J.ophthalmol.(Ukraine).2018;3:68-73.
|
https://doi.org/10.31288/oftalmolzh201836873 Value of static automated perimetry in assessing visual impairments in patients with pituitary adenoma with suprasellar extension K.S. Iegorova, Cand Sc (Med), M.O. Guk, Dr Sc (Med), L.V. Zadoianyi, Cand Sc (Med), O.M. Guk, Cand Sc (Med) Romodanov Neurosurgery Institute; Kyiv (Ukraine) E-mail: iegorova_katya@ukr.net TO CITE THIS ARTICLE: Iegorova KS, Guk MO, Zadoianyi LV, Guk OM. Value of static automated perimetry in assessing visual impairments in patients with pituitary adenoma with suprasellar extension. J.ophthalmol.(Ukraine).2018;3:68-73. https://doi.org/10.31288/oftalmolzh201836873
Background: Pituitary adenoma (PA) is a neoplasm that develops from anterior pituitary cells and accounts for 20-25% of all intracranial extracerebral tumors. In a functioning PA, a specific clinical syndrome develops, and, therefore, the diagnosis can be made early, when the tumor is small. In a non-functioning PA, the early stage is often asymptomatic and the disease is usually diagnosed only with the onset of visual impairment, with 3.5% to 16% of patients having blindness as an outcome. Purpose: To investigate changes in the visual field in pituitary adenomas with suprasellar extension and various anatomical positions of the optic chiasm. Materials and Methods: Ninety-six (100%) patients with a non-invasive PA with suprasellar extension were under surveillance at the Romodanov Neurosurgery Institute between 2015 and 2016, and underwent clinical neurological and ophthalmological examination and comprehensive neuroimaging evaluation. Inclusion criteria were a history of surgical procedure for a non-invasive PA with suprasellar extension, and visual impairment. Results and Discussion: Of the 96 patients, 50 (52%) had visual impairment, and were included in the analysis. Bitemporal visual field changes and homonymous hemianopia were found in 48 (96%) patients and 2 (4%) patients, respectively. Symmetric, asymmetric or markedly asymmetric chiasmal syndrome was found in 32 (67%), 11 (23%), and 5 (10%) patients, respectively. Of the 50 patients, 8 (16%) had a prefixed chiasm, and 3 (6%; patients with a bitemporal constriction of the visual fields) had a postfixed chiasm. Patients with pituitary adenoma may have a delayed onset of or no visual impairment due to the presence of a prefixed or postfixed chiasm. Conclusion: Static automated perimetry (SAP) is a sensitive and objective technique for detecting visual field defects in patients with PA with suprasellar extension. The SAP demonstrated characteristic visual field changes in temporal halves, with a degree of visual field loss ranging from mean deviation −1.26 to −19.31 dB. Keywords: pituitary adenoma, positions of the chiasm, automated static perimetry
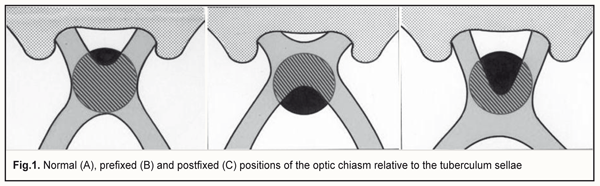
Introduction Pituitary adenoma (PA) is a neoplasm that develops from anterior pituitary cells and accounts for 20-25% of all intracranial extracerebral tumors. Pituitary adenomas are classified as functioning and non-functioning (NFPA), according to the presence or absence, respectively, of pituitary hormone hypersecretion, with NFPA accounting for 35-45% of all cases. In a functioning pituitary adenoma, a specific clinical syndrome develops, and, therefore, the diagnosis can be made early, when the tumor is small [1-3]. In a NFPA, the early stage is often asymptomatic and the disease is usually diagnosed only with the onset of visual impairment, with 3.5% to 16% of patients having blindness as an outcome [4, 5]. A PA can achieve large or even giant dimensions, which makes surgical treatment extremely difficult. Among functioning pituitary adenomas, this is related only to prolactin-secreting adenoma in elderly (non child-bearing age) patients. In a cohort study conducted in northern Finland, the annual incidence of PA increased from 3.8 cases per 100,000 population during 1992–1999 to 4.2 cases per 100,000 population during 2000–2007. In addition, in a study conducted in Iceland, the annual incidence increased from 0.6 cases per 100,000 population during 1955–1972 to 5.8 cases per 100,000 population during 2003–2012. Since the annual incidence of PA has been estimated as 2.5-3 per million in Ukraine, and most patients with PA are of young or middle working age, PA diagnosis and management issues have become especially socially important in this country [2, 3, 6]. Visual impairment due to a PA is associated with the compression of the anterior visual pathway that comprises the optic nerves, chiasm, and optic tracts. Because the anatomy of the anterior visual pathway is specific, atypical changes in the visual field occur in a PA with suprasellar extension. It has been reported that 40-65% of patients with PA have visual disturbance. Specifically, reduced visual acuity and visual field impairment have been found in 38-68.5% and 68-70%, respectively, of patients with PA. 30-62% of patients with PA manifest visual impairment [7-9]. The topographic relationship of the chiasm and sella turcica is important for emergence of visual impairment, and depends on the length of the intracranial portion of the optic nerve. The chiasm with a normal position (80% of the population) overlies the diaphragma sellae. When the chiasm is prefixed, the optic nerves are short, and the chiasm sits over the sella (15% of the population). When the chiasm is postfixed (5% of the population), the optic nerves are long, the chiasm sits posteriorly over the sella [10-12] (Fig. 1).
