J.ophthalmol.(Ukraine).2018;3:41-51.
|
https://doi.org/10.31288/oftalmolzh201834151 Comparing bioelectrical activity of the peripheral retina among myopic patients operated for rhegmatogenous retinal detachment complicated by choroidal detachment Alibet Yassine, Ophthalmologist, Postgraduate Student, V.S. Ponomarchuk, Dr Sc (Med), Prof., G.V. Levytska, Cand Sc (Med), N.I. Khramenko, Cand Sc (Med) Filatov Institute of Eye Disease and Tissue Therapy; Odessa (Ukraine) E-mail: alibet.yassine@gmail.com TO CITE THIS ARTICLE: Аlibet Yassine, Ponomarchuk VS, Levytska GV, Khramenko NI. Comparing bioelectrical activity of the peripheral retina among myopic patients operated for rhegmatogenous retinal detachment complicated by choroidal detachment. J.ophthalmol.(Ukraine).2018;3:41-51. https://doi.org/10.31288/oftalmolzh201834151
Background: High myopia is known to be a major risk factor for the development of choroidal detachment (CD) in eyes with rhegmatogenous retinal detachment (RRD). Trophic disturbances of the retina in axial myopia have been previously confirmed by electroretinography (ERG) data, and are likely to play an important role in the pathogenesis of RRD complicated by CD. To the best of our knowledge, no study has examined in detail the ERG in myopic patients operated for RRD combined with CD. Purpose: 1) To investigate the bioelectrical activity of the peripheral retina after successful surgery for combined RRD and CD in patients differing in the degree of myopia, and 2) to compare the characteristics with those of normal eyes and myopic patients successfully operated for uncomplicated RRD. Materials and Methods: Fifty two patients (52 eyes) were included into the study 3 months after undergoing a single successful vitrectomy with gas tamponade, either for uncomplicated RRD (32 eyes), or combined RRD and CD (20 eyes). They were divided into four groups: Groups 1 and 2 (moderate and high myopes after surgery for uncomplicated RRD; 21 and 11 patients, respectively), and Groups 3 and 4 (moderate and high myopes after surgery for combined RRD and CD; 9 and 11 patients, respectively). Fourteen age-matched individuals (28 eyes) without any ocular or systemic disease were enrolled as controls (Group 5). Scotopic rod response, scotopic combined rod-cone response, and scotopic oscillatory potentials (OPs) were recorded to examine the bioelectrical activity of the peripheral retina. Results: The b-wave amplitude of scotopic rod-mediated response (the summed response of the midperipheral retinal layers to a weak flash arising from the rods in the dark-adapted eye) in myopic eyes in Groups 3 and 4 was 12-fold lower than in normal eyes, 4.3- to 8.8-fold lower than in the fellow eye, and 2.9- to 8.4-fold lower than in myopic eyes in Groups 1 and 2. In addition, the a-wave amplitude (the response of the peripheral retinal photoreceptors) in myopic eyes in Groups 1 and 3 was 1.8-fold lower than in normal eyes, and in highly myopic eyes, 3.4-fold lower than in normal eyes. The b-wave amplitude of scotopic combined rod-cone response (representing the activity of the midperipheral retinal layers) in Groups 3 and 4 was 2.5-fold and 7.5-fold lower, respectively, than in normal eyes, and 1.5-fold and 4.4-fold lower, respectively, than in the fellow eye, and 1.87-fold lower than in myopic eyes in Groups 1 and 2. The OP amplitude in myopic eyes in Groups 3 and 4 was 8.2-fold lower than in normal eyes, 4-fold lower than in the fellow eye, and 2.6- to 5.5-fold lower than in myopic eyes myopic eyes in Groups 1 and 2. The b-wave implicit time of scotopic combined rod-cone response in myopic eyes in Groups 1 to 4 was 19.9% (p < 0.05) longer than in normal eyes. In addition, myopic eyes in Groups 1 to 4 had similar a-wave implicit time compared with normal eyes. We found direct correlations between BCVA and b-wave and a-wave amplitudes of the scotopic rod-mediated response ERG (r = 0.59 and r = 0.67, respectively), b-wave amplitude of the scotopic combined rod-cone response ERG (r = 0.5), and OP amplitude (r = 0.62), and an inverse correlation (r=-0.63) between BCVA and b-wave implicit time for the scotopic combined rod-cone response ERG in myopic patients after surgery for combined RRD and CD. Conclusion: In myopic patients after surgery for combined RRD and CD, the bioelectrical activity of the peripheral retina was found to be low
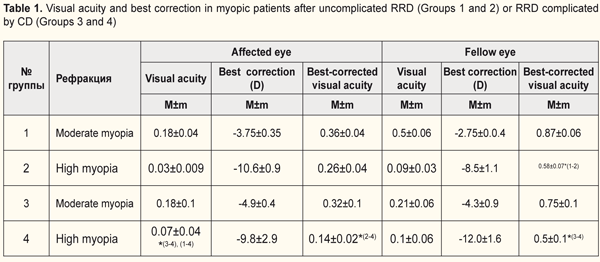
