J.ophthalmol.(Ukraine).2018;4:7-10.
|
https://doi.org/10.31288/oftalmolzh20184710 Received: 17 April 2018; Published on-line: 31 August 2018 A two-stage laser surgery for fibroplastic changes of the vitreous humor P. P. Chechin, Cand. Sc. (Med.), K.G. Drachenko, O.V. Guzun, Cand. Sc. (Med.), S.K. Drachenko Filatov Institute of Eye Diseases and Tissue Therapy of NAMS of Ukraine; Odessa (Ukraine) E-mail: olgaguzun@mail.ru TO CITE THIS ARTICLE: Chechin PP, Drachenko KG, Guzun OV, Drachenko SK. A two-stage laser surgery for fibroplastic changes of the vitreous humor. J.ophthalmol.(Ukraine).2018;4:7-10. https://doi.org/10.31288/oftalmolzh20184710
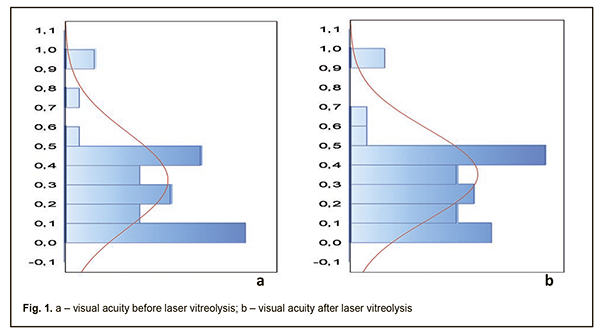
Background. Patients with profilerative vitreoretinopathy are performed vitrectomy which, however, is challenging in the presence of high visual function, transparent lenses, and single vitreoretinal adhesion bands as well as at risk of hemorrhages. Purpose. To determine the efficacy of a two-stage laser treatment, including laser photocoagulation (LP) and laser vitreolysis (LV), for vitreoretinal adhesion bands. Material and Methods. A total of forty-two patients (42 eyes) with fibroplastic changes were treated. Laser interventions were performed in two stages: 1) laser photocoagulation of the retina, in sites where the bands attached the retina, followed by 2) neodymium-doped yttrium aluminum garnet (Nd:YAG) laser vitreolysis. Accurate focusing and adjusting the optimal laser energy contribute to increased treatment efficacy. Results. At the first stage, 36 patients (86%) were performed preventive LP of newly-formed vessels of the bands and limiting LP in the sites of attachment of the bands and membranes. LP was made in the basement of the vitreoretinal bands in the sites where tractional retinal detachment could occur. At 2-3 weeks, after chorioretinal comissura had been formed, Nd:YAG LV was performed. On treatment completion, visual acuity increased by 27% in 28 patients (67%). In addition, the level of intraocular pressure almost did not change (20.0 mm Hg). The present treatment managed to dissect the vitreoretinal adhesion bands and to decrease a degree of traction in 38 patients (67%). Conclusion. The studies showed a high efficacy of a two-stage laser treatment for vitreoretinal adhesion bands which, in certain cases, can be alternative to surgical treatment, vitrectomy and endolaser photocoagulation. Keywords: proliferative vitreoretinopathy, laser photocoagulation, Nd-Yag laser vitreolysis Background Hemorrhage and exudates as a consequence of ocular trauma or uveitis can lead to fibrous proliferation with vitreous adhesion bands and membranes which induce retinal deformation and traction. The frequency of retinal detachment in patients with proliferative vitreoretinopathy ranges from 5.1 to 11.7% [6]. Since medicinal treatment is of low-efficiency nowadays, vitrectomy with separation or fragmentation of the preretinal proliferating tissue is used in order to prevent from developing tractional retinal detachment. Separation or segmentation of vitreous adhesions is an important and difficult task when performing a surgical intervention in the vitreous. Surgery is challenging when performing it in patients with high visual function, transparent lenses, and single vitreous adhesions as well as at risk of hemorrhages. Fibroplastic changes in the vitreous with the presence of vitreoretinal adhesions traditioanally require a two-stage treatment including pars plana vitrectomy and endolaser photocoagulation. However, complications, including cataract, secondary glaucoma, hemorrhages, and recurrent retinal detachment, are observed in 15-46% cases of vitrectomy [2]. Based on literature sources, laser interventions for fibroblastic changes in the vitreous are divided into two freestanding techniques: laser photocoagulation and laser vitreolysis or fragmentation. With the purpose to flatten vitreous adhesion bands, M.I. Beliaieva (2009) recommends performing laser photocoagulation of their surface [1]. In our opinion, however, such operation will result not only in the flattening but