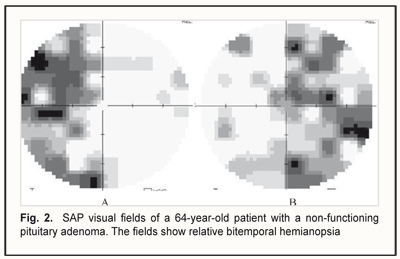
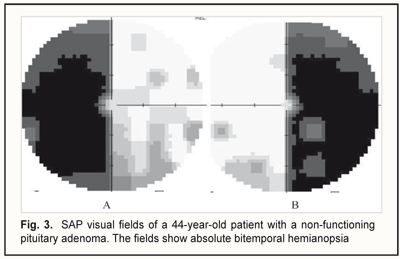
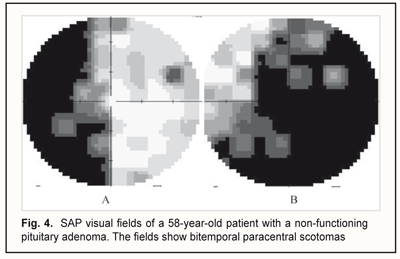
Direct chiasmal compression by a neoplasm results in visual impairments that are more typical for macroadenoma. Visual function impairment emerges at the “ophthalmic stage” of PA development and represents a chiasmal syndrome characterized by reduced visual acuity, specific visual field impairment, and development of descending primary atrophy of the optic nerve. The purpose of the study was to investigate a component of the chiasmal syndrome (specifically, changes in the visual field) in non-invasive pituitary adenomas with suprasellar extension and various anatomical positions of the optic chiasm. Materials and Methods Ninety-six (100%) patients (age, 14 to 74 years; mean age, 51±0.8 years; 52 (54%) women and 44 (46%) men) with a non-invasive PA with suprasellar extension were under surveillance at the Romodanov Neurosurgery Institute between 2015 and 2016, and underwent clinical neurological and ophthalmological examination and comprehensive neuroimaging evaluation. Inclusion criteria were a history of surgical procedure for a non-invasive PA with suprasellar extension, and reduced visual acuity and/or or visual field impairment. Neuroimaging procedures (sella turcica X-ray study, magnetic resonance imaging (MRI), and computer tomography (CT)) were performed to identify initially whether optic chiasm was prefixed, normofixed or postfixed. The final identification was performed during the surgical procedure. Ophthalmological examination included visual acuity assessment, biomicroscopy, kinetic and static perimetry, and direct and indirect ophthalmoscopy. Static automated perimetry (SAP) was performed with the Centerfield 2 Perimeter (Oculus, Wetzlar, Germany) using the neurological 30-2 threshold test program and Neuro screening program. Aside from defect localization, the arithmetic mean of the sensitivity loss, the mean defect (MD), was used to assess visual field severity. It represents the average visual field loss of a patient based on the difference between the mean sensitivity actually measured and the average normal sensitivity tested. Visual field loss severity was classified as “no visual field loss” (Grade 0; normal visual field), mild visual field loss (Grade 1; MD, –2 dB to –4 dB), moderate visual field loss (Grade 2; MD, –4 dB to –12 dB), severe visual field loss (Grade 3; MD, –12 dB to –20 dB), and very severe visual field loss (Grade 4; MD, worse than –20 dB). A chiasmal syndrome was considered symmetric if both eyes had the same grade of visual field loss. In addition, a chiasmal syndrome was considered asymmetric if the difference between eyes in grade of visual field loss severity was 1, and it was considered markedly asymmetric if the difference was 2 or greater. Results and Discussion Of the 96 patients with history of surgical procedure for a non-invasive PA growing upwards out of the pituitary fossa, 50 (52%) had reduced visual acuity and/or visual field impairment, and were included for the analysis. Reduced visual acuity in one or two eyes was found in 43 patients. Thirty-six patients had best-corrected visual acuity (BCVA) worse than 1.0 in both eyes; seven had BCVA of 1.0 in one eye and worse than 1.0 in the fellow eye; three had BCVA worse than 1.0 in one eye and