Keywords: rhegmatogenous retinal detachment, choroidal detachment, myopia, electroretinography Introduction It is generally accepted that rhegmatogenous retinal detachment (RRD), when complicated by choroidal detachment (CD), has an especially unfavorable prognosis [1-3], with clinically apparent intraocular inflammation being a feature of the disease [4, 5]. RRD is a degenerative disease with clinical signs of retinal hypoxia, which even if uncomplicated, is associated with expression of inflammatory mediators in ocular tissues and fluids [6]. Compared with the patients with uncomplicated RRD, cytokines, chemokines, and growth factors in patients with combined RRD and CD have been found significantly up-regulated [7], possibly due to a difference in baseline levels of trophic disturbances. It is, however, possible that, in the presence of RRD, it is the eyes that are morphologically predisposed to the complication (i.e., those in which early degenerative changes are more apparent) where choroidal detachments might develop. Our hypothesis on apparent trophic disturbances of the retina in patients with combined RRD and CD is substantiated by the following. Combined RRD and CD are known to occur more often in highly myopic eyes [8]. Trophic disturbances of the retina in axial myopia have been confirmed by electroretinogram (ERG) studies [9]. High prevalence of high myopia [10, 11] and high frequency of combined RRD and CD (up to 18.9% of all cases with RRD) in Chinese population versus 0.5-4.5% in European populations [8, 12-14] illustrate this relationship. Given the above, investigation of the degree of trophic disturbance in the retina in patients with combined RRD and CD would contribute to the body of knowledge on the pathogenesis of this specific form of retinal detachment. The purpose of this study was 1) to investigate the bioelectrical activity of the peripheral retina after successful surgery for combined RRD and CD in patients differing in the degree of myopia, and 2) to compare the characteristics with those of normal eyes and myopic patients successfully operated for uncomplicated RRD. Materials and Methods Fifty two patients (52 eyes) were included into the study 3 months after undergoing a single successful procedure, either for uncomplicated RRD (32 patients, 32 eyes), or combined RRD and CD (20 patients, 20 eyes). They were divided into four groups: Groups 1 and 2 (moderate and high myopes after surgery for uncomplicated RRD; 21 and 11 patients, respectively), and Groups 3 and 4 (moderate and high myopes after surgery for combined RRD and CD; 9 and 11 patients, respectively). Patients with uncomplicated RRD were comparable with those with combined RRD and CD with regard to period of detachment (19.2±8.3 days vs 17.5±13.2 days), type of surgery (vitrectomy, retinal laser photocoagulation, and perfluoropropane tamponade) and age (53.8±17 years). Operated eyes demonstrated a refractive error that was comparable to the fellow eyes, and peripheral retinal degeneration was observed in both the operated and fellow eyes. Fourteen individuals (28 eyes) without any ocular or systemtic disease were enrolled as controls (Group 5). Exclusion criteria were history of previous vitreoretinal surgery, ocular trauma, glaucoma, age-related macular degeneration, epi- or submacular membrane, macular tear, diabetic or vascular retinal disorders. Operated and fellow eyes were assessed for bioelectric retinal activity. A full field (Ganzfeld) ERG examination was performed using electrophysiological test unit Retiscan according to ISCEV Standard ERG protocols [15], which included scotoptic rod response, scotopic combined rod–cone response and scotopic oscillatory potentials. Pupils were dilated, and skin reference electrodes (of < 5 kOhm impedance) were placed near the orbital rim. Thereafter, the patient underwent dark adaptation for 20 minutes, 2-3 anesthetic eye drops were administered topically, and the contact lens electrode was placed on the eye. The responses were evoked by flashes of different intensities and durations, and with different numbers of flash stimuli per session, as per ISCEV Standard ERG protocols [15]. Data base development and analysis was performed using Statistica 10.0 (StatSoft, Tulsa, OK, USA) software. Distributions were tested for normality using histogram plots and the Kolmogorov-Smirnov test. The parametric Student's t test was used to determine significant differences between two normally distributed samples. Wilcoxon signed-rank test and Mann-Whitney U test were used for the comparison of two samples when the underlying distributions were not normal. Non-parametric Spearman correlation coefficient (rs) was used to determine the linear relationship between the variables. Results There was no difference between the two groups of moderate myopes (Group 1 and Group 3) and between the two groups of high myopes (Group 2 and Group 4) with regard to uncorrected visual acuity (UCVA) in the affected eye (0.18±0.09 and 0.04±0.01, respectively; Table 1). In addition, there was no difference between the two groups of moderate myopes with regard to best-corrected visual acuity (BCVA; 0.34±0.09). There was, however, a significant difference between the two groups of high myopes (Group 2 and Group 4), with regard to BCVA in the affected eye (0.26±0.04 vs 0.14±0.02, p < 0.05). Therefore, in patients who had undergone surgery for either RRD alone or combined RRD and CD, the BCVA in the affected eye was lower than normal, and depended on the refractive error, and on whether the patient had a history of RRD alone or combined RRD and CD. The BCVA in the affected eye in Group 4 was 46% lower (p = 0.04) than in Group 2, and 61% lower than in moderate myopes of Groups 1 and 3.
