J.ophthalmol.(Ukraine).2018;2:41-44.
|
https://doi.org/10.31288/oftalmolzh/2018/2/4144 Histomorphologic changes after contact transscleral Nd: YAG laser cyclophotocoagulation with scleral compression P. P. Chechin, Cand. Med. Sc.; V. V. Vit, Dr. Med. Sc., Prof.; O. V. Guzun, Cand. Med. Sc. SI “Filatov Institute of Eye Diseases and Tissue Therapy of NAMS of Ukraine”; Odessa (Ukraine) E-mail: olga.v.guzun@gmail.com TO CITE THIS ARTICLE: Chechin PP, Vit VV, Guzun OV. Histomorphologic changes after contact transscleral Nd: YAG laser cyclophotocoagulation with scleral compression. J.ophthalmol.(Ukraine).2018;2:41-4. https://doi.org/10.31288/oftalmolzh/2018/2/4144
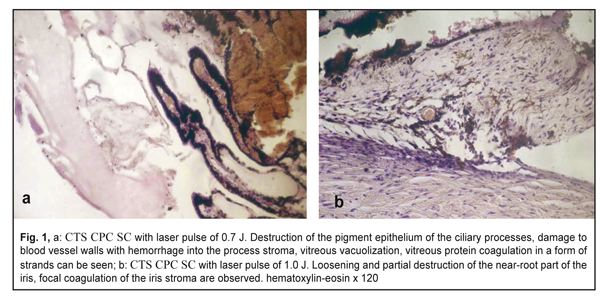
Introduction. Refractive glaucoma is referred to the most severe forms of the disease. To reduce intraocular pressure and pain syndrome, transscleral laser photocoagulation of the ciliary body is currently used. Puprose. To determine in experiment morphological changes in the sclera and ciliary body after contact transscleral cyclophotocoagulation (CTS CPC) with scleral compression (SC) using infrared Nd: YAG laser radiation. Material and Methods. Experimental studies involved two rabbits (4 eyes). Nd: YAG laser (λ=1.06 µm) was adapted to a 600 µm fiberoptic crystal probe and used for laser photocoagulation. Laser pulse was 0.7- 1.2 J; laser pulse length was 3 ms. After topical anesthesia with proxymetacaine hydrochloride (0.5%), CTS CPC SC was performed in superior and inferior eyeball quadrants, at 2-3 mm from the limbus in two rows in full circle (360°) with the sclera compressed by a 6 g endface for 5 seconds. Results. The histological studies at Day 1 after CTS CPC SC revealed damage to the pigment epithelium of the ciliary processes and their vessels when laser pulse parameters were low (0.7-1.0 J). High-energy CTS CPC SC of the ciliary body (1.1-1.2 J) damaged the sub-conjunctival tissue and sclera. With laser radiation, collagen stromal fiber separation and channeling were noted as result of a hydrodynamic shock which can supposedly lead to increased transscleral filtration. The mechanism of antihypertensive action of CTS CPC SC using Nd:YAG laser is likely to include two components: photocoagulation and hydrodynamic cavitation. Key words: transscleral cyclophotocoagulation, Nd: YAG laser, ciliary body, sclera, morphological changes Introduction Refractive glaucoma is referred to the most severe forms of the disease. A range of medications and surgeries which are currently used do not achieve the efficacy as desired: lowering intraocular pressure (IOP) and pain syndrome. Today, in a number of cases, laser photocoagulation (LP) of the ciliary body is considered to be effective and relatively safe treatment [1-7]. Currently, there is no consensus on the mechanism of antihypertensive action of transscleral LP of the ciliary body using different wave lengths of infra-red diapason (0.89; 1.06; 1,5 µm). Different authors have reported that the antihypertensive action can be associated with thermal destruction of ciliary processes, direct transscleral filtration, formation of a variety of biologically active agents (prostaglandin, prostacyclin), or reduction of vascular perfusion and ischemia development [3, 8]. The purpose of the present paper was to experimentally determine morphological changes occurring in the sclera and ciliary body after contact transscleral cyclophotocoagulation with scleral compression (CTS CPC SC) using infrared Nd:YAG laser radiation. Material and Methods Experimental studies