worse than 0.1 in the fellow eye; two had BCVA worse than 0.1 in both eyes; one had BCVA worse than 0.1 in one eye and light perception in the fellow eye. Bitemporal visual field changes and homonymous hemianopia were found in 48 (96%) patients and 2 (4%) patients, respectively. Symmetric, asymmetric or markedly asymmetric chiasmal syndrome was found in 32 (67%) patients, 11 (23%) patients, and 5 (10%), respectively. Figures 2 to 4 present the SAP visual fields in patients with some versions of a symmetric chiasmal syndrome. Of the 32 patients with a symmetric chiasmal syndrome, complete and absolute bitemporal hemianopsia was observed in 10 (31%) patients, was characterized by a complete loss of vision in the temporal half of each visual hemifield both for white and colors, and was associated with a total injury to all crossed nerve fibers. In addition, 10 (31%) patients had relative bitemporal hemianopsia that was associated with a partial injury to crossed nerve fibers, and 3 (9%) had a bitemporal constriction of the visual fields which occurred in an injury to a portion of crossed nerve fibers in the anterior chiasm. Furthermore, relative superior quadrant bitemporal hemianopsia was detected in 4 (13%) patients. Moreover, 4 (13%) patients had bitemporal paracentral scotomas that occurred in an injury to crossed papillomacular fibers in the posterior chiasm. Finally, one (3%) patient demonstrated residual visual field in the nasal inner quadrant, with binocular loss of central vision.
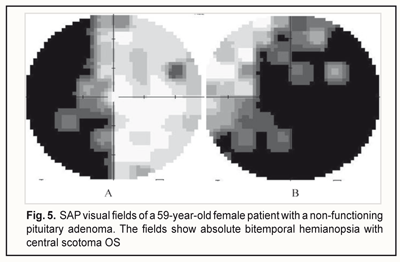
Of the eleven patients with an asymmetric chiasmal syndrome, 5 (45%) had complete and absolute bitemporal hemianopsia with a monocular central scotoma, 4 (37%) had relative bitemporal hemianopsia with a monocular central scotoma, and 2 (18%) had bitemporal paracentral scotoma with monocular relative temporal hemianopsia (Fig. 5). Examination of visual fields and perimetry demonstrated complete and absolute bitemporal hemianopsia with a monocular central scotoma in 5 (45%), relative bitemporal hemianopsia with a monocular central scotoma in 45 (37%), and bitemporal paracentral scotoma with relative temporal hemianopsia in 2 (18%) of these 11 patients (Fig. 5) on visual field examination.
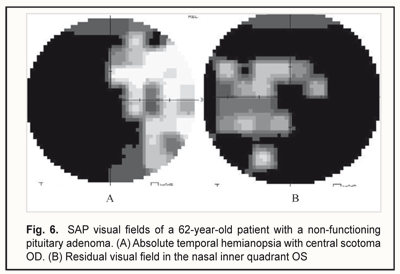
Of the five patients with a marked asymmetric chiasmal syndrome, 2 had complete and absolute temporal hemianopsia with a combination of a central scotoma in one eye and relative temporal hemianopsia in the other; 2 had relative temporal hemianopsia in one eye with a central scotoma in the other; and 1 had complete and absolute temporal hemianopsia with a central scotoma in one eye and residual visual field in the nasal inner quadrant in the fellow eye (Fig. 6) on visual field examination.
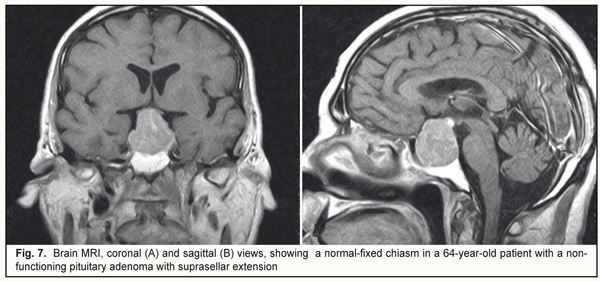
No loss of sensitivity to light was seen in 2 (2%) eyes. Loss of sensitivity to light was classified as mild in 25 (25%) eyes, moderate in 45 (45%) eyes, and severe and very severe in 21 (21%) eyes. The loss was bilateral in 6 (12%) patients. Symmetric chiasmal syndrome was the most common chiasmal syndrome (67%) in our patients with pituitary adenoma with suprasellar extension; this involved reduced visual acuity with symmetric injury to the temporal halves of the visual field secondary to an injury to crossed optic nerve fibers (Fig. 7).