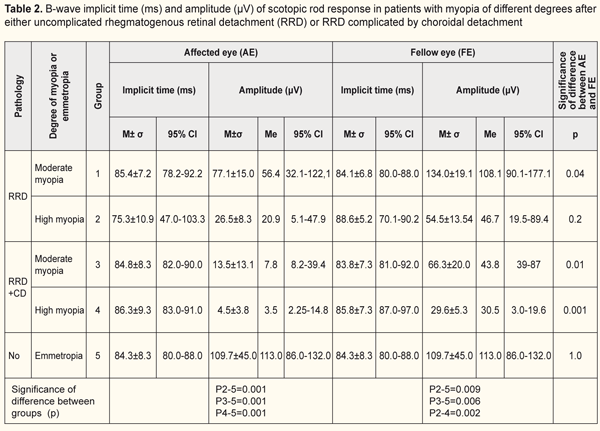
The BCVA in the fellow eye in moderate myopes of Group 1 was 0.87±0.06, which was 33% higher than in high myopes of Group 2 (0.58±0.07, p < 0.05). There was no significant difference in the BCVA in the fellow eye between patients who had undergone surgery for combined RRD and CD (Groups 3 and 4) and those who had undergone surgery for RRD only (Groups 1 and 2; Table 1). Next, we examined a b-wave of the scotopic rod response for the ERG to a dark-adapted eye, which is a combined response arising from bipolar rod cells and Müller cells of the peripheral retina (Table 2).
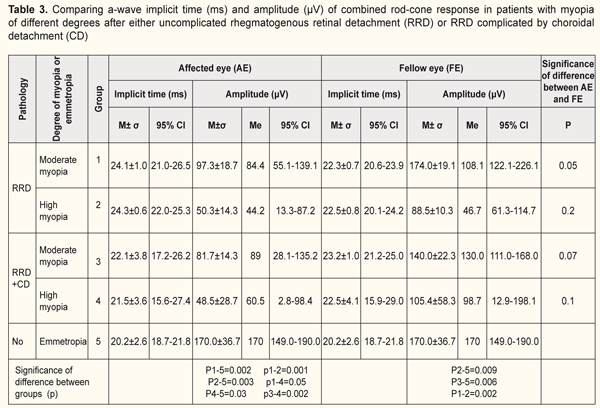
It should be noted that, since only one moderate myope that had undergone surgery for combined RRD and CD underwent ERG examination, this case was not included in the analysis. However, his affected eye demonstrated decreased bioelectrical activity. There was no difference in b-wave implicit time for the scotopic flash ERG in the affected eye between the groups. In addition, there was no difference in this parameter between the affected eye and the fellow eye. The median b-wave implicit time for the five groups was 85.4± 2.5 ms. In the ERGs to a weak flash arising from the rods in the dark-adapted eye, b-wave amplitudes were found to differ between study groups (Table 2). The mean b-wave amplitude in the control group was 109.7±45.0 μV (median value, 113.0 μV; 95% CI, 86.0 μV to 132.0 μV). All non-control groups had significantly lower b-wave amplitudes than controls. Thus, in moderate and high myopes who had undergone surgery for uncomplicated RRD, the b-wave amplitude was 2.1-fold lower (median, 56.4 μV) and 4.4-fold lower (median, 20.9 μV), respectively, than in controls (p < 0.05). In moderately and highly myopic eyes that had undergone surgery for RRD complicated by CD, the b-wave amplitude was the lowest compared to normal eyes, and was 12-fold lower compared to normal eyes (95% CI, 2.5 μV to 39.4 μV; p = 0.001). Therefore, examination of the bioelectrical activity of the peripheral retina in the affected eye based on the b-wave amplitude demonstrated that the most severe damage to retinal function was found in Groups 3 and 4 (Table 2). In these groups, the median b-wave amplitude was 9.4 μV, which was 2.9-fold lower (p = 0.003) than in Group 2 (high myopes who had undergone surgery for uncomplicated RRD), and 8.4-fold lower (p = 0.0001) than in Group 1 (moderate myopes who had undergone surgery for uncomplicated RRD). It is interesting that, compared with the fellow eye, the b-wave amplitude in the affected eye in Group 1 was two-fold lower (p = 0.04), and in Group 2 was not significantly different. In addition, in moderate and high myopes who had undergone surgery for RRD complicated by CD, the b-wave amplitude in the affected eye was 4.3-fold lower (p = 0.01), and 8.8-fold lower (p = 0.001), compared with the fellow eye (Table 2). We found a direct correlation (r=0.5; p < 0.05) between BCVA and b-wave amplitude of the peripheral retina in the affected eye. The scotopic combined rod-cone response ERG reflects the functional activity of the outer and midretinal layers (the photoreceptors of rods and cones, and the relevant bipolar cells and Muller cells), presumably from the peripheral retina. In the scotopic combined rod-cone response ERG, the negative a-wave arises from the photoreceptors (i.e., the photopic and scotopic system composed of cones and rods) [16], and is characterized by a time-relevant parameter, latency or implicit time (milliseconds) and composite bioelectrical parameter, amplitude (microvolts). According to the convention, the a-wave amplitude is measured from the average, pre-stimulus baseline to the a-wave trough, and the implicit time is measured from the time of the flash to the peak of the wave [17]. In all postoperative patient groups, a-wave amplitude, but not a-wave implicit time was significantly different from that in controls, and the median a-wave implicit time was 22.4 ± 2.6 ms (Table 3).
