J.ophthalmol.(Ukraine).2018;3:74-79.
|
https://doi.org/10.31288/oftalmolzh201837479 Changes in the characteristics of superficial electromyography potentials recorded from the horizontal extraocular muscles in children with non-alternating nonaccommodative comitant strabismus after electrical stimulation treatment V.P. Mazur, MD, I.M. Boichuk, Dr Sc (Med) SI "Filatov Institute of Eye Diseases and Tissue Therapy of NAMS of Ukraine; Odessa (Ukraine) E-mail: iryna.ods26@gmail.com TO CITE THIS ARTICLE: Mazur VP, Boichuk IM. Changes in the characteristics of superficial electromyography potentials recorded from the horizontal extraocular muscles in children with non-alternating nonaccommodative comitant strabismus after electrical stimulation treatment. J.ophthalmol.(Ukraine).2018;3:74-79. https://doi.org/10.31288/oftalmolzh201837479
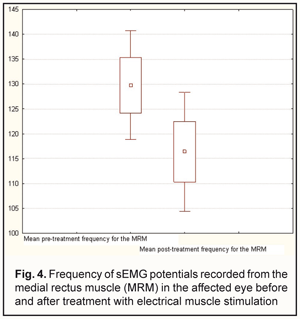
Background: Electrical stimulation of lateral rectus muscles (LRM) is a physiotherapeutic technique used in the management of non-alternating nonaccommodative comitant strabismus (NNCS). Changes in the ocular neuromuscular system after a course of electrical muscle stimulation have never been assessed previously due to the lack of a method for analysis. Purpose: To determine the characteristics of superficial electromyography (sEMG) potentials recorded from the horizontal extraocular muscles in children with NNCS, and 2) to determine the changes in the ocular neuromuscular system with the help of sEMG before and after a course of electric stimulation of the muscles. Materials and Methods: An electromyography recorder (M-TEST-2) was used to examine 60 children (120 eyes) with NNCS in accordance with the methodology that we have reported previously. The Amplipuls-5 apparatus was used for electrical stimulation of LRMs in 8 children with non-alternating nonaccommodative comitant esotropia (NNCES). To this end, we followed the therapeutic regimen proposed by Yurov and Cherikchi. Results: In NNCES, frequency of sEMG potentials recorded from the medial rectus muscle (MRM) was significantly higher both in the esotropic eye and in the non-affected fellow eye compared to normal pediatric eyes (109.29 ± 15.89 Hz vs 58.67±15.97 Hz, р=0.0001 and 53±3.49 Hz vs 58.67±15.97 Hz, р=0.0001, respectively). In addition, in non-alternating nonaccommodative comitant exotropia (NNCEX) , there was a significant difference in frequency of sEMG potentials recorded from the LRM, between the esotropic eye, but not the non-affected fellow eye, and normal pediatric eyes (102.52±14.45 Hz vs 60±18.6 Hz, р=0.0001, and 53.16±10.03 Hz vs 60±18.6 Hz, р=0.0001, respectively). In children with NNCS, we found an improvement in the imbalance between the characteristics of sEMG potentials recorded from the horizontal rectus muscles after a course of electrical stimulation. An electrical-stimulation efficiency criterion was devised based on Кν, the ratio of the frequencies of the sEMG potentials recorded from the antagonist rectus muscles. Conclusion: In NNCES and NNCEX, frequencies of sEMG potentials recorded from the LRM differed between the esotropic eye and normal pediatric eyes, and those from the MRM differed between the exotropic eye and normal pediatric eyes, respectively. In children with NNCES, electrical muscle stimulation treatment resulted in an improvement in the imbalance between the characteristics of sEMG potentials recorded from the LRM and MRM.