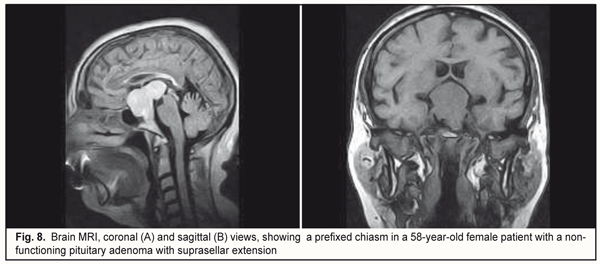
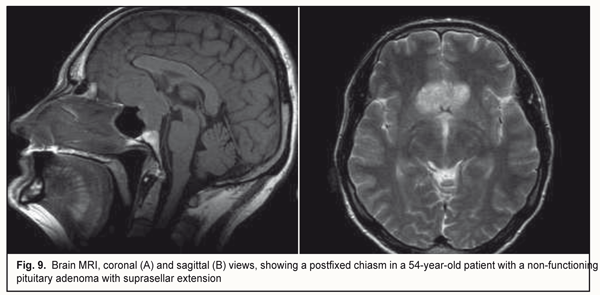
Of the 50 patients with reduced visual acuity and/or or visual field impairment, the hiasm was prefixed in 8 (16%) patients, specifically, in 4 patients with a bitemporal paracentral scotoma, 2 patients with homonymous hemianopia, and 2 patients with a markedly asymmetric visual field (Fig. 8). In addition, the hiasm was postfixed in 3 (6%) patients with a bitemporal constriction of the visual fields (Fig. 9).
Patients with pituitary adenoma may have a delayed onset of or no visual impairment due to the presence of a prefixed or postfixed chiasm. Conclusion Static automated perimetry is a sensitive and objective technique for detecting visual field defects in patients with pituitary adenoma with suprasellar extension. Visual field examination is of special value in the topical diagnosis of an injury to the visual pathway, and enables the clinician to determine visual field margins, the degree of sensitivity loss, and the extent of damage to the visual system. The static automated perimetry demonstrated characteristic visual field changes in temporal halves, with a degree of visual field loss ranging from mean deviation −1.26 to −19.31 dB. References 1.Abouaf L, Vighetto A, Lebas M. Neuro-ophthalmologic exploration in non-functioning pituitary adenoma. Ann Endocrinol (Paris). 2015 Jul;76(3):210-9 2.Rivoal O, Brézin AP, Feldman-Billard S, Luton JP. Goldmann perimetry in acromegaly: a survey of 307 cases from 1951 through 1996. Ophthalmology. 2000 May;107(5):991-7. 3.Guk MO. [Diagnosis and treatment of non-functioning pituitary adenomas]. [Dr Sc (Med) dissertation]. Kyiv: Romodanov Neurosurgery Institute; 2017. 328 p. Ukrainian 4.Nishimura M, Kurimoto T, Yamagata Y, et al. Giant pituitary adenoma manifesting as homonymous hemianopia. Jpn J Ophthalmol. 2007 Mar-Apr;51(2):151-3. 5.Kitthaweesin K, Ployprasith C. Ocular manifestations of suprasellar tumors. J Med Assoc Thai. 2008;91(5):711–5. 6.Halle AA, Drewry RD, Robertson JT. Ocular manifestations of pituitary adenomas. South Med J. 1983 Jun;76(6):732-5 7.Lee IH, Miller NR, Zan E, et al. Visual Defects in Patients With Pituitary Adenomas: The Myth of Bitemporal Hemianopsia. AJR Am J Roentgenol. 2015 Nov;205(5):W512-8 8.Kan E, Kan EK, Atmaca A, et al. Visual field defects in 23 acromegalic patients. Int Ophthalmol. 2013 Oct;33(5):521-5. 9.Ogra S, Nichols AD, Stylli S, et al. Visual acuity and pattern of visual field loss at presentation in pituitary adenoma. J Clin Neurosci. 2014 May;21(5):735-40. 10.Schiefer U, Isbert M, Mikolaschek E, et al. Graefes Arch Clin Exp Ophthalmol. 2004 Jun;242(6):468-77. 11.Serova NK. [Clinical neuro-ophthalmology: Neurosurgical aspects]. Tver: Triada LLC; 2011. Russian 12.EZh Tron. [Visual pathway disorders]. Moscow: Medgiz; 1955. Russian
|