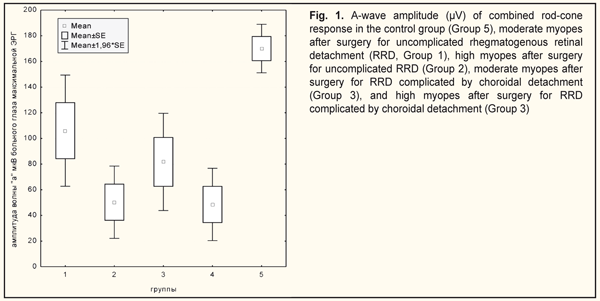
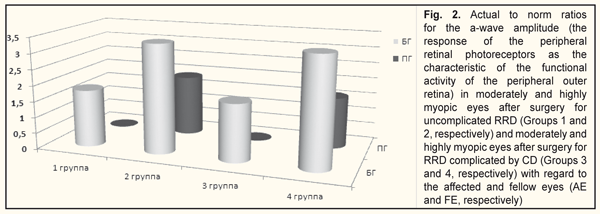
Compared to controls (170.0±36.7 μV), the a-wave amplitude in moderate myopes and high myopes who had undergone surgery for uncomplicated RRD was 1.75-fold lower (p = 0.002) and 3.4-fold lower (p = 0.003), respectively. Therefore, in the former myopes, this characteristic was 1.9 higher than in the latter myopes, and this difference was significant (p = 0.001). Compared to controls, the a-wave amplitude in moderate myopes and high myopes who had undergone surgery for RRD complicated by CD was 2.0-fold lower (81.7±14.3 μV; p = 0.002) and 3.4-fold lower (p = 0.003), respectively (Table 3). Therefore, in the former myopes, this characteristic was 1.7 higher than in the latter myopes, and this difference was significant (p = 0.002; Fig. 1; Table 2).
In all postoperative patient groups, functional activity of photoreceptors (assessed through the a-wave amplitude) was significantly lower than in controls. The changes seen in postoperative high myopes were more apparent (with the a-wave amplitude being 1.7-1.9 lower) than in moderate myopes (Fig. 2), and the presence of CD in the history had no influence on the state of photoreceptors.
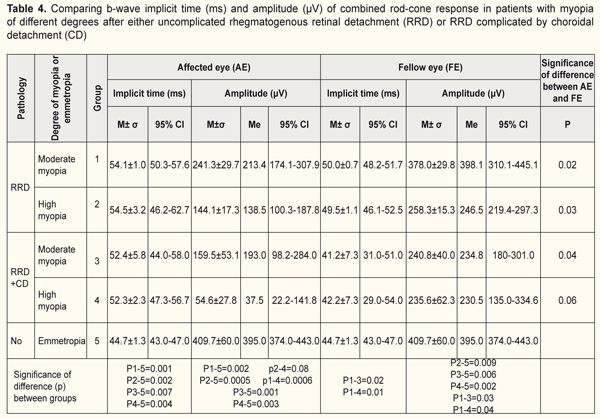
Therefore, the a-wave amplitude reflects the functional state of photoreceptors, and compared to controls, its values in high myopes after surgery for either uncomplicated RRD or RRD combined with CD were 3.4-fold lower, whereas in moderate myopes after surgery for either uncomplicated RRD or RRD combined with CD were 1.9-fold and 1.7-fold lower, respectively. We found a direct correlation (r=0.67; p < 0.05) between BCVA and a-wave amplitude in the scotopic combined rod-cone response ERG for the affected eye. In the scotopic combined rod-cone response ERG, the positive b-wave arises from bipolar cells and Muller cells of the midperipheral retina [18], and its amplitude and implicit times are measured from a-wave trough to b-wave peak and from the time of the flash to the peak of the wave [17], respectively. In all postoperative patient groups, b-wave implicit time of the scotopic combined rod-cone response ERG was significantly different from that in controls (44.7 ± 1.3 ms). There was no significant difference in b-wave implicit time between postoperative patient groups with the median value being 53.6±1.2 ms, which was 19.9% (p < 0.05) longer than in controls. Therefore, irrespective of the refractive error, the b-wave implicit time for the combined response ERG in the affected eye of patients who had undergone surgery for uncomplicated RRD or RRD complicated by CD was longer than in controls (Table 4). We found an inverse correlation (r=-0.63; p < 0.05) between BCVA and b-wave implicit time for the scotopic combined rod-cone response ERG in the affected eye.