Keywords: non-alternating comitant strabismus, electrical stimulation of the extraocular muscles, superficial electromyography potentials
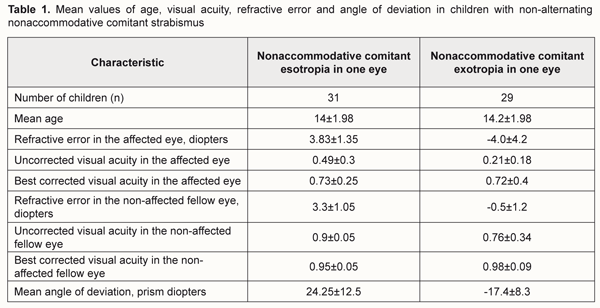
Introduction Strabismus occurs in 0.5-7.1% of children, often disturbs the development of normal visual acuity and binocular vision, and is a substantial cosmetic defect that affects the child’s social development. Alternating strabismus occurs much more often than non-alternating strabismus. In non-alternating nonaccommodative comitant strabismus (NNCS), the affected eye has profoundly reduced visual function compared to the non-affected fellow eye. This is why most ophthalmologists consider only orthoptic and pleoptic or surgical treatment as the first option, but do not consider physiotherapeutic methods at all when managing patients with NNCS. Low awareness of physiotherapeutic approaches for the treatment of strabismus among practitioners may be explained not only by unavailability of proper literature, but also by unavailability of techniques for testing the physiological state of the lateral and medial rectus muscles (LRMs and MRMs, respectively), especially in children, in a non-invasive way. Some features of the ocular neuromuscular system make the electric testing problematic, since the electric current required for determination of apparent deviation of the eye (either from its neutral position, or from the fixation object) significantly exceeds the pain threshold. Changes in the state of the ocular neuromuscular system have been judged also from a coordimetry examination that allows estimating the motor function of the strabismic extraocular muscles. However, the coordimetry method does not allow determining changes in the ocular neuromuscular system after a course of electric muscle stimulation. The purpose of the study was 1) to determine the characteristics of electric potentials of the horizontal extraocular muscles in NNCS, and 2) to determine the changes in the ocular neuromuscular system with the help of superficial electromyography (sEMG) before and after a course of electric stimulation of the muscles. Materials and Methods Thirty-one children (62 eyes) with non-alternating nonaccommodative comitant esotropia (NNCES) and 29 children (58 eyes) with non-alternating nonaccommodative comitant exotropia (NNCEX) underwent examination. The optic media and fundi were normal. Data from history taking and ocular examination were used to classify the type of strabismus. Table 1 shows mean characteristics of the study sample.
An electromyography recorder (M-TEST-2) was used to assess the function of horizontal extraocular muscles in accordance with the methodology that we have reported previously [2, 3]. The SEMG characteristics were recorded in triplicate for each rectus muscle. SEMG amplitude and frequency data was processed automatically using M-TEST-2 software. The Amplipuls-5 apparatus (MAYAK, FGUP (100% state-owned company), Kursk, Russia) was used for electrical stimulation of the horizontal rectus muscles (Fig. 1). We followed the therapeutic regimen proposed by Yurov and Cherikchi [5, 6], with electrical stimulation of the LRM and MRM performed in comitant esotropia and exotropia, respectively.
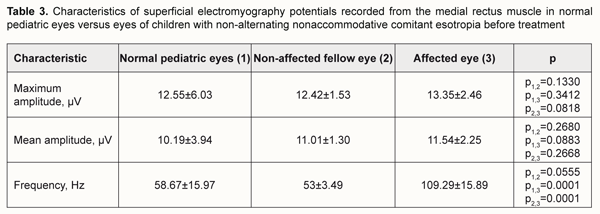
Results and discussion The data on the functional state of the horizontal extraocular muscles in the examined children before treatment is presented in the tables below. There were no significant differences in the mean amplitude and maximum amplitude of sEMG potentials between the esotropic eye and fellow eye in children with NNCES (Tables 2 and 3). In addition, the frequency of sEMG potentials was significantly higher in the esotropic eye than in the non-affected fellow eye (109.29 ± 15.89 Hz vs 53±3.49 Hz, р=0.0001) and in normal pediatric eyes (58.67±15.97 Hz, р=0.0001).
