted by a medial end through the lacrimal puncta into the distal part of the disrupt canaliculus in such a way that the lateral end of the tube, sutured with a thread, coincides with the lateral end of the horizontal part of the lacrimal canaliculus and the cut side wall of the tube is towards the eyeball. This hole of the tube can be seen from inside of the eyelid where the removed inner wall of the canaliculus is absent. Both ends of U-shaped suture, which the tube is transfixed with, are passed through separate punctures, released on the anterior surface of the eyelid, and tied. The probe is secured in the distal part of the disrupt canaliculus. The U-shaped 6/00 stitch, penetrating at 5 mm from the wound margin with an interval of 2-3 mm, is put and left untied on the eyelid wound and on the inner palpebral ligament or periorbit in the site of the ligament rupture; afterwards, it is punctured out on the skin more medially according to the anterior lacrimal crest. In addition, a 9-10/00 suture is put on the anterior and posterior walls of both ends of the disrupt canaliculus, one for each. The U-shaped stitch is put so that the eyelid is pulled medially backwards and upwards for the lower lid. These sutures are tightened. The medial end of the silicone tube is passed through the medial part of the disrupt canaliculus into the lacrimal sac using a stiff guide wire. Both sutures on the lacrimal canaliculus and the U-shaped suture on the underlay are tied. Afterwards, the rest of stitches are put on the wound margin. If it is impossible to find in the wound the end of the proximal part of the disrupt inferior canaliculus then, firstly, a U-shaped suture is put and left untight and, secondly, a tubular spiral-shaped probe, a so-called “pigtail” desighed by Lebekhov P.I., Mogutin G.M., Korkhmarosh et al., is passed in the wound retrogradely through the intact inferior lacrimal canaliculus and the proximal part of the disrupted canaliculus. A thread, 0.3-0.4 mm in diameter, is passed through this probe until it is released from the probe into the wound. The thread is handled by forceps and the probe is removed retrogradely. The thread is passed through the silicone tube (the canacular probe), entering the proximal end and releasing from the lateral end of the disrupt canaliculus. Along the thread, the silicone tube is inserted into the proximal part of the disrupt canaliculus and, after putting two stitches on both ends of the disrupted canaliculus, the thread is removed. To check the correctness of the tube’s placement in the canaliculus, it is administered a normal saline which must run to the nose. In the same way, the disrupted inferior canaliculus is sutured in case when it is ruptured near the very lacrimal sac. To find the medial end of the disrupted superior canaliculus, the spiral-shaped probe (“pigtail”) is not passed retrogradely through the uninjured inferior canaliculus because this operation can be a greater risk than the unsutured superior lacrimal canaliculus. In such cases, the eyelid only is sutured. After the surgery, the eyes are bandaged for 2-3 days with a daily redressment. In the post-operative period, the lacrimal ducts are washed with antiseptics through the silicone tube and the intact canaliculus. The silicone tube is removed from the lacrimal canaliculus at 2-3 months after the surgery, cutting the suture tie in the eyelid and grabbing the lateral end of the tube with forcips or a curved needle. After removing the tube, the canaliculus is washed with anticeptics once a week for one month. Results We used the proposed technique in surgery of 6 patients with a lacrimal canaliculus rupture in its medial inner third. The one year follow up showed that the tear flow through the injured canaliculus was completely recovered, canalicular and lacrimonasal tests were positive, and no tearing was observed. In one case, when the canaliculus ruptured near the lactrimal sac, the stricture was formed. Conclusions Firstly, the suture, securing the tube to the eyelid, can never be cut so the tube cannot be replaced and fallen out; it provides the connection of the disrupted canaliculus ends with stable and secure immobilization for the required period of time. Secondly, tear flow around and in the tube is partially recovered after redressing the bandage and rinsing through the tube and the intact superior canaliculus for the first time. Thirdly, The silicone tube is placed completely in the horizontal part of the lacrimal canaliculus and in the lacrimal sac so it cannot be seen by surrounded people and it does not cause the eyelid deformation. Finally, a tie on the eyelid is low-observable, it does not contact with and does not irritate the eyeball. We believe that a PMCD method of an eyelid wound with a lacrimal canaliculus rupture using a proposed flexible silicone canalicula probe, which is placed and secured only in the horizontal part of the lacrimal canaliculus, is quite effective. The important stage of the operation is the correct suturing of the eyelid to the medial canthus when the eyelid is pulled medially backwards and upwards.
References
1. Brzheskii VV, Troianovskii RL. [Surgical treatment of lacrimal passage injuries. Modern Ophthalmology. Guidance for physicians. Edited by Danilichev VF. SPb; 2000. 398p. Russian.
|