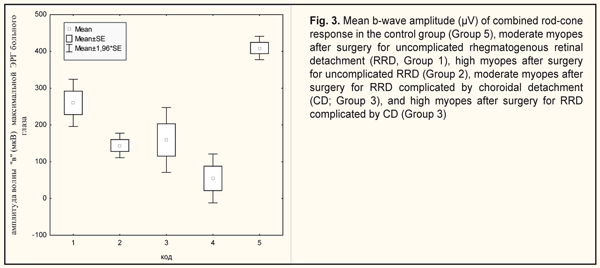
In all postoperative patient groups, b-wave amplitude for the combined response ERG in the affected eye was also significantly different from that in controls. Compared to controls (409.7±60.0 μV; 95% CI, 374 μV to 443 μV; Table 4; Fig. 3), this characteristic in moderate and high myopes who had undergone surgery for uncomplicated RRD was 1.7-fold lower (p = 0.002; 241.3±29.7 μV; Group 1) and 2.84-fold lower (p = 0.0005; 144.1±17.3 μV; Group 2), respectively. In moderate and high myopes who had undergone surgery for RRD complicated by CD, b-wave amplitude for the combined response ERG in the affected eye was 159.5±53.0 μV, and 54.6±27.8 μV, respectively. No statistically significant differences in b-wave amplitude for the combined response ERG in the affected eye was found between these groups due to a high intragroup variation in this characteristic (100%; 98 to 284 μV for Group 3 and 124%; 22 to 141 μV for Group 4). The median b-wave amplitude for the combined response ERG in the affected eye for groups 3 and 4 was 112±90 μV. Compared to moderate (Group 1) and high myopes (Group 2) who had undergone surgery for unncomplicated RRD, b-wave amplitude for the combined response ERG in the affected eye in high myopes who had undergone surgery for RRD complicated by CD (Group 4) was 4.5-fold lower (p = 0.0006) and 2.7-fold lower (p = 0.08), respectively (Table 4). The median value for Groups 1 and 2 (210±90 μV) was 1.87-fold lower than that for Groups 3 and 4 (112±90 μV; p = 0.008).
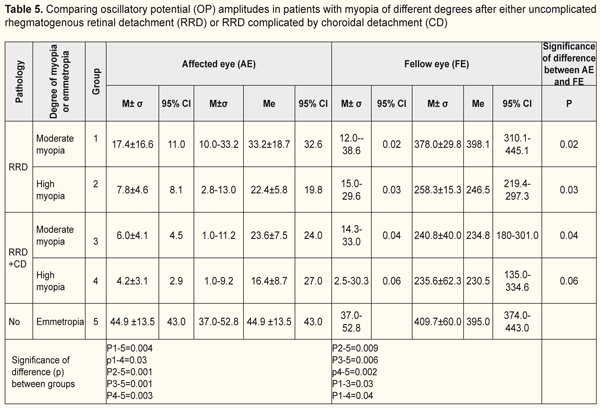
Therefore, in moderate and high myopes who had undergone surgery for RRD complicated by CD (Groups 3+4), median bioelectrical midretinal activity with regard to b-wave amplitude for the scotopic combined rod-cone response ERG in the affected eye was 1.87 lower than that in those who had undergone surgery for uncomplicated RRD (Groups 1+2) (p < 0.05), and 3.7 lower than the norm. We found a direct correlation (r=0.66; p < 0.05) between BCVA and b-wave amplitude for the scotopic combined rod-cone response ERG in the affected eye. In addition, we found that, in high myopes who had undergone surgery for uncomplicated RRD, and in moderate and high myopes who had undergone surgery for RRD complicated by CD, median b-wave amplitude for the combined response ERG in the fellow eye was 1.7 lower than the norm. Furthermore, in Groups 1, 2, 3 and 4, b-wave amplitude for the combined response ERG in the fellow eye was 1.6, 1.8, 1.5, and 4.4-fold lower, respectively, than that in the affected eye (Table 4). Median b-wave implicit time for the combined response ERG in the affected eye in Groups 1 to 4 was 19.9% longer than the norm (p < 0.05). Median b-wave amplitude for the combined response ERG in Groups 1 and 2 was 1.7 and 2.8-fold lower, respectively, than the norm (p < 0.05). In addition, median b-wave amplitude for the combined response ERG in Groups 3 and 4 was 1.87-fold lower, than that in Groups 1 and 2, and 3.7 lower than the norm (p < 0.05). Oscillatory potentials A group (3 – 5) of small high-frequency waves may be detected on the ascending limb of the b-wave of normal human ERG and they are known as oscillatory potentials (OPs). They represent interactions between inner retinal cells, including amacrine cells [17]. In addition, OPs indirectly reflect the state of retinal trophism [17], and reduced amplitude of OPs characterizes the ischemia of the internal retina [19]. The OP amplitude is measured from the baseline to the peak of the OP. Mean OP amplitude in Groups 1 and 2 was 17.4±16.6 μV and 7.8±4.6 μV, respectively, which was 2.6-fold (p = 0.004) and 5.6-fold (p = 0.001) lower, respectively, compared to controls (44.9 ±13.5 μV) (Table 5).