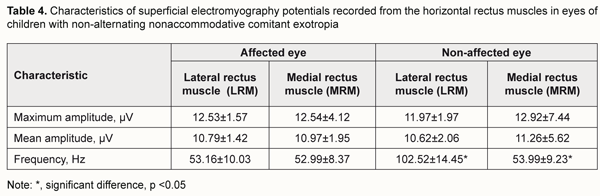
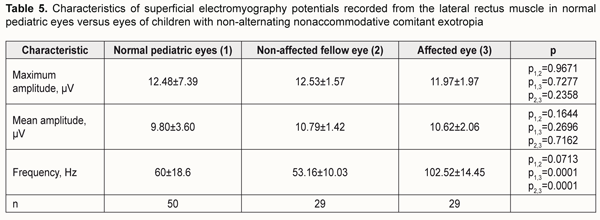
The characteristics of sEMG potentials recorded from the horizontal extraocular muscles in children with NNCEX are presented in Table 4. Mean amplitude and maximum amplitude of sEMG potentials of the LRM in the strabismic eye in these children were similar to those in the normal eyes of controls, with no significant differences (р > 0.05). In addition, frequency of sEMG potentials was significantly higher in the strabismic eye than in the fellow eye (102.52 ± 14.45 Hz vs 53.16±10.03 Hz, р=0.0001) and in normal pediatric eyes (60±18.6 Hz, р=0.0001).
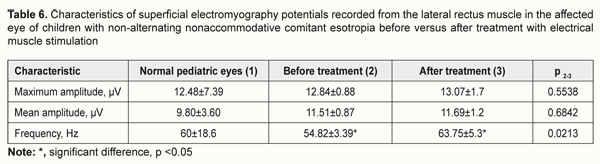
Pre-treatment and post-treatment changes in the electrical activity of the LRM of the strabismic eye in children with NNCES and presented in Table 6 and Figs. 1 and 2. The table shows that, after treatment, amplitudes of sEMG potentials from the LRM did not change (р > 0.05), but the frequencies statistically significantly increased (р < 0.05).
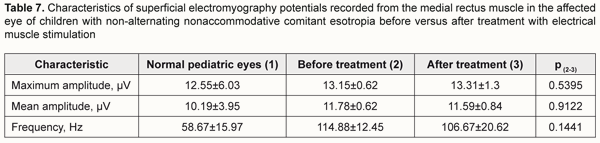
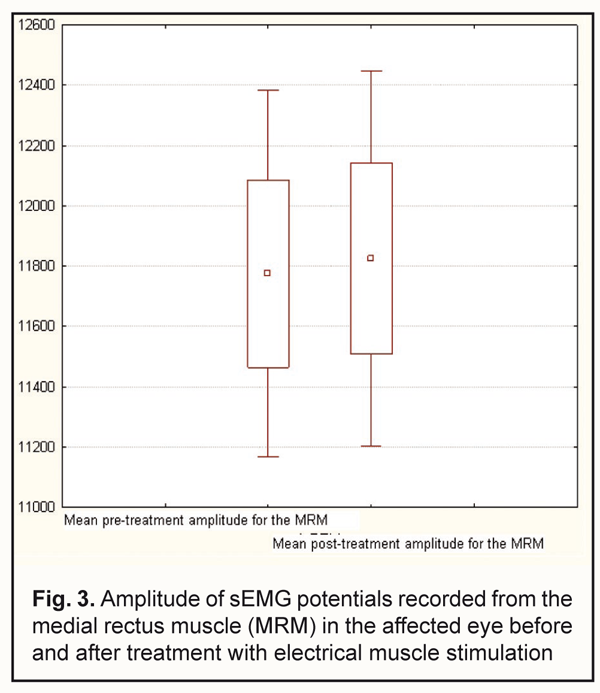
Pre-treatment and post-treatment changes in the electrical activity of the MRM of the strabismic eye in children with NNCEX are presented in Table 7 and Figs. 3 and 4. The table shows that amplitudes of sEMG potentials from the MRM did not change (р > 0.05), whereas the frequency decreased, alrhough not significantly (р >0.05), and became more normal after treatment.