in the shrinking and shortening of the vitreous adhesion bands, which can provoke retinal detachment. Some authors have shown that Nd:YAG or Er:YAG laser vitreolysis and fragmentation for vitreous opacities can be used as an independent method of treatment [3, 5]. In the meantime, such manipulations can be connected to a variety of complications including retinal detachment, posterior capsule rupture, and a damage to IOL, so the authors recommend performing such operations very carefully at the distance of 0.5-4.5 mm from the retina [4, 8, 9]. The purpose of the present paper was to determine the efficacy of a two-stage laser treatment, including laser photocoagulation (LP) and laser vitreolysis (LV), for vitreoretinal adhesion bands. Material and Methods A total of forty-two patients (42 eyes) with posttraumatic/uveal fibroplastic changes as vitreoretinal bands and opacities in a shape of flat membranes and masses were treated. The mean age of the patients was 41.7 (SD 16.54); a male/female ratio was 29 (69%) / 13 (31%). At baseline, visual acuity averaged 0.33 (SD 0.25) and ranged from 0.01 to 0.1, from 0.2 to 0.5, and from 0.6 to 1.0 in 13 (31%), 26 (62%), and 3 (7%) eyes, respectively. A level of intraocular pressure (IOP) before treatment averaged 18.5 (SD 1.38) mm Hg ranging from 16.0 to 21.0 mm Hg. Laser interventions were performed in two stages: LP of the retina in sites where the bands attached the retina followed by LV. Selection criteria were the presence of transparency of refractive medium and maximal mydriasis. Retinal LP was performed under topical anesthesia through the Goldman lens using lasers with λ=0.48 and 0.53 µm. Coagulates with a 50-200-μm spot size with a 100-200 µm spacing were made in 3-4 rows in the checkerboard order. Laser power was defined by a state of refractive media of the eye, location, and a pigmentation degree and ranged from 200 to 700 mW with an exposure of 0.15 s. The diameter of laser irradiation was minimal in the macular zone, medium in the paramacular zone, and maximal in the periphery. LV or segmentation of membrane formations using Nd:YAG laser with λ=1.06 µm was performed 2-3 weeks later as the second stage. LV was also carried out under topical epibulbar anesthesia through the Goldman lens with a targeted action precisely focused on the object, greater than 1.0 mm from the retina and the anterior capsule/IOL. Pulse energy ranged from 1.2 to 3.5 mJ. Precise focusing, adapting a contact lens, and adjusting the optimal laser energy contribute to treatment efficacy and prevent from the damage to substructures of the eye (lens capsules, IOL, retina). The patients were performed visual acuity testing, ophthalmoscopy, IOP measurement, ultrasound scanning, and color imaging before and after each stage of laser treatment. Results At the first stage, 36 patients (86%) were performed preventive LP of newly-formed vessels of the bands and limiting sequential LP in the sites of attachment of the bands, membranes, folds, or retinal detachment in order to create the lines of demarcation. LP was made in the basement of the vitreoretinal bands in the sites where tractional retinal detachment could occur. At 2-3 weeks, after chorioretinal comissura had been formed, Nd:YAG VL or segmentation of membrane formations was performed. The sequence of the interventions made it possible to avoid increasing the area of retinal detachment which could occur in LV as a result of hydrodynamic shock. As a treatment result, 38 patients (90%) were managed to dissect vitreoretinal adhesion bands and to decrease a degree of traction, which was clinically expressed as a flattening and partial attachment of the retina. At the moment of LV, in three cases (7%) there were insignificant hemorrhages from the newly-formed vessels located in the body of the bands; they, though, dissolved within 3-5 days. In the presence of small, ‘fresh’, local retinal detachments, the retina was completely attached in 10 patients (24%). On treatment completion, visual acuity significantly increased in 28 patients (67%) by 27% to 0.42 (SD 0.25), (р<0.0001) (Fig. 1, Table 1.).