There was no significant difference in OP amplitude between moderate and high myopes who had undergone surgery for RRD complicated by CD, with the median value being 5.23±3.6 μV, which was 8.2-fold lower compared to controls (p = 0.001). Moderate myopes who had undergone surgery for RRD complicated by CD exhibited a 4-fold decrease in OP amplitude (p = 0.01) compared to the fellow eye. However, the difference in OP amplitude between the affected and fellow eyes in Group 4 was insignificant due to highly variable data (Table 5). We found a direct correlation (r=0.626; p < 0.05) between BCVA and OP amplitude in the affected eye. When comparing the operated eyes of Group 4 with those of Group 1, the OP amplitude was reduced 4.25-fold (p = 0.03). When comparing the groups for differences in OP amplitude between the affected and fellow eyes, the greatest difference (a 4-fold reduction; p = 0.04) was found in moderate and high myopes who had undergone surgery for RRD complicated by CD, and the lowest (a 1.9-fold reduction; p = 0.02) in moderate myopes who had undergone surgery for uncomplicated RRD. Discussion A retinal detachment is a separation of the neurosensory retina from the retinal pigment epithelium, a serious condition that can lead to blindness [20]. Photoreceptors, the outer nuclear layer and the outer plexiform layer obtain oxygen and nutrients from the choriocapillaris choriocapillary network; a retinal detachment causes the development of the ischemic process in these layers. The damage may spread to the inner retinal layers due to raised intraocular pressure and/or impaired retinal autoregulation [21]. According to Azarmina and colleagues [20], a steady improvement in the bioelectrical activity of retinal components occurs as early as 3 months after retinal re-attachment surgery, and this improvement remains stable at the 6 month follow-up visit. The authors refer to a number of experimental studies in which it has been demonstrated that photoreceptor ultrastructure recovers completely one month after re-attachment surgery [22]. Following reattachment, the ultrastructural relationship between the photoreceptors and the RPE is re-established, but it does not return to the predetachment state even after short detachment episodes coupled with prolonged recovery periods. All of the reattached retinae show some degree of abnormality, ranging from subtle changes in photoreceptor ultrastructure to dramatic degenerative effects in the outer retina. Photoreceptor recovery varies widely between adjacent regions within the same retina. In some retinae, recovery in cones is inferior to that in rods [23]. Parallelism in improvement of retinal and visual function after re-attachment surgery is deemed to be important. A number of factors can compromise the recovery process. This is related, in particular, to the conditions with the initial malnutrition of retinal cells, e.g., due to pathological myopia, where a reduced blood volume in the eye is commonly observed [24]. Westall and co-authors reported a linear reduction in the logarithmic transform of ERG amplitude with increasing axial length [9]. A choroidal detachment contributes to a significantly impaired retinal nutrition, with a subsequent insufficient improvement in photoreceptor and visual function after anatomically successful re-attachment surgery. The occurrence of CD in eyes with primary RRD is relatively uncommon (2%-4.5% [3] to 8.6% [8]). Longer axial length is a risk factor, along with the location of the retinal breaks, and the extent of retinal detachment [8]. That is why in this paper we give particular attention to the analysis of retinal function in the eyes with different degrees of myopia which underwent anatomically successful re-attachment surgery for combined RRD and CD. We found that myopic eyes that underwent surgery for either RRD only or combined RRD and CD had similar a-wave implicit time compared with normal eyes, but, irrespective of the degree of myopia and whether they underwent surgery for either RRD only or combined RRD and CD, their median b-wave implicit time was 19.9% (p < 0.05) longer than in controls. It has reported that implicit time of the ERG response from the intact retina did not change with an increase in axial length [9]. Regeneration of photoreceptor outer segments and restoration of the anatomical relationship between the neurosensory retina and the RPE may explain recovery of retinal function after retinal reattachment [25]. In the current