were performed in two Black Velvet Chinchilla rabbits (4 eyes). Nd:YAG laser (λ=1.06 µm) was adapted to a 600 µm fiberoptic crystal probe and used for laser photocoagulation. Laser pulse was 0.7 to 1.2 J; laser pulse length was 3 ms. After topical anesthesia with proxymetacaine hydrochloride (0.5%), CTS CPC SC was performed in superior and inferior eyeball quadrants, at 2-3 mm from the limbus in two rows in full circle (360°) with the sclera compressed by a 6 g endface for 5 seconds. In right eyes, CTS CPC SC was performed with laser pulse of 0.7 J and 1.0 J in the superior and inferior quadrants, respectively. In left eyes, laser pulse was 1.2 J and 1.1 J in the superior and inferior quadrants, respectively. The animals were taken out of the experiment through air embolization at Day 1 and 3 after CTS CPC SC. Sites of laser radiation in the enucleated eyes of the experimental animals were studied histologically. The enucleated eyes were formalin fixated and cut in a forward/reverse direction from the limbus to ciliochoroidal junction. After being embedded in paraffin and prepared, sections were hematoxylin-eosin stained. Light microscope images were photorecorded using a digital camera. Results Principal changes in the ocular structures within laser radiation sites were destructive, the degree of which depended on a radiation power. The most pronounced changes were noted in the stroma and pigment epithelium of the iris and ciliary processes, i.e. in intensively pigmented structures. With laser pulse of 0.7 J, the changes were limited to destruction of ciliary process blood vessel walls and hemorrhage into the stroma. In addition, vacuolization and destruction were revealed in the vitreous, in the sites attached to the ciliary body (Fig. 1a).
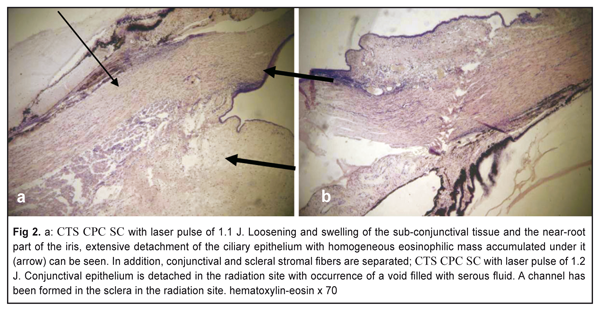
With laser pulse of 0.7 J, we noted detachment and destruction of an unpigmented layer of the ciliary body pigment epithelium, homogenization of the stroma, and destruction in the ciliary processes. A near-root part of the iris was swollen with the presence of necrotized cells and loosened stromal elements. A destruction of the iris pigment epithelium was also noted (Fig. 1b). With laser pulse of 1.1 J, ciliary stroma edema and focal edema of nonpigmented ciliary epithelium were detected. In addition, we noted a detachment of nonpigment epithelium, vacuole-like formations, and a homogeneous protein-containing accumulation between the ciliary processes and anterior chamber angle (Fig. 2a).
With laser pulse of 1.2 J, changes were also revealed in the sclera and conjunctiva. Herewith, voids filled in with serous fluid were noted in the subconjunctival tissue. With the laser radiation, we noted collagen stromal fibers with channel formation. The above changes were revealed at Day 1 after CC TS CPC. At Day 3 after CC TS CPC, specific features were the presence of inflammation and necrosis signs which were mainly common for the area of the sub-conjunctival tissue and superficial layers of the sclera. Conclusion The histological studies revealed that, at Day 1 after CTS CPC SC, there was variously pronounced damage to the pigment epithelium of the ciliary processes and their vessels when laser pulse parameters were low (0.7-1.0 J). High-energy CTS CPC SC of the ciliary body (1.1-1.2 J) damaged the sub-conjunctival tissue and sclera. With laser radiation, collagen stromal fiber separation and channeling were noted as result of a hydrodynamic shock which can supposedly lead to increased transscleral filtration. References
|