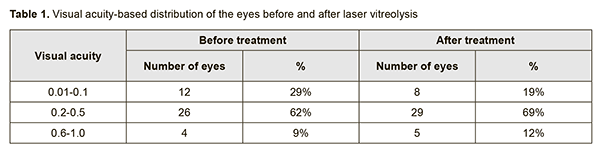
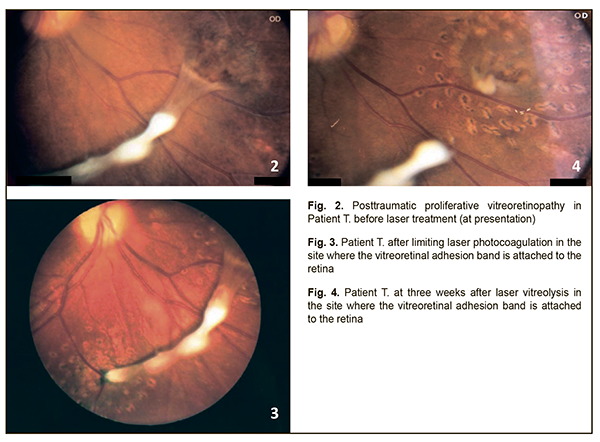
In the meanwhile, a level of IOP did not change significantly and averaged 20.0 (SD 1.13) mm Hg ranging from 18.0 to 22.0 mm Hg. On laser vitreolysis completion and retinal attachment achievement, laser coagulation was repeated; however, this time, it was delivered closer to the center of band attachment site. In four patients (10%), it was impossible to completely dissect the vitreoredinal adhesion bands due to their high density and fibrous thickness; so those patients were performed vitrectomy. The studies showed a high efficacy of a two-stage laser treatment for vitreoretinal adhesion bands which can be alternative to surgical treatment (vitrectomy and endolaser photocoagulation) in certain cases. A clinical case Patient T., aged 45 y/o, applied to SI “The Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine” at 10 months after trauma and a course of medicinal treatment, performed at place of residence, for blunt injury of the right eye and subtotal hemophthalmos. Diagnosis at presentation: OD – proliferative vitreoretinopathy VIS OD = 0.1 (uncorrected); VIS OS = 1.0; IOP OD = 21.0 mm Hg; IOP OS = 17.0 mm Hg Ophthalmoscopy of the right eye in the macular zone at the end site of the adhesion band revealed the elevation and traction of the retina with thinned retinal portions (Fig. 2).
The patient was performed limiting LP in the sites where the adhesion bands attached the retina (in the macular area and, two weeks later, under the optic disk) (Fig. 3). Pigmented laser exposure areas were formed. Three weeks later, the patient was performed LV in the macular zone and the end site of the band (Fig. 4). Having been dissected in the end site, the vitreoretinal band shortened. The retina was attached. No traction signs were observed. VIS OD = 0.2 (uncorrected); VIS OS = 1.0; IOP OD = 19.0 mm Hg; IOP OS = 17.0 mm Hg Thus, LV is a pathogenic treatment since it removes the obstacle for retinal attachment. Our findings are consistent with those of foreign investigators, Liu X.Y. et al., who have also shown the flexibility of Nd:YAG laser for accurate dissection and tissue removal in vitreoretinal manipulations with high-grade security [7]. The main disadvantage is the need for manipulation in immediate proximity to the retina. Our experience of many years has shown a high efficacy of a two-stage laser treatment for vitreoretinal adhesion bands in patients with fibroplastic changes of the vitreous humor. The present treatment resulted in the fact that 38 patients (90%) were managed to dissect the vitreoretinal adhesion bands and to decrease the degree of traction, which was evidenced by the flattened and partially-attached retina. Only in 4 patients (10%), it was impossible to completely dissect the bands due to their high density and fibrous thickness. In 10 patients (24%), in the presence of small ‘fresh’ local retinal detachment, the retina was completely attached. On treatment completion, visual acuity increased in 28 patients (67%) to 0.42 (SD 0.25), (р<0.0001). The IOP level was stable. No complications were observed during the laser interventions. Conclusion
The studies showed a high efficacy of a two-stage laser treatment for vitreoretinal adhesion bands which, in certain cases, can be alternative to surgical treatment, vitrectomy and endolaser photocoagulation.
References
|