study, the a-wave amplitude of the scotopic combined rod-cone response ERG, which reflects the activity of the peripheral retina photoreceptor layer, was 1.8-fold lower in highly myopic eyes that underwent surgery for either RRD only or combined RRD and CD, than in moderately myopic eyes that underwent surgery for either RRD only or combined RRD and CD. Iin moderate and high myopes who had undergone surgery for RRD complicated by CD (Groups 3+4), median bioelectrical midretinal activity with regard to b-wave amplitude for the scotopic combined rod-cone response ERG in the affected eye was 1.87 lower than that in those who had undergone surgery for uncomplicated RRD (Groups 1+2) (p < 0.05), and 3.7 lower than the norm. According to Gong et al. [26], the amplitude of the scotopic b wave in operated eyes was 58.1% of the control eyes. In our study, the amplitude of the scotopic b wave in myopic eyes that had undergone surgery for combined RRD and CD was 12-fold lower compared to normal eyes. Function and trophism of the inner peripheral retina was least disturbed in moderately myopic eyes after surgery for uncomplicated RRD, and most disturbed in highly and moderately myopic eyes after surgery for RRD complicated by CD (with a 8.2-fold lower OP amplitude than in normal eyes). Therefore, outer retinal photoreceptor function was more impaired in highly myopic eyes after surgery for either uncomplicated RRD or RRD combined with CD (with the a-wave amplitude 3.4-fold lower than in controls), whereas midretinal function was more impaired in myopic eyes after surgery for RRD combined with CD (with the b-wave amplitude 3.7- to 12-fold lower than in controls), which provides evidence on the severity and depth of ischemia in CD. In addition, there were correlations of BCVA with amplitudes of responses from photoreceptors, midperipheral retina, as well as amacrine cells of the peripheral retina. Our findings are in agreement with those of Azarmina et al. [20], who demonstrated that BCVA improvement occurs in parallel with improvement in ERG response. Therefore, in the presence of anatomical retinal reattachment, the functional outcome was affected by the presence of myopia and choroidal detachment, which is likely to be associated with severe retinal ischemia. Conclusion First, the b-wave amplitude of scotopic rod-mediated response (the summed response of the midperipheral retinal layers to a weak flash arising from the rods in the dark-adapted eye) in myopic eyes after surgery for combined RRD and CD was 12-fold lower than in normal eyes, 4.3- to 8.8-fold lower than in the fellow eye, and 2.9- to 8.4-fold lower than in myopic eyes after surgery for uncomplicated RRD. Second, the a-wave amplitude of scotopic combined rod-cone response (the response of the peripheral retinal photoreceptors) in moderately myopic eyes after surgery for either uncomplicated RRD or combined RRD and CD was 1.8-fold lower than in normal eyes, and in highly myopic eyes, 3.4-fold lower than in normal eyes. In addition, the b-wave amplitude of scotopic combined rod-cone response (representing the activity of the midperipheral retinal layers) in moderately and highly myopic eyes after surgery for combined RRD and CD was 2.5-fold and 7.5-fold lower, respectively, than in normal eyes, and 1.5-fold and 4.4-fold lower, respectively, than in the fellow eye, and 1.87-fold lower than in myopic eyes after surgery for uncomplicated RRD. Third, OP amplitude (that reflects the function of amacrine cells and the trophism of the inner retinal layers) in moderately and highly myopic eyes after surgery for combined RRD and CD was 8.2-fold than in normal eyes, 4-fold lower than in the fellow eye, and 2.6- to 5.5-fold lower than in myopic eyes after surgery for uncomplicated RRD. Fourth, b-wave implicit time of scotopic combined rod-cone response in all myopic eyes after surgery for either uncomplicated RRD or combined RRD and CD was 19.9% (p < 0.05) longer than in normal eyes. In addition, myopic eyes that underwent surgery for either uncomplicated RRD or combined RRD and CD had similar a-wave implicit time compared with normal eyes. Finally, we found direct correlations between BCVA and characteristics of electric retinal activity like b-wave amplitude of scotopic rod-mediated response ERG (r = 0.59), a-wave amplitude of the scotopic combined rod-cone response ERG (r = 0.67), b-wave amplitude of the scotopic combined rod-cone response ERG (r = 0.5), and OP amplitude (r = 0.62). In addition, we found an inverse correlation (r=-0.63; p < 0.05) between BCVA and b-wave implicit time for the scotopic combined rod-cone response ERG in the affected eye. References 1.Ghoraba HH. Primary vitrectomy for the management of rhegmatogenous retinal detachment associated with choroidal detachment. Graefes Arch Clin Exp Ophthalmol. 