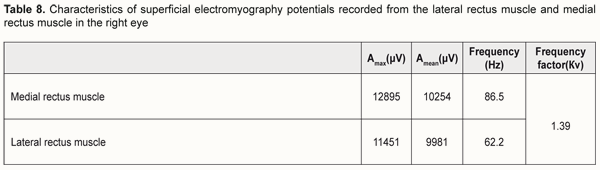
We examined the outcomes of treating the patients with electrical stimulation, and noted that this treatment failed to improve the strabismus in some cases. Thereafter, we examined the electric potentials of the oculomotor muscles in these cases in detail, and noted an improvement in the imbalance between antagonists muscle groups. That is why we considered a ratio of the frequency of the electrical activity from the LRM to that from the MRM in all esotropic patients before treatment, and called this ratio the “frequency factor”, Кν. We found that the electrical simulation treatment in esotropic patients with Кν> 1.5 did improve the strabismic deviation, whereas in those with Кν< 1.5, did not. The frequency factor, Кν, calculated after the sEMG examination of the horizontal extraocular muscles, allows establishing whether the electrical simulation treatment is indicated, and predicting whether the treatment will be effective for a particular patient. Example case 1: Patient B. aged 12 years and diagnosed with nonaccommodative comitant esotropia, high hypermetropia, and high refractive amblyopia in his right eye Pertinent clinical findings at baseline: Uncorrected visual acuity measured 0.06 OD and 1.0 OS. Best-corrected visual acuity measured 0.1 OD. The patient was highly hyperopic with spherical correction of +7.00 OD. Refractive error measured +10.00 sph OD and the left eye was emmetropic. There was esotropia of the right eye of +10 prism diopters (PD) without correction and +10 PD with correction. He had monocular vision. Кν=νLRM / νMEM = 86.5/62.2=1.39 Pertinent clinical findings after treatment with electrical stimulation: Uncorrected visual acuity measured 0.07 OD and 1.0 OS. Best-corrected visual acuity measured 0.1 OD. The patient was highly hyperopic with spherical correction of +7.00 OD. Refractive error measured +10.00 sph OD and the left eye was emmetropic. There was esotropia of the right eye of +10 PD without correction and +10 PD with correction. He had monocular vision. We concluded that since the frequency factor, Кν, for the strabismic eye (i.e., the right eye) was 1.39 < 1.5, the electrical simulation treatment was ineffective and resulted in no decrease in strabismus angle. Conclusion First, frequencies of electrical potentials recorded from the LRM of the affected eye in NNCES, and those recorded from the MRM for the affected eye in NNCEX, differed from those for normal pediatric eyes (109.29 ± 15.89 Hz vs 58.67±15.97 Hz, and 102.52 ± 14.45 Hz vs 60 ± 18.6 Hz, respectively). Second, in children with NNCS, we found changes in the characteristics of electrical activity of the horizontal rectus muscles after a course of electrical stimulation, with an improvement in the imbalance between the sEMG potentials for the LRM and MRM. Third, we calculated the frequency factor, Кν, as a ratio of the frequency of the sEMG potentials of the LRM to that of the MRM (Кν = νLRM / νMEM) for the esotropic patient, or as a vice versa ratio (Кν = νMEM / νLRM) for the exotropic patient before treatment. Finally, based on the frequency factor, Кν, calculated after the sEMG examination of the horizontal extraocular muscles, one can establish whether electrical simulation treatment is indicated, and predict whether this treatment will be effective for a particular patient. References 1.Andriienko AA. [Electrical stimulation of extraocular muscles as a component in the comprehensive management of strabismus]. Vrach Delo. 1975;11:103-5. Russian 2.Boichuk IM, Mazur VP. [A new method of surface electromyography of direct eye muscles in children]. Oftalmol. Zh. 2014;3:15-18. Russian 3.Information Bulletin No. 13, based on Pat. of Ukraine №91,463 issued 10.07.2014. [Device for transconjunctival superficial electromyography of extraocular muscles]. Authors: Boichuk IM, Mazur VP. Patent Holder: State Institution Filatov Institute of Eye Diseases and Tissue Therapy, NAMS of Ukraine. Ukrainian 4.Sosin IN, Buiavykh AG. [Physical therapy for ocular disorders: a guide for practitioners]. Simferopol: Tavriia; 1998. Russian 5.Cherikchi LE. [Physical therapy in ophthalmology]. Kyiv: Zdorov’ia; 1979. Russian 6.Yurov SI. [Treatment of comitant esotropia with electrical stimulation of the lateral rectus muscles]. Oftalmol Zh. 1968;8: 597-601. Russian 7.Sasaki T, Suzuki K, Matsumoto M et al. Origins of surface potentials evoked by electrical stimulation of oculomotor nerves: are they related to electrooculographic or electromyographic events? J Neurosurgery. 2002 Oct;97(4):941-4
|