2001; 239(10):733-6 2.Sharma T, Gopal L, Badrinath SS. Primary vitrectomy for rhegmatogenous retinal detachment associated with choroidal detachment. Ophthalmology. 1998;105:2282–5 3.Sharma T, Gopal L, Reddy RK, et al. Primary vitrectomy for combined rhegmatogenous retinal detachment and choroidal detachment with or without oral corticosteroids: a pilot study. Retina. 2005; 25: 152–7 4.Alibet Y, Levystka G, Umanets N, Pasyechnikova N, Henrich PB. Ciliary body thickness changes after preoperative anti-inflammatory treatment in rhegmatogenous retinal detachment complicated by choroidal detachment. Graefes Arch Clin Exp Ophthalmol. 2017 Aug;255(8):1503-08 5.Wei Y, Wang N, Chen F, et al. Vitrectomy combined with periocular/intravitreal injection of steroids for rhegmatogenous retinal detachment associated with choroidal detachment. Retina. 2014 Jan;34(1):136-41 6.Levytska GV. [TNF- and VEGF levels in patients differing in severity of rhegmatogenous retinal detachment]. Problemy ekologichnoi ta medychnoi genetyky i klinichnoi imunologii. 2013; 5(119):71–9 Russian 7.Dai Y, Wu Z, Sheng H, et al. Identification of inflammatory mediators in patients with rhegmatogenous retinal detachment associated with choroidal detachment. Mol Vis. 2015; 21:417–27 8.Yajie Yu, Ming An, Bin Mo, et al. Risk factors for choroidal detachment following rhegmatogenous retinal detachment in a chinese population. BMC Ophthalmol. 2016;16:140 9.Westall CA, Dhaliwal HS, Panton CM, et al. Values of electroretinogram responses according to axial length. Doc Ophthalmol. 2001, 102(2): 115–30 10.Kang JH, Park KA, Shin WJ, Kang SW. Macular hole as a risk factor of choroidal detachment in rhegmatogenous retinal detachment. Korean J Ophthalmol. 2008; 22: 100–3 11.Sun J, Zhou J, Zhao P, et al. High prevalence of myopia and high myopia in 5060 Chinese university students in Shanghai. Invest Ophthalmol Vis Sci. 2012; 53:7504–09 12.Li Z, Li Y, Huang X, et al. Quantitative analysis of rhegmatogenous retinal detachment associated with choroidal detachment in Chinese using UBM. Retina. 2012; 32: 2020–5 13.Seelenfreund MH, Kraushar MF, Schepens CL, Freilich DB. Choroidal detachment associated with primary retinal detachment. Arch Ophthalmol. 1974;91(4):254–8 14.Zhu J, Xu X, Zhang X. Surgical therapeutic results of rhegmatogenous retinal detachment associated with choroidal detachment. Zhonghua Yan Ke Za Zhi. 2002 Mar;38(3):135-9 15.Wu De Zheng, Liu Yan. Atlas of testing and clinical application for Roland Electrophysiological Instrument. Beijing: Science and Technology Press. 2006. pp. 5–19 16.Brown KT. The electroretinogram: its components and their origin. Vision Res. 1968;8:633–77 17.Shamshinova AM, Volkov VV. [Functional studies in ophthalmology]. Moscow: Meditsina; 1999. Russian 18.Newman EA, Odette LL. Model of electroretinogram b-wave generation: a test of the K+ hypothesis. J Neurophysiol. 51:164–82 19.Moskowitz A, Hansen RM, Fulton AB. ERG oscillatory potentials in infants. Doc Ophthalmol. 2005 Mar-May; 110(2-3):265-70 20.Azarmina M, Moradian S, Azarmina H. Electroretinographic changes following retinal reattachment surgery. J Ophthalmic Vis Res. 2013 Oct; 8(4): 321–9 21.Kim IT, Ha SM, Yoon KC. Electroretinographic studies in rhegmatogenous retinal detachment before and after reattachment surgery. Korean J Ophthalmol. 2001; 15:118-27 22.Retinal separation, retinotomy, and macular relocation: I. Experimental studies in the rabbit eye. Graefes Arch Clin Exp Ophthalmol. 1993 Nov;231(11):629-34 23.Anderson DH, Guerin CJ, Erickson PA, Stern WH, Fisher SK. Morphological Recovery in the Reattached Retina. Invest Ophthalmol Vis Sci. 1986 Feb;27(2):168-83 24.Ponomarchuk VS, Khramenko NI, Guzun OV. [Outcomes of treating high myopia with laser stimulation and phosphene stimulation]. Oftalmologiia. Vostochnaia Evropa. 2016;4:618-20. Russian 25.Montrone L, Ziccardi L, Stifano G, et al. Regional assessment of cone system function following uncomplicated retinal detachment surgery. Doc Ophthalmol. 2005 Jan;110(1):103-10 26.Gong Y, Wu X, Sun X, Zhang X, Zhu P. Electroretinogram changes after scleral buckling surgery of retinal detachment. Doc Ophthalmol. 